Infectious diseases
advertisement
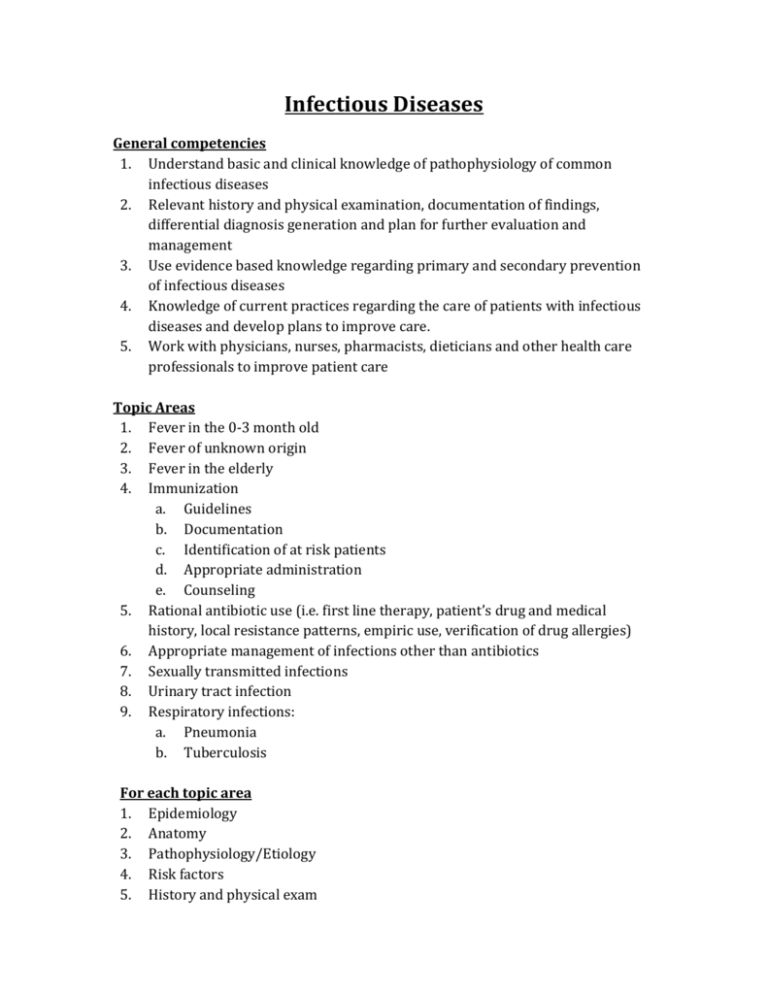
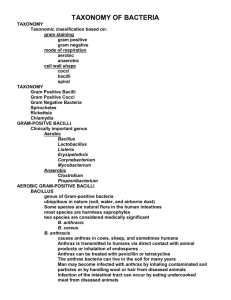
Infectious Diseases General competencies 1. Understand basic and clinical knowledge of pathophysiology of common infectious diseases 2. Relevant history and physical examination, documentation of findings, differential diagnosis generation and plan for further evaluation and management 3. Use evidence based knowledge regarding primary and secondary prevention of infectious diseases 4. Knowledge of current practices regarding the care of patients with infectious diseases and develop plans to improve care. 5. Work with physicians, nurses, pharmacists, dieticians and other health care professionals to improve patient care Topic Areas 1. Fever in the 0-3 month old 2. Fever of unknown origin 3. Fever in the elderly 4. Immunization a. Guidelines b. Documentation c. Identification of at risk patients d. Appropriate administration e. Counseling 5. Rational antibiotic use (i.e. first line therapy, patient’s drug and medical history, local resistance patterns, empiric use, verification of drug allergies) 6. Appropriate management of infections other than antibiotics 7. Sexually transmitted infections 8. Urinary tract infection 9. Respiratory infections: a. Pneumonia b. Tuberculosis For each topic area 1. Epidemiology 2. Anatomy 3. Pathophysiology/Etiology 4. Risk factors 5. History and physical exam 6. 7. 8. 9. Diagnostic Tests Differential diagnosis Management Psychosocial implications Highlighted teaching points 1. Risk Factors a. Identify patients who will specifically benefit from immunization (e.g., not just the elderly and children, but also the immunosuppressed, travellers, those with sickle cell anemia, and those at risk for pneumonia and hepatitis A and B) b. Patients at high risk for UTI: high-risk patients: pregnancy, immune compromise, neonate, young male, elderly male (prostatic hypertrophy) 2. History and physical exam a. In elderly, do not use fever, or lack thereof, as pathognomonic for pathology 3. Diagnostic tests: a. Use a selective approach in ordering cultures before initiating antibiotic therapy (usually not in uncomplicated cellulitis, pneumonia, urinary tract infections, and abscesses; usually for assessing community resistance patterns, in patients with systemic symptoms, and in immunocompromised patients) b. Screening appropriately for sexually transmitted infections c. Urinary tract infections i. rule out complications – sepsis, pyelonephritis, impacted infected renal calculi) ii. appropriate work-up of boys with UTIs, young girls with recurrent UTIs (ultrasound, etc) 4. Differential diagnosis a. Include infection in differential of confusion in the elderly, failure to thrive, unexplained pain (necrotizing fasciitis, abdominal pain in children with pneumonia) etc. b. Antibiotic allergy (rule out other causes before accepting the diagnosis) c. Fever in the 0-3 mo old: rule out bacteremia d. Fever of unknown origin i. Rule out life-threatening causes (meningitis, endocarditis) ii. Rule out non-infectious causes (i.e. drug reaction, heat stroke) e. Include diseases for which vaccination has been given in differential – do not assume complete immunity f. 5. 6. Consider other diagnoses if patient is not responding to usual treatment for infection g. Rule out sexually transmitted infection in any genito-urinary-abdominal symptom h. Rule out urinary tract infection in very young or elderly patients with non-specific symptoms (abdominal pain, fever, delirium) i. Differential diagnosis for dysuria: i. Sexually transmitted infections ii. Vaginitis iii. Renal calculi iv. Interstitial nephritis v. Prostatitis vi. Urinary tract infection Management a. Rational antibiotic use i. First line therapy, patient’s drug and medical history, local resistance patterns ii. Avoidance of antibiotic use in patient with suspected viral illness iii. Empiric use in urgent situations (meningitis, septic shock, febrile neutropenia) b. Appropriate management of infections other than antibiotics i. Fluid resuscitation in septic shock ii. I & D for abscess iii. Pain relief c. Sexually transmitted infections i. High risk and symptomatic: treat empirically ii. Treatment of partners iii. Contact tracing (public health agency) d. Urinary tract infections i. Modify treatment for high risk individuals (neonate, pregnancy, immune compromise, you and elderly men) ii. Treat empirically in pregnancy, sepsis, pyelonephritis Psychosocial implications a. Counseling for parents against vaccination References: 1. College of Family Physicians of Canada. (2010). Defining Competence for the purposes of certification by the College of Family Physicians of Canada: The evaluation objectives in family medicine. Mississauga, ON.