Diabetes
advertisement

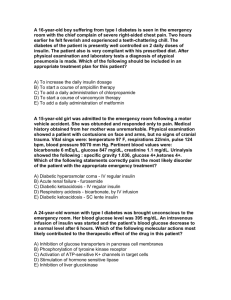
Diabetes 4-5% of the UK population has diabetes. 20-30% of them are treated with insulin. Pancreas produces 2 hormones that regulate blood glucose: insulin secreted when blood glucose levels rise after eating, and glucagon when blood glucose levels are low. Insulin encourages cells to take up glucose to be broken down for energy. Glucagon stimulates the conversion of glycogen stored in the liver to glucose to raise the level of glucose in the blood. Glucose is also made and stored by the liver which secretes glucose between meals and at night when we are asleep. Therefore, insulin is secreted at a low basal level throughout the day and night, and increases after meals. During exercise, the level of insulin secreted falls. Secretion in health is about 30-40 units daily. NB do not use the terms NIDDM or IDDM Type 1 Autoimmune disease where the beta cells that produce insulin are destroyed. Therefore the body fails to produce any insulin to control blood sugar. Usually occurs before the age of 40. Highest incidence around 11 – 12 years of age. Acute onset over a period of weeks or months. Need insulin injections for life. Type 2 Body does not produce enough insulin or it does not use it effectively. Linked to obesity. Higher risk in Afro-Caribbean’s, Southern Asians and people over 40. Need to change lifestyle, take tablets and eventually insulin injections. Diet should be low in animal fat, carbohydrates should be starchy and long lasting such as those found in bread, rice and potatoes. Most common tablets used are Metformin which increases the body’s sensitivity to insulin. Symptoms Thirst Excessive urine (polyuria) Tiredness Weight loss Muscle wasting Regular thrush Blurred vision Risks 1. Hypoglycaemia: low blood glucose. Insulin has moved too much glucose out the blood stream. Occurs when taken too much insulin, skipped a meal, during vigorous exercise, or excessive alcohol intake. The brain is totally reliant on the blood glucose for its energy so can cause headache, confusion, aggression, tremor, pallor, sweating can lead to loss of consciousness. Symptoms include sweating, shaking, weakness, hunger, nausea, tingling lips. Treatment – need something sugary e.g. glucogel. In cases of LOC need intramuscular injection of glucagon 1mg. Can also use IV glucose in LOC. 2. Hyperglycaemia: high blood glucose. Extreme thirst, dry mouth, blurred vision, drowsiness, excessive urine. Can lead to ketoacidosis – the breakdown of fat instead of glucose for energy because the insulin is not moving the glucose into the cells to be broken down for energy. Leads to increased acids in the blood. Complications Small capillaries are affected by raised glucose and this can result in eye disease (retinopathy), kidney disease (neuropathy), nerve conduction problems (peripheral neuropathy). Diagnosis Urine test There should not be any glucose present. Kidneys usually reabsorb glucose but in diabetics, blood glucose levels are much higher so the kidneys are unable to reabsorb all the glucose. If positive, pt will need a blood test Blood-Glucose (Do not use term BM) Normal range 4.3 – 7 mmol/l BG of 11.1 mmol/l or greater suggests diabetes. Should do an FBS to confirm. Elderly acceptable levels = 4-12. More important to prevent hypos, esp. if live alone. Younger adults acceptable levels = 4-8. More important to have tight control to prevent later complications. BG increases after eating. Target levels for type 1 diabetes 2 hours postprandial (after food) are ˂7.8 mmol/l Target levels for type 2 diabetes 2 hours postprandial are up to 9 mmol/l If BG greater than 15mmol/l, check urine for ketones. Check for patterns Fasting Blood Sugar No food or drink other than water for 8 hours. When fasting, glucagon is stimulated which causes the liver to convert stored glycogen into glucose to increase blood sugar level. In non-diabetics, this will stimulate insulin to move the increased glucose from the blood into cells to restore normal levels. In diabetics, insulin does not work effectively so blood glucose remains high. An FBS of 7.0 mmols or greater indicates diabetes. FBS used for diagnosis and to assess affects of medications. Hb A1C Oral medications Metformin = first line choice. Improves body’s response to insulin and prevents it from making too much sugar. (NB need to monitor kidney function, if creatinine greater than 150, worsening renal function indicated and need to stop metformin). Side effect of Metformin = diarrhoea. Usually stops in first two weeks. Acarbose – reduces rate that starchy and sugary foods absorbed into the body Glitazones e.g. rosiglitazone and pioglitazone. Help the body use its own insulin more effectively. Prandial glucose inhibitors eg repaglinide and nateglinide. Help the body to produce the right amount of insulin after meals. Tolbutamide Sulphonylureas e.g. glimeperide, gliclazide, glipizide, glibenclamide. Increase the amount of insulin made by the body. need access to a BG monitor due to risk of hypos. Insulin Genetically engineered – recombinant human insulin, but can also be engineered from pigs and cows. Most common errors are associated with prescribing and administration. Only give insulin in a syringe, pen or pump designed solely for insulin. Only give it if you have had specific training. Let the patient do their own insulin if they can. Check BNF, ask diabetes specialist or pharmacist if unsure. There are over 20 different insulin’s. They have a proprietary name e.g. Apidra® (must be stated when prescribed) and an approved name e.g. insulin glulisine. Insulin in the UK is made in one strength 100 units per ml (U100 insulin) Some pt’s use a concentrated 500 units per ml e.g. Humulin R – injected TDS before meals via an insulin pump. This has 5 x the glucose lowering effect and must be stored separately from other insulin’s. Not found in the BNF as it is not licensed in the UK. When prescribed the words ‘units’ should always be written in full. Insulin is categorised according to how fast it acts. Insulin has a short half life of 5-6 mins as it is rapidly destroyed by the liver. Therefore it is bound to zinc or proteins to overcome this and be released over a longer period of time (see chart). Regimens (number of daily injections) OD – long acting insulin, usually type 2, usually used in combination with an oral agent. BD – Fast acting and background insulin eg NovoMix 30 or Humulin M. Multiple (basal bolus therapy) 4-5 times per day. Mimic normal insulin release. Intermediate insulin OD and short/rapid acting with meals. Variable rate IV insulin infusions Given in hospital when patient not eating or drinking. Acute illness or surgery can lead to hyperglycaemia. NB soluble insulin given IV has a half life of 3-5 minutes. IV infusions must be diluted e.g. in sodium chloride. IV glucose must also be prescribed. IV insulin solution expires 24 hrs after preparation. Only discontinue infusion when pt can eat and drink again. Type 1 – must restart insulin regimen as soon as infusion ends. Discontinue IV insulin 30 mins after pt takes usual insulin/diabetic meds. Infusion is not recommended if pt is eating and drinking as makes it more difficult to maintain blood glucose levels. Routes of administration Available in: vials, cartridges for insulin pens, pre-loaded insulin pens, insulin pumps ( connected via a catheter under the skin in the abdomen, usually deliver steady small doses and bolus at mealtimes via short acting insulin). Injected at 90 degrees subcut. Common lengths of needle: 5mm, 6mm, 8mm. Dependent on build of patient. Absorbed fastest from the arm, slightly slower from the abdomen, and slowest from the leg. Use a wide area of the same site at the same time each day. Storage Unopened should be stored in fridge. Once opened, store at room temp. NB absorption of cold insulin differs from that of insulin at room temp. Do not store insulin pen with needle already attached. Do not predraw. Side effects of insulin Hypoglycaemia Most common. BM less than 4.0 mmols/l. 2 effects: 1. Adrenergic – adrenaline and glucagon cause rapid release of glucose from the liver. Fight or flight symptoms eg sweating, tremor, palpitations, tachy/brady, bounding pulse, nausea, anxiety. 2. Neuroglycopaenic – cerebral function impaired when plasma glucose less than 3.5 mmols. Symptoms: irrational behaviour, confusion, irritability, slurred speech, fitting, lethargy. Untreated – paralysis, hemiplegia, coma. Causes: too much diabetic med, vigorous exercise (exhausts muscle glycogen stores which take a day to replenish), not enough food esp. long lasting carbohydrates, too much alcohol/on an empty stomach, delayed/missed meal, drug interactions, lack of steroid, hypothyroidism, renal impairment, liver failure. Treatment – see chart. Skin problems Lipohypertrophy (production of fatty lumps stimulated by insulin) – if injection repeatedly given in same site. They do not have a normal supply of nerves or blood vessels so are not painful. Rotate injection site daily to avoid. Lipoatrophy – loss of fat under skins surface creating a dip with a firm texture. Now rare because insulins are highly purified. Small painful lumps that disappear within hours/days– from not injecting deep enough Weight gain Due to water retention. Fat and protein also no longer being broken down for energy as glucose is being moved into the cells effectively. Insulin also stimulates appetite. NB if pt BG low and insulin due, correct hypo first, re-check BG and if 4 or greater then still give insulin as takes a while to work so if do not give it, pts BG will rise later in the day and will take a long time to correct itself. Could cause delayed discharge. Therefore, do not ever not give insulin. Just make sure you correct any hypos first. Do not reuse needles. Leaving the needle on the pen can cause insulin to leak out or air to be drawn in, would could alter the amount/mixture of insulin received. Insulin could also crystallise in the needle between injections and create a blockage. Reuse could also bend the needle, creating microtrauma leading to lipodystrophy, painful injections and needle breakage. Sterility is also reduced. Diet If pt is on insulin, they must have carbs with every meal as carbs are turned into blood glucose for energy. Eating about the same amount of carb foods at the same time each day helps with BG control. Grains, fruits and vegetables provide fibre, vitamins and minerals. Whole grain breads, bran cereal and brown rice increase fibre. Use whole wheat and whole grain flour. Eat more fresh fruit and vegetables. Eat dark green leafy vegetables. Milk provides carbohydrates, protein and fat. Should have skimmed or semi skimmed. Meat provides protein. It should be lean e.g. cut fat off, avoid having sausages or bacon often, eat fish and poultry more often. Eggs and cheese are included in the meat group. Limit egg yolks to 3 per week and choose low fat cheeses. Eat a diet low in saturated fat and cholesterol. Use a cooking spray. Bake or grill meats. Choose low fat options. Sugar free options may still have a lot of carbohydrates so remember to include them in meal planning. Try to limit sugar as much as poss but a teaspoon of sugar on cereal or in tea is ok if the pt is insistent and will not accept sweetner as an alternative. Don’t recommend diabetic chocolate as it still affects the BG, causes loose stools and is expensive. Alcohol affects BG of patients on insulin. It can lower BG hours after it has been drunk. Alcopops are high in sugar so avoid them. Do not drink on an empty stomach. Sexual Health Sex is a form of exercise and can cause a hypo. Erection difficulties are common in men with diabetes. The pill may increase insulin requirements. BG should be stable for at least 3 months before trying for a baby. If either parent had diabetes, or there is a string family history of diabetes, then there is an increased risk the child will develop diabetes. Exercise Try to exercise 1-2 hours after a meal. Take a snack / sports drink before exercise and/or reduce insulin dose. Hypos can happen 6-15 hours after exercise. NB it takes up to 20 hours to replace carbohydrate. Don’t inject near the exercising muscle as the insulin will be absorbed very quickly. If blood sugar is mid teens or higher, check for ketones. If ketones are present, do not exercise. Other types of diabetes/causes of hyperglycaemia Steroids NB steroids cause insulin insensitivity meaning BM may increase. Therefore, pts on steroids should have OD BMs. If BM consistently greater than 11 and pt on steroids, need to inform doctor. Steroids usually taken in the morning, therefore, BG goes up by the afternoon when the steroid has started to take effect. Diabetics who normally take tablets may need insulin whilst they are on steroids. Infection Cause BG to rise Gestational diabetes During non-diabetic pregnancy, the body produces up to 3 times the normal amount of insulin to maintain normal BG levels. Impaired Glucose Tolerance (IGT) develops when the pancreas cannot produce enough insulin to maintain normal BG levels during pregnancy. IGT can normally be diet controlled. Gestational diabetes (GDM) - when BG levels are greater than 6 mmol/l before meals and greater than 8 mmol/l after food. Treated with insulin. Risk factors: over 40 y/o, obesity, family history, previous GDM, ethnic origin (indo-asian, afro-carribean, African, arab, Mediterranean, Hispanic), polycystic ovary syndrome. If have GDM, mother is at increased risk of developing type 2 diabetes later in life. Women with pre-existing insulin treated diabetes should reduce insulin immediately after birth. Women with type 1 diabetes are at greater risk of hypos in the post natal period, esp. if breast feeding. Should have a snack or meal available before or during feeds. Any damage to the pancreas e.g. cancer Driving and Employment By law, must tell DVLA if take insulin or tablets for diabetes. If diabetes is well controlled should be able to keep licence. If take insulin, will be given a restricted licence for 1,2 or 3 years which will need to be renewed. Tell your insurance company. When driving, check BG before you go, don’t drive if less than 5mmol/l. Stop for a snack every 2 hours. Employment – only industry which bans diabetes is the armed forces. Feet Diabetes affects the nerves and blood supply to the feet (neuropathy). Decreased sensation in feet. Narrowing of blood vessels in the legs making wounds/sores slow to heal. Pressure on an area on the foot can cause corns and calluses. The skin eventually breaks down and an ulcer forms. If left untreated, can lead to amputation. Need to check level of sensation and circulation in feet. Need to: check feet daily, keep feet clean, wear shoes that are the right size, avoid shoes/socks/tights with a pronounced seem around the foot, use a moisturiser (but not in between the toes as this could lead to athletes foot), avoid direct heat. Do not use razors, corn or verruca remedies. Diabetic Retinopathy High risk if blood glucose levels are high over a long period of time. Blisters develop on the small blood vessels in the retina which can burst and bleed. Can cause yellowish-white patches in the retina. Body tries to make new blood vessels, but they are weak and break and bleed easily. Symptoms: reduced vision, loss of sight. Need a diabetic eye check yearly. Laser treatment (photocoagulation) used to seal off leaky blood vessels and prevent eye sight from getting worse. Glaucoma Drainage problems in the eye leading to an increase in pressure within the eyeball. Can lead to blindness. Cataracts More common in diabetics and have an earlier onset – middle age. High blood glucose for a prolonged period causes glucose to build up on the lense making it cloudy so that less light can pass into the eye. NB having high blood glucose can make your body dehydrated. When start treatment for diabetes, BG will fall and dehydration will be reversed. Fluid level in eye increases resulting in blurred vision which can last for up to 3 months. Think Glucose National Campaign Winchester focussing on: referrals, timing meals and insulin, feet (doctors must foot stamp notes within 4 hours of admission), coding (stamp). Sources of Information BNF Monthly Index of Medical Specialities www.mims.co.uk DAFFNE Winchester Hospital Diabetic Team Endocrinology consultants - Dr Chong and Dr Norris Diabetic Nurse Specialist – Kate Mon: ward round Tues: ante-natal clinic Wed: diabetic foot ulcer clinic Thurs: ward round, pump clinic, endocrine testing Community diabetes nurse is based in Lyndhurst but has clinics all over Hampshire. If a pt is having problems in the community e.g. practice nurse cannot resolve a foot ulcer, can refer to consultants clinic at the hospital. Ward can refer to community diabetes nurse if patient is being discharged and has not been seen by diabetic nurse e.g. at the weekend.