Microbiology 62 [5-11
advertisement

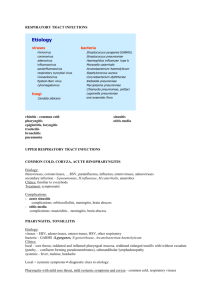
Microbiology 62: Respiratory System Infections - Most common site for infection Pneumonia = #1 cause of death from infectious disease Infections of Nose and Throat - - - Group A streptococcal pharyngitis = in school children in winter o Fever, tonsillar exudates, tender cervical adenopathy increase likelihood o Conjunctivitis, cough, coryza, diarrhea = decrease likelihood o Complications = peritonsillar and retropharyngeal abscesses, otitis media, sinusitis, pneumonia, acute glomerulonephritis, and rheumatic fever Rhinoviruses, adenoviruses (conjunctivitis), coronaviruses, influenza viruses and parainfluenza viruses may cause pharyngitis o Epstein-Barr virus common in adolescents/young adults o Enteroviruses (group A coxsackieviruses) -> herpangina (small vesicles in throat) Chlamydophila pneumoniae, Arcanobacterium haemolyticum, Mycoplasma pneumonia -> other causes of pharyngitis Common cold from viral infection of nasopharynx o 40-50% of colds caused by rhinovirus group o Coronaviruses next common group Infections of Epiglottis - - Clinical: trouble breathing, nasal flaring, drooling, fever Nafcillin effective against influenza B Acute epiglottitis = supraglottitis (URI), frequently 2-7 y.o from influenza B o Universal immunization against influenza B o In adults, S. pneumoniae and group A streptrococci more frequent causes Radiograph of lateral neck shows enlarged epiglottis (secure airway with endotracheal tube) Infections of Larynx and Trachea - Larangotracheitis = croup -> sudden onset of barking cough and difficult respiration o Viral URI (parainfluenza viruses 1-3) or rarely S. aureus, runny nose, hoarseness (in adults), cough o Mucous membrane edema -> narrows (esp inspiration = inspiratory stridor) o Self0limited resolving after 5-7 days o Provide oxygen, epinephrine, have child stand in steam room Infections of Large Bronchi - Acute tracheobronchitis = infection or inhalation of irritants o Viruses (rhino, corona, RSV, influenza, and adenoviruses) or bacteria (M. pneumonia, Chlamydophila pneumoniae, Bordetella pertussis) o o B. pertussis -> whooping cough Cough, myalgias, headache made worse by coughing, substernal chest pain, high fever COPD -> chronic bronchitis -> acute exacerbation of chronic bronchitis (AECB) ↑ cough and sputum production, sputum purulence, and SOB increase likelihood of bacterial infection Treat with antibiotics against H. influenzae, M. catarrhalis and S. pneumoniae Infections of Bronchioles - Bronchiolotis associated with respiratory synsytial virus Infections of the Lungs - - Acute pneumonia = sudden onset, progression of symptoms in few days o Community-acquired = person-to-person (airborne) or animal/environmental reservoirs (airborne or insect vectors) Pneumocystis carnii -> infect immunocompromised patients o Hospital-acquired (nosocomial) Subacute or chronic pneumonia = tuberculosis, fungal pneumonia, anaerobic lung abscess Entry and Spread - Direct inhalation, aspiration, spread along mucous membrane surface, hematogenous, or direct penetration Defense Mechanisms of lungs - - Vibrissae (hair in lungs) filter large particles Large particles (> 10 μm) settle at abrupt change points, small particles reach terminal bronchioles/alveoli o Endotracheal tubes predispose to pneumonia Epithelial cells covered with cilia containing lysozyme, lactoferrin, secretory IgA antibodies o Impaired cilia -> bronchiectasis (permanent dilation of small airways) Alveoli contain IgA antibodies, complement, and macrophages Acute Pneumonias - Community-Acquired Pneumonia (CAP) = fever, cough, chest pain (pleuritic), SOB, rapid respiration, cyanosis, crackles/rales o Typical presentation = high fever, shaking chills, chest pain, lobar consolidation S. pneumoniae most common cause, H. influenzae, S. aureus and other Gram – bacteria Predilection for very young and elderly (COPD) o Atypical presentation = less severe, dry cough, headache M. pneumoniae, C. pneumoniae and legionellae o o - Alcoholics increase risk for S. pneumoniae, Klebsiella pneumonia, S. aureus Nursing home, immunocompromised, and lung disease increase risk for Pseudomonas aeruginosa (Gram- enteric) and S. aureus o Chlamydia psittaci -> disease in birds -> psittacosis (parrot fever) o Coxiella brunetii -> farm animals -> Q fever o Legionella pneumphila -> contaminated water -> Legionnaire disease o <2 y agent usually virus (RSV, influenza, parainfluenza, adenoviruses) o Diagnostic finding (!) = infiltrate Focal lobar consildation with S. pneumoniae, K. pneumoniae, aspiration Diffuse interstitial infiltrates with M. pneumoniae, C. pneumoniae, P. carinii Cavitate -> S. aureus, Mycobacterium tuberculosis o Risk factors for drug resistant S. pneumoniae (DRSP) = recent respiratory infection, antimicrobial use, advanced age, immunocompromised or high risk area Hospital-Acquired Pneumonia (HAP) = new parenchymal lung infection 48+ hours after admission to hospital o Fever, cough, purulent (green) sputum production, SOB, pleuritic chest pain, tachycardia, tachypnea, tactile fremitus and dullness to percussion o Intubation -> ventilator-associated pneumonia (VAP) o Enteric Gram negative bacteria and S. aureus typically Enterobacteriaceae, K. pneumonia, Proteus species, E. coli Prolonged hospitalization => P. aeruginosa and Acinetobacter species o Therapy based on likelihood of infection with multidrug-resistant (MDR) pathogens Risk factors = antimicrobial therapy (90 days), 5+ day hospitalization, high MDR organisms around, immunosuppression, dialysis Treat with broad-spectrum antibiotics Subacute Pneumonias - Lung abscess from gross aspiration of oropharyngeal/gastric contents -> polymicrobial infection o Anaerobes and microaerophilic organisms from mouth o S. aureus, K pneumoniae, mycobacteria, and others too o Fungi -> Histoplasma capsulatum, Blastomyces dermatitidis, Coccidioides immitis, Cryptococcus neoformans o Clinical = fever, foul-smelling breath, amphoric breath sounds, lung cavity Pneumonia in the Immunocompromised Patient - Usually rarely cause infection in normal individuals P. carinii -> HIV pts, CD4 lymphocyte < 200 Low-grade fever, cough, fatigue, diffuse bilateral infiltrate, treat with trimethoprim and sulfamethoxazole Other infections from Aspergillus fumigatus and CMV -> immunosuppression for organ transplant