Dear Journal of Heart and Cardiology Editor, I hope you will find the
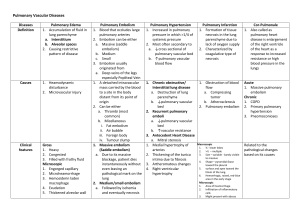
advertisement

Dear Journal of Heart and Cardiology Editor, I hope you will find the enclosed manuscript, “Cardiopulmonary Clots- Management of Acute Pulmonary Embolus in Association with Right Heart Thrombus: a Case Report” enlightening and worthy of sharing with your readers in the Cardiology Research Journal. The manuscript describes a patient we cared for in our teaching hospital. My faculty mentor, (Dr. Ali) and I (Yaser Jbara, MD) have shared in reviewing this case as well as preparing this manuscript. Thus we meet the criteria for authorship and will sign statements attesting authorship and releasing the copyright should our manuscript be accepted for publication. Dr. Ali and I have no potential conflicts of interest to disclose. Our manuscript has not previously been published nor is it under consideration elsewhere. All of our tables and figures are original. We are submitting our work as a case report. Our patient gave verbal consent for his de-identified medical information to be published as a medical case report. If you have further questions feel free to contact me; I am the lead author as well as the corresponding author. Contact information: Yaser Jbara, MD Wright State University, Boonshoft School of Medicine Department of Internal Medicine Weber CHE Building, Second Floor 128 East Apple Street Dayton, OH 45409-2902 Jbarayaser@yahoo.com yaser.jbara@wright.edu Omair Ali, MD Wright State University, Boonshoft School of Medicine Department of Cardiology Fellowship Weber CHE Building, Second Floor 128 East Apple Street Dayton, OH 45409-2902 Omairy2j@gmail.com Phone: 937-776-5822 FAX: (937) 208-2621 Sincerely, Yaser Jbara, MD Internal Medicine Residency Program Wright State University, Boonshoft School of Medicine Cardiopulmonary Clots- Management of Acute Pulmonary Embolus in Association with Right Heart Thrombus Abstract: Pulmonary embolism is a common and lethal disease. It may, rarely, coexist with right heart thrombus. When it does, it carries a high mortality risk. We describe here three patients with pulmonary embolism in association with a right heart thrombus, their approaches to management and outcomes. All three patients had a chest CT scan and an echocardiogram that showed RHT. Introduction: Right heart thrombus is a rare disease; it may coexist with pulmonary thromboembolism 4%-18%. The mortality is up to 44%. Though no treatment guidelines for management of right heart thrombus exist, we report 3 cases of right heart thrombus management with their outcomes. Patient 1: A 39 year old male with a history of deep vein thrombosis in his right lower leg, presented with sudden onset of shortness of breath. He was unable to refill Rivaroxaban and subsequently had not been taking it for weeks. He denied hemoptysis, fevers, chills or night sweats. His vitals were temperature of 98.3 F, respiratory rate of 29 per minute, pulse of 87 per min, blood pressure of 143/104 mm Hg and oxygen saturation is 97% on 1 L nasal cannula. Examination revealed clear lung auscultation and trace lower extremity edema. Cardiopulmonary examination was otherwise normal. Basic metabolic panel and complete blood counts were within normal limits. His electrocardiogram revealed normal sinus rhythm without acute changes. A Chest CT (Figure 1a,1b) revealed evidence of chronic pulmonary emboli in lower lobes of both lungs. Reports also commented on acute pulmonary emboli in the same distribution. Multiple filling defects were seen in a dilated right atrium, some of these were peripherally located and seemed adherent to the right atrium wall. He was admitted to the hospital and placed on heparin drip. A stat echocardiogram (Figure 1) showed ventricular septum with D-shaped conformation both at systole and diastole (suggestive of volume and pressure overload). Ejection fraction was preserved. The right ventricle was severely dilated. The right atrium revealed a thrombus close to the superior vena cava origin. It measured 3.3 cm in height x 1.8 cm in width x 2.8 cm in length. Tricuspid valve was structurally normal. The right ventricular systolic pressure was 95 mmHg (this was increased when compared to Echocardiographic parameters which showed an RVSP of 78 mmHg six months prior). These findings were suggestive of acute cor pulmonale. Thrombolytic agent was given. Concerns for distal embolization of right atrial thrombus into the pulmonary circulation with thrombolysis, the decision was made to surgically intervene. Intraoperative transesophageal echocardiogram (figure 3) delineated the right atrial mass. Right atrial thrombectomy was then performed (Video 1, Figure 4) He was continued on heparin drip and transitioned to Coumadin. His INR values were therapeutic on discharge. In follow up the Patient continues to fare well. Figure 4 1 Patient 2: A 65 year old female with history of chronic atrial fibrillation, on Rivaroxaban, presented with acute shortness of breath. She had denied any constitutional symptoms, hemoptysis, orthopnea or paroxysmal nocturnal dyspnea. EKG (figure 5) showed atrial fibrillation with rapid ventricular response and additionally right heart strain pattern. A CT of the chest showed bilateral acute pulmonary embolism in the proximal portions of pulmonary artery bifurcations (Figure 6a, 6b). She was placed on heparin for anticoagulation and Diltiazem drip for heart rate control. A focused echocardiogram showed three masses, loosely attached to each other, close to the posterior wall of right ventricle, without any visible attachment to any wall (Figure 7). Through interventional radiology, the patient underwent thrombolysis with alteplase via ekosonic endovascular system (eKOS). A repeat Echocardiogram two days later showed resolution of the right heart clots. She was discharged to the rehab center a few days later. Patient 3 An 82 year old female with Stage IV (metastatic) Breast Cancer reported sudden onset of labored breathing at home associated with lightheadness. Family contacted EMS. She was found via pulse oximetry to have an oxygen saturation of 78% on room air. She was also tachycardic with pulse of 107 beats per minute and hypertensive with blood pressures of 140/88 mm Hg. Examination revealed an elderly lady in respiratory distress. She was started on a face mask however oxygenation did not improve adequately. She was intubated on site. A CT of the chest (figure 8a,8b) revealed large pulmonary emboli to the right and left pulmonary arteries. The right atrium and right ventricle was noted to be enlarged. She was admitted to the intensive care unit for further care and management. She was deemed to not be appropriate candidate for thrombolytics. She was started on intravenous heparin for anticoagulation. An echocardiogram (figure 9,10) showed a large mobile thrombus measuring 3.2 cm x 3.8 cm, prolapsing through the tricuspid valve into the right ventricle and back into the right atrium. Family elected to not put her through extensive intervention or procedures. The patient continued to remain unresponsive. Her condition progressively deteriorated until clinical death two days later. Figure 8a CTPE highlighting Large pulmonary embolism in the right pulmonary artery Figure 8b CTPE highlighting Large pulmonary embolism in the left pulmonary artery Figures 9- 2D Echocardiogram in Apical 4 chamber view showing highly mobile thrombus moving from right atrium through the tricuspid valve into the right ventricle. Figures 10- 2D Echocardiogram in Right ventricular tilt position showing highly mobile large thrombus moving from right ventricle through the tricuspid valve into right atrium Discussion Acute pulmonary embolism (APE) is a common disease and can be fatal. Approximately 300,000 to 600,000 people are diagnosed each year in the United States. Per the center for disease control and prevention, it claims the life of 60,000-100,000 Americans annually. The incidence of right heart thrombus in pulmonary embolism is a rare phenomenon, authors have estimated it to be present 4% to 18% in the setting of an acute pulmonary embolus (1, 2,3) with a reported mortality over 44 % (1,4,5) as they transit from legs to the pulmonary vasculature. Therefore, it is crucial for physicians to evaluate if a right heart thrombus coexists with any patient presenting with a pulmonary embolism, as patients are at risk for compromise of the cardiopulmonary circulation and sudden circulatory failure [6]. Computed tomography pulmonary angiogram has been considered the definitive diagnostic imaging for detecting pulmonary embolism. Its sensitivity to also detect a coexisting right heart thrombus is not well known. The use of a bedside echocardiogram can offer vital clues toward the presence of pulmonary embolism. The diagnostic value of an ultrasonographical combined strategy (echocardiography associated with venous ultrasonography) is high and this strategy seems to be reliable in pulmonary embolism. In a patient with hemodynamic compromise, an echocardiogram showing right ventricular (RV) dilation and impairment, with spared involvement of the ventricular apex is the ‘McConnell sign’. This is highly suggestive of pulmonary embolism. This sign is due to the following proposed mechanism (7). To counter the abrupt increase in afterload and equalize the regional wall stress, the right ventricle assumes a spherical shape. The apical sparing is secondary to its tethering to a contracting and hyperdynamic left ventricle. In a patient with shock or hypotension, the absence of echocardiographic signs of RV overload or dysfunction practically excludes PE as a cause of hemodynamic compromise. Right heart thrombi in transit can also be sometimes found on transthoracic echocardiography (4). Electively, or in non-high risk situations (stable patients where mortality rates are low) it can offer prognostic information and risk stratify the embolism. (8). While we acknowledge that, in an isolated small to medium sized pulmonary embolus, the echocardiogram has a low sensitivity, this does increase exponentially when dealing with a massive pulmonary embolism (9). Moreover, if a right ventricular or right atrial thrombus is present, the sensitivity of an echocardiogram is high. The diagnosis of acute Cor pulmonale by direct visualization of right ventricle overload, paradoxical intraventricular septal motion and elevated pulmonary pressures is also an advantageous to echocardiogram [10]. If a trans-esophageal echocardiography is performed, it may allow direct visualization of a pulmonary embolus in the central pulmonary arteries and may also evaluate for the presence of a patent foramen ovale, which often harbors thrombus travelling from right to left atrium. As no prospective trials exist for the management of right heart thrombus in the setting of pulmonary embolism, recognition of diagnosis is considered an emergent management requiring thrombolysis or embolectomy. Several authors have described, that heparin alone has a mortality rate up to 100% and is not recommended as the sole treatment. Classic treatment is surgical embolectomy. A potential advantage of surgical approach is the ability to repair a patent foramen ovale if present, and reduce the risk of subsequent paradoxical embolism and stroke. However, potential complications include, use of general anesthesia, cardiopulmonary bypass, and inability to remove coexisting pulmonary thromboemboli beyond the central pulmonary arteries. Other treatment options of thrombolysis have been described to accelerate thrombus lysis, pulmonary reperfusion, reduce pulmonary hypertension and improve biventricular function by decreasing right ventricle–left ventricle interdependence. Moreover, thrombolysis has the additional benefit to dissolve clots in other locations at the same time, for example, the intracardiac thrombus, the pulmonary embolus, and the venous thrombosis. Finally, it is a simple, rapid, widely applicable treatment, and it can be administered at the bedside. Others have previously cautioned against the use of thrombolytic agents in type B thrombi. Thrombolytic agents may dissolve the adherent stalk and actually promote distal embolism of these organized thrombi (11). In Patients with PFO, fragmentation may lead to systemic embolization. Therefore, no standard treatment exists and patients may be treated per clinical setting. For patients with relative contraindications to both thrombolysis and embolectomy, interventional techniques have been described, for example, Aspiration thrombectomy, thrombus fragmentation, and rheolytic thrombectomy. Given the high mortality rate [1,3,12] , regardless of treatment, some authors recommended embolectomy [13] while others favored thrombolysis as a treatment [12,14] or as a therapeutic bridge to surgery [1] . In conclusion, though right heart thrombus in the setting of acute PE is a rare phenomenon, we suggest a minimum of non-invasive, simple bedside focused echocardiogram to look for right heart thrombus, as we recommend management via thrombolysis or embolectomy per case by case and avoid observation or heparin therapy alone as sole treatment for right heart thrombus in transit due to its high mortality rate. Further studies are needed to suggest best practical diagnostic approach and management on evaluation of right heart thrombus in the setting acute pulmonary embolism. References 1. Chartier L, Be´ra J, Delomez M et al. Free-floating thrombi in the right heart: diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation 1999;99:2779e83. 2. Ferrari E, Benhamou M, Berthier F, et al. Mobile thrombi of the right heart in pulmonary embolism: Delayed disappearance after thrombolytic therapy. Chest 2005;121:1051-3. 3. Torbiki A, Galie N, Covezzoli A et al. Right heart thrombi in pulmonary embolism: results from the international cooperative pulmonary embolism registry. J Am Coll Cardiol 2003;41:2245e51. 4. Casazza F, Bongarzoni A, Centonze F et al: Prevalence and prognostic significance of right-sided cardiac mobile thrombi in acute massive pulmonary embolism. Am J Cardiol 1997, 79:1433-1435. 5. de Vrey, Bax JJ, Poldermans D et al. Mobile right heart thrombus and massive pulmonary embolism. Eur J Echocardiogr. 2007 Jun;8(3):229-31. Epub 2006 May 23. 6. European Working Group on Echocardiography, “The European Cooperative Study on the clinical significance of right heart thrombi,” European Heart Journal, vol. 10, pp. 1046–1059, 1989. 7.Janz RF, Kubert BR, Pate EF et al Effect of shape on pressure volume relationships of ellipsoidal shells. Am J Physiol. 1980; 238: H917–H926. 8. Konstantinides S., Geibel A., Heusel G et al Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism. N Engl J Med. 2002;347:1143-50. 9. Calvin JE. Pressure segment length analysis of right ventricular function: influence of loading conditions. Am J Physiol. 1991; 260: H1087–H1097 11. Onwuanyi AE, Brown RJ, Vahedi M, et al. Eustachian valve thrombus: Critical factor in outcome of venous thromboembolism. Echocardiography 2003;20:71-3. 11. Thompson CA, TN Skelton. Thromboembolism in the right side of the heart. South Med J 1999;92:826-30. 12. Rose PS, Punjabi NM, Pearse DB: Treatment of right heart thromboemboli. Chest 2002, 121:806-814. 13. Cameron J, Pohlner PG, Stafford EG et al. Right heart thrombus: recognition, diagnosis and management. J Am Coll Cardiol. 1985 May;5(5):1239-43. 14. G. Pierre-Justin and L. A. Pierard, “Management of mobile right heart thrombi: a prospective series,” International Journal of Cardiology, vol. 99, no. 3, pp. 381–388, 2005.