2B 13 UNIT 3 Quiz2
advertisement

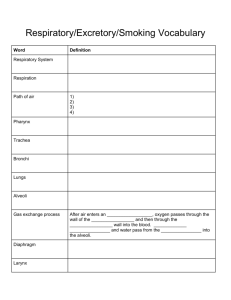
Quiz Urinary System 1. The kidneys help regulate blood volume. help control blood pressure. help control pH. All of the above are correct. 2. The location of the kidneys in relationship to the peritoneal lining of the abdominal cavity is referre to as retroperitoneal. retroabdominal. posterior. dorsal. 3. All of the following belong to the urinary system EXCEPT the urethra. ureter. bladder. prostate. 4. The functional unit of the kidney is called a glomerulus. nephron. corpuscle. calyx. 5. Most glucose molecules are reabsorbed in the proximal convoluted tubules. distal convoluted tubules. collecting ducts. loop of Henle. 6. Which of the following substances can be eliminated from the blood by tubular secretions? potassium ions hydrogen ions ammonium ions All of the above. 7. The structure that connects a kidney to the urinary bladder is the ureter. urethra. renal pelvis. collecting duct. 8. Urine is expelled from the urinary bladder by excretion. defecation. micturition. filtration. 9. All the following are principle solutes of urine EXCEPT urea. creatinine. glycogen. uric acid. 10. Which of the following hormones increase reabsorption of water in the collecting ducts? renin. ADH. aldosterone. insulin. Quiz Respiratory System 11. The exchange of gases between blood and cells is called pulmonary ventilation. internal respiration. external repiration. cellular respiration. 12. Which of the following does NOT belong to the conducting prtion of the respiratory system? alveoli bronchioles nose pharynx 13. The structure which closes off the larynx is the glottis. Adam's apple. epiglottis. vocal cords. 14. Which of the following describes a correct order of structures in the respiratory passeways? pharynx, trachea, larynx, bronchi, bronchioles larynx, pharynx, trachea, bronchiles, bronchi trachea, pharynx, larynx, bronchi, bronchioles pharynx, larynx, trachea, bronchi, bronchioles 15. The exchange of gases occurs in the trachea. bronchioles. alveoli. bronchus. 16. The volume of air that can be exhaled after normal exhaltation is the tidal volume. residual volume. inspiratory reserve volume. expiratory reserve volume. 17. The volume of air in a normal breath is called total lung capacity. vital capacity. tidal volume. residual volume. 18. Gas exchange in the lungs happens by the process of osmosis. diffusion. exocytosis. active transport. 19. Most oxygen in the blood is transported as gas dissolved in plasma. as oxyhemoglobin. as carboxyhemoglobin. as bicarbonate. 20. The primary chemical stimulus for breathing is the concentration of carbon monoxide in the blood. carbon dioxide in the blood. oxygen in the blood. carbonic acid in the blood. 21. What are the contents and percentages of the indicated portions of the hematocrit below? A. B. 22. List the normal number range for each leukocyte (A-E) below and give the primary reason that each would be elevated. A B C D E 23. Completely label each identified component for all of the images that are below: 24. Completely label each identified component for all of the images that are below: 25. Completely label each identified component for all of the images that are below: 26. Completely label each identified component for all of the images that are below: 27. Completely label each unidentified component for all of the images that are below: 28. Completely label each unidentified component for all of the images that are below: 29. Identify the specific blood type seen below : Functional Anatomy of the Respiratory System 1. The nasal cavity, the chamber within the nose, is divided medially by a nasal septum and separated from the oral cavity by the palate (Figure 13.1). The nasal cavity is lined with a mucosa, which warms, filters, and moistens incoming air. The mucosa also contains receptors for sense of smell. Paranasal sinuses and nasolacrimal ducts drain into the nasal cavity. 2. The pharynx (throat) is a mucosa-lined, muscular tube with three regions nasopharynx, oropharynx, and laryngopharynx. The nasopharynx functions in respiration only; the others serve both respiratory and digestive functions. The pharynx contains tonsils, which act as part of the body's defense system. 3. The larynx (voice box) is a cartilage structure; most prominent is the thyroid cartilage (Adam's apple). The larynx connects the pharynx with the trachea below. The laryngeal opening (glottis) is hooded by the epiglottis, which prevents entry of food or drink into respiratory passages when swallowing. The larynx contains the true vocal cords, which produce sounds used in speech. 4. The trachea (windpipe) extends from larynx to primary bronchi. The trachea is a smooth muscle tube lined with a ciliated mucosa and reinforced with C-shaped cartilage rings, which keep the trachea open. 5. Right and left primary bronchi result from subdivision of the trachea. Each plunges into the hilus of the lung on its side. 6. The lungs are paired organs flanking the mediastinum in the thoracic cavity. The lungs are covered with visceral pleura; the thorax wall is lined with parietal pleura. Pleural secretions decrease friction during breathing. The lungs are primarily elastic tissue, plus passageways of the respiratory tree. The smallest passageways end in clusters of alveoli. 7. The conducting zone includes all respiratory passages from the nasal cavity to the terminal bronchioles; they conduct air to and from the lungs. Respiratory bronchioles, alveolar ducts and sacs, and alveoli which have thin walls through which gas exchanges are made with pulmonary capillary blood are respiratory zone structures (Figure 13.2). Return to top Respiratory Physiology 1. Mechanics of breathing: Gas travels from high-pressure to low-pressure areas. Pressure outside the body is atmospheric pressure; pressure inside the lungs is intrapulmonary pressure; pressure in the intrapleural space is 2. 3. 4. 5. 6. intrapleural pressure (which is always negative). Movement of air into and out of the lungs is called pulmonary ventilation, or breathing (Figure 13.3). When inspiratory muscles contract, intrapulmonary volume increases, its pressure decreases, and air rushes in (inspiration). When inspiratory muscles relax, the lungs recoil and air rushes out (expiration). Expansion of the lungs is helped by cohesion between pleurae and by the presence of surfactant in alveoli. Nonrespiratory air movements: Nonrespiratory air movements are voluntary or reflex activities that move air into or out of the lungs. These include coughing, sneezing, laughing, crying, hiccupping, yawning. Respiratory volumes and capacities: Air volumes exchanged during breathing are tidal volume, inspiratory reserve volume, expiratory reserve volume, and vital capacity (Figure 13.4). Residual volume is nonexchangeable respiratory volume and allows gas exchange to go on continually. Respiratory sounds: Bronchial sounds are sounds of air passing through large respiratory passageways. Vesicular breathing sounds occur as air fills alveoli. External respiration, gas transport, and internal respiration: Gases move according to laws of diffusion (Figure 13.5). Oxygen moves from alveolar air into pulmonary blood. Most oxygen is transported bound to hemoglobin inside RBCs. Carbon dioxide moves from pulmonary blood into alveolar air. Most carbon dioxide is transported as bicarbonate ion in plasma. At body tissues, oxygen moves from blood to the tissues, whereas carbon dioxide moves from the tissues to blood. Control of respiration a. Nervous control: Neural centers for control of respiratory rhythm are in the medulla and pons. Reflex arcs initiated by stretch receptors in the lungs also play a role in respiration by notifying neural centers of excessive over inflation. b. Physical factors: Increased body temperature, exercise, speech, singing, and nonrespiratory air movements modify both rate and depth of breathing. c. Volition: To a degree, breathing may be consciously controlled if it does not interfere with homeostasis. d. Emotional factors: Some emotional stimuli can modify breathing. Examples are fear, anger, and excitement. e. Chemical factors: Changes in blood levels of carbon dioxide are the most important stimuli affecting respiratory rhythm and depth. Carbon dioxide acts directly on the medulla via its effect on reducing blood pH. Rising levels of carbon dioxide in blood result in faster, deeper breathing; falling levels lead to shallow, slow breathing. Hyperventilation may result in apnea and dizziness, due to alkalosis. Oxygen is less important as a respiratory stimulus in normal, healthy people, but it is the stimulus for those whose systems have become accustomed to high levels of carbon dioxide. Return to top Respiratory Disorders 1. The major respiratory disorders are emphysema, chronic bronchitis, and lung cancer. A significant cause is cigarette smoking. 2. Emphysema is characterized by permanent enlargement and destruction of alveoli. The lungs lose their elasticity, and expiration becomes an active process. 3. Chronic bronchitis is characterized by excessive mucus production and its pooling in lower respiratory passageways, which severely impairs ventilation and gas exchange. Patients may become cyanotic as a result of chronic hypoxia. 4. Lung cancer is extremely aggressive and metastasizes rapidly. The three most common lung cancers are squamous cell carcinoma, adenocarcinoma, and small cell carcinoma. Return to top Developmental Aspects of the Respiratory System 1. Premature infants have problems keeping their lungs inflated due to lack of surfactant in their alveoli. (Surfactant is formed late in pregnancy.) 2. The most important birth defects of the respiratory system are cleft palate and cystic fibrosis. 3. The lungs continue to mature until young adulthood. 4. During youth and middle age, most respiratory system problems are a result of external factors, such as infections and substances that physically block respiratory passageways. 5. In old age, the thorax becomes more rigid and lungs become less elastic, leading to decreased vital capacity. Protective mechanisms of the respiratory system decrease in effectiveness in elderly persons, predisposing them to more respiratory tract infections. Return to top Urinary System Kidneys Ureters, Urinary Bladder, and Urethra Developmental Aspects of the Urinary System Kidneys 1. The paired kidneys are retroperitoneal in the superior lumbar region. Each kidney has a medial indentation (hilus), where the renal artery, renal vein (Figure 15.1). And ureters are seen. Each kidney is enclosed in a tough fibrous capsule. A fatty cushion holds the kidneys against the trunk wall. 2. A longitudinal section of a kidney reveals an outer cortex, deeper medulla, and medial pelvis. Extensions of the pelvis (calyces) surround the tips of medullary pyramids and collect urine draining from them. 3. The renal artery, which enters the kidney, breaks up into segmental, lobar, and then interlobar arteries that travel outward through the medulla. Interlobar arteries split into arcuate arteries, which branch to produce cortical radiate arteries, which serve the cortex. 4. Nephrons are structural and functional units of the kidneys (Figure 15.2). Each consists of a glomerulus and a renal tubule. Subdivisions of the renal tubule (from the glomerulus) are glomerular capsule, proximal convoluted tubule, loop of Henle, and distal convoluted tubule. A second (peritubular) capillary bed is also associated with each nephron. 5. Nephron functions include filtration, reabsorption, and secretion (Figure 15.3). Filtrate formation is the role of the high-pressure glomerulus. Filtrate is essentially plasma without blood proteins. In reabsorption, done by tubule cells, needed substances are removed from filtrate (amino acids, glucose, water, some ions) and returned to blood. The tubule cells also secrete additional substances into nitrate. Secretion is important to rid the body of drugs and excess ions (potassium, hydrogen, and ammonia) and to maintain acid-base balance of blood. 6. Blood composition depends on diet, cellular metabolism, and urinary output. To maintain blood composition, the kidneys must: a. Allow nitrogen-containing wastes (urea, ammonia, creatinine, uric acid) to go out in the urine. b. Maintain water and electrolyte balance by absorbing more or less water and reclaiming ions in response to hormonal signals. ADH, which acts on the collecting ducts, increases water reabsorption and conserves body water. Aldosterone increases reabsorption of sodium and water and decreases potassium reabsorption. c. Maintain acid-base balance by actively secreting bicarbonate ions (and retaining H+) and by absorbing bicarbonate ions (and secreting H+. Chemical buffers tie up excess H+ or bases temporarily: respiratory centers modify blood pH by retaining C02 (decreases pH) or by eliminating more CO2 from the blood (increases blood pH). Only the kidney can remove metabolic acids and excess bases from the body. 7. Urine is clear, yellow, and usually slightly acid, but its pH value varies widely. Substances normally found in urine are nitrogenous wastes, water, various ions (always sodium and potassium). Substances normally absent from urine include glucose, blood proteins, blood, pus (WBC's), bile. Return to top Ureters, Urinary Bladder, and Urethra 1. The ureters are slender tubes running from each kidney to the bladder (Figure 15.4). They conduct urine by peristalsis from kidney to bladder. 2. The bladder is a muscular sac posterior to the pubic symphysis. It has two inlets (ureters) and one outlet (urethra). In males, the prostate gland surrounds its outlet. The function of the bladder is to store urine. 3. The urethra is a tube that leads urine from the bladder to the body exterior. In females, it is 3-4 cm long and conducts only urine. In males, it is 20 cm long and conducts both urine and sperm. The internal sphincter of smooth muscle is at the bladder-urethra junction. The external sphincter of skeletal muscle is located more inferiorly. 4. Micturition is emptying of the bladder. The micturition reflex causes the involuntary internal sphincter to open when stretch receptors in the bladder wall are stimulated. Since the external sphincter is voluntarily controlled, micturition can ordinarily be temporarily delayed. Incontinence is the inability to control micturition. Return to top Developmental Aspects of the Urinary System 1. The kidneys begin to develop in the first few weeks of embryonic life and are excreting urine by the third month, 2. Common congenital abnormalities include polycystic kidney and hypospadias. 3. Common urinary system problems in children and young to middle-aged adults are infections caused by fecal microorganisms, sexually transmitted disease-causing microorganisms, and streptococcus. 4. Renal failure is an uncommon, but extremely serious, problem in which kidneys are unable to concentrate urine, and dialysis must be done to maintain chemical homeostasis of blood. 5. With age, filtration rate decreases and tubule cells become less efficient at concentrating urine, leading to urgency, frequency, and incontinence. In males, urinary retention is another common problem. Return to top