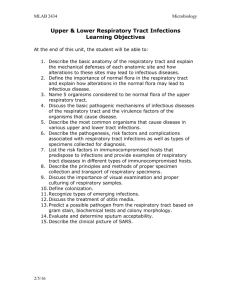
Upper Respiratory Tract Infections
advertisement

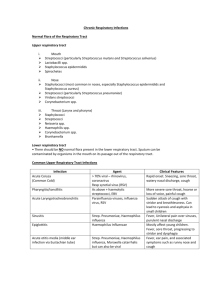
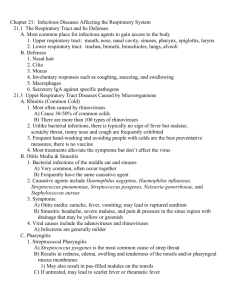
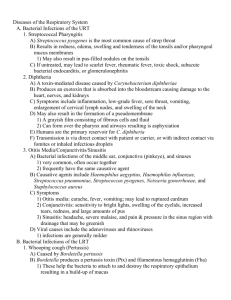
BIO 580 Medical Microbiology Unit 3 Respiratory Tract Infections 1 RESPIRATORY TRACT nose to alveoli continuous operation is essential constantly exposed to air & microbes divided into 2 regions : upper & lower Generalizations Many cause local infections, some may spread systemically Professional invaders - normal healthy host, specific attachment mechanisms, specific evasion tactics Secondary invaders - impaired host Most common infections seen by doctors High morbidity absenteeism Upper - usually mild & self-limiting Lower - can be severe & life-threatening in children bacterial in adults Upper Respiratory Tract Infections itis = inflammation - surface infections 1. Rhinitis = cold 100% viral (see Table 18.4) Rhinovirus and Coronaviruses - 50% 115 different Rhinoviruses all w/ different surface antigens Other viruses (Parainfluenza, Enterovirus, RSV, etc) transmission via aerosol and by contaminated hands bind to and infect ciliated epithelial cells of nose incubation is 1-3 days damage to epithelial cells mild inflammation, release of inflammatory mediators abundant mucus diagnosed by clinical signs & symptoms (burning sensation in nose/throat, followed by sneezing, runny nose, fatigue, malaise. Sore throat and cough generally due to post nasal drip. No or low fever) treatment is symptomatic control – interferon, sIgA, and IgG - immunity is short-lived BIO 580 Medical Microbiology Unit 3 Respiratory Tract Infections 2 2. Pharyngitis (= sore throat) and tonsilitis infected mucosa or inflammation of lymphoid tissue 70% viral – symptoms often include rhinorrhea, conjunctivitis, malaise or fatigue, hoarseness, and low-grade fever Rhinovirus, Coronavirus, Adenovirus, etc, see Table 18.5 CMV -clinically silent in URT esp. in infant/child – can spread from blood to placenta and infect fetus; second only to Down’s as a cause of mental retardation EBV -2 peaks 1-6 years and 14-20 years (infectious mononucleosis – fever, sore throat, petechiae on hard palate, lymphadenopathy and splenomegaly, with anorexia and lethargy. Symptoms due to release of cytokines. Plyclonal activation of B cells; WBC dif shows at least 10% atypical lymphocytes) EBV infections can reactivate, see Fig. 18.6. 30% bacterial – usually no rhinorrhea, cough, or conjunctivitis S. pyogenes (age 5-15), onset is abrupt, acute - chills, headache, severe sore throat, lymph nodes swell, tonsils tender w/ white, pusfilled lesions, high fever, no cough, no nasal discharge N. gonorrhoeae – in sexually active C. diphtheria – rare in U.S. 3. Otitis media and sinusitis = ear and sinus ear infections are second most common infection of childhood (after colds) and most common cause of visits to pediatricians 50% viral respiratory syncytial virus (RSV), influenza, parainfluenza, rhinovirus, adenovirus 50% bacteria - secondary invaders S. pneumoniae, Haemophilus influenzae, Moraxella 4. Epiglottitis H. influenzae type B (vaccination = Hib) Severe inflammation with edema life-threatening respiratory obstruction BIO 580 Medical Microbiology Unit 3 Respiratory Tract Infections 3 Lower Respiratory Tract Infections 1. Laryngitis and tracheitis Viruses (symptoms – hoarseness, burning retrosternal pain) Parainfluenza virus – croup (dry cough and inspiratory stridor) RSV, Influenza virus, Adenovirus Bacteria GAS, H. influenzae, S. aureus C. diphtheria - life threatening, rare in U.S. due to vaccination (DaPT) 2. Whooping cough Org - Bordetella pertussis (GNR, ox +, obligate aerobe) Humans are sole reservoir Highly contagious Transmission - person - person airborne droplets Colonization - attach to ciliated mucosa in trachea using fimbriae & hemagglutinin also spreads to bronchi Several toxic factors -affect inflammation or damage ciliated epithelium 1. pertussis toxin - A-B structure exotoxin; A unit is an ADPribosylase, disrupts signal transduction in affected cell - prod massive amts mucoid secretions 2. Adenylate cyclase toxin - enters neutrophils & causes them to incr. cAMP - inhibits chemotaxis, phagocytosis, & killing 3. Tracheal cytotoxin - kills tracheal epithelial cells 4. Endotoxin Incubation - 1-3 weeks Pathology - ciliated epithelium of trachea becomes covered w/ massive purulent exudate Presentation early - runny nose, sneezing, fever, mild dry cough week later - mucus & bact fill lower trachea, cough becomes paroxysmal - violent coughing fits, 5-20X w/ no breath in btwn - as air rushes back in - whoop also vomiting, epistaxis, periorbital edema, conjunctival hemorrhage Complications - CNS anoxia, secondary pneumonia Immunization - DaPT Rate of infection in unvaccinated exposed - 90-95%; Mortality - up to 14% BIO 580 Medical Microbiology Unit 3 Respiratory Tract Infections 4 3. Acute bronchitis - Inflammation of the tracheal/bronchial tree assoc w/ infection Orgs Professional pathogens; Viruses (rhino-, corona-, adeno-, influenzae,) and Mycoplasma pneumoniae Secondary invaders - S. pneumoniae, H. influenzae Presentation - cough - treatment is symptomatic - antibiotics? usually recommended 4. Influenza = the Flu Org - Influenzavirus types A, B, C; A - segmented RNA, 3 major HA types, 2 major NA types; antigenic epitopes change from yr-yr (antigenic drift & shift) Transmission - person - person small airborne droplets Colonization - attaches via HA to sialic acid receptors on ciliated epithelium of trachea/bronchi, RME Incubation - 1-3 days Pathology - impair mucociliary clearance, tracheobronchitis, bronchospasms; cytokines released from damaged cells & WBC may symptoms Presentation - fever 102-104, chills, severe headache w/ retro-orbital pain, muscular aches (esp backache), dry cough, weakness (prostration). Most cases resolve 1-2 wks Complications - 1º influenza pneumonia (1% of cases but 30% fatality, pregnant women ↑ risk), 2º bacterial pneumonia (H. influenzae, S. pneumonia, S. aureus, S. pyogenes) Epidemics are indicated by the number of unexpected deaths due to influenza, when # exceeds 10,000-50,000 = epidemic BIO 580 Medical Microbiology Unit 3 Respiratory Tract Infections 5 5. Bronchiolitis children less than 2 swollen by inflammation, passage of air is restricted necrosis of epithelial cells lining the bronchioles Orgs 75% RSV Respiratory Syncytial Virus - paramyxovirus (RNA), enveloped Most common cause of fatal bronchiolitis & pneumonia in infants (1/100 hospital) - humans only reservoir Transmission - resp. droplets to hands Colonization - nasopharynx - surface spikes are fusion proteins that fuse host cells to cause "syncytia", then virus invades LRT by surface spread in secretions Incubation 4-5 days Immunopathology - maternal Ab in infant react w/ virus Ag, liberate histamine & other inflammatory mediators Presentation - cough, rapid respiration, cyanosis 25% other viruses 6. Pneumonia 4,000,000 people/yr. Most common cause of infection related death in the US. 6th leading cause of death wide range of microbes Transmission - inhalation or aspiration Colonization - attach to resp epithelium Pathology - respiratory distress from the interference of gas exchange in lungs, systemic effects Orgs children - viral or bacteria secondary to viruses adults - bacterial, kind depends on risk factors, age, other diseases in hospitals GN BIO 580 Medical Microbiology Unit 3 Respiratory Tract Infections 6 Bacterial - acute onset, high fever Typical - classic bacteria of acute, community-acquired - S. pneumoniae (25-60%), H. influenzae (5-15%), others - S. aureus, Klebsiella, E. coli, Pseudomonas Atypical - M. pneumoniae, Chlamydia pneumoniae, Legionella pneumophila, Coxiella burnetii Chest exam rales (abnormal crackles) evidence of consolidation chest x-ray Viral Transmission - inhaled or from blood Colonization - attach specifically Orgs RSV - children Parainfluenza virus types 1 & 2 – children; hemagglutinin & neuraminidase & fusion proteins Adenovirus - 41 types; 5% of acute resp. illness Influenzavirus 7. Chronic Infections of the lungs Tuberculosis - review Fungi Aspergillus fumigatus – aspergillosis - Predisposing condition asthma, pre-existing lung cavities, chronic pulmonary disorders fungal ball aspergilloma doesn’t invade but in immunosuppressed invade lungs to produce disseminated disease Histoplasma capsulatum - histoplasmosis Coccidiodes immitis - San Joaquin Valley Fever Blastomyces dermititidis - blastomycosis Pneumocystis jiroveci (formerally P. carinii) - pneumocystis pneumonia 8. Cystic fibrosis very viscous bronchiol secretions leads to fluid stasis in the lungs & infections w/ P. aeruginosa (S. aureus, H. influenzae, B. cepacia)