Quick Care
advertisement

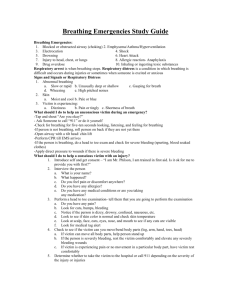
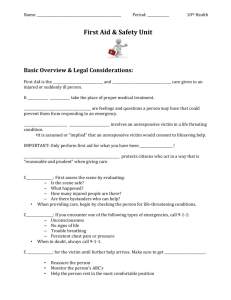
QUICK CARE “Quick Care,” is the immediate, temporary care given to BISD personnel and students in the case of an accident or sudden illness before the services of trained health professional can be secured. The Red Cross First Aid Manual is the suggested guide and was used as a reference for the pamphlet. This adaptation by Donna Knapp, RN and Phyllis Stout, RN It is important to prevent accident or illness when humanly possible. Nevertheless, in case of disaster, sudden illness or injury, the school should be prepared to give first aid/emergency care when necessary. Cardiopulmonary Resuscitation (CPR) should never be attempted by any person other than those trained and certified in CPR by a certified CPR Instructor. List of CPR Trained Staff Members 1. 2. 3. 4. 5. ____________________________ 6. _________________________ ____________________________ 7. _________________________ ____________________________ 8. _________________________ ____________________________ 9.__________________________ ____________________________ 10._________________________ In case of Sudden Illness or Injury 1. Administer quick care according to this reference. 2. Notify school Administrator. 3. Contact parent by phone at home or work; if unable to contact parent: a. Contact relative or friend as noted on the emergency card. b. Contact Emergency Medical Services (EMS) as deemed necessary 4. If you have difficulty determining the appropriate action to take, contact the school nurse or Central Health Services at 548-8191. Note: Transportation of ill students can only be provided by the parent or ambulance (NO EXEPTIONS). The safety of the student should be the primary concern in selecting appropriate transportation, if available discuss the situation with parent, and when in doubt call an ambulance. 1 IN LIFE-THREATENING SITUATIONS 1. If the illness or injury is clearly serious or life-threatening and requires immediate intervention by trained personnel, call 911 and ask for EMS. 2. Be prepared to give the following information: Your Name Phone Number Name of the School :_____________________________________ Street Address of the School:______________________________ The location of the injured person Description of the status -Level of Consciousness: Awake, Drowsy, Confused, Loss of Consciousness -Respiratory status (labored, rapid or depressed) -Bleeding: (major if direct pressure does not control the bleeding). 3. Assign someone to watch for EMS vehicle and stay on the phone for further instructions. 4. Examine the victim. An emergency is present if: IF DO Breathing has stopped Start CPR Breathing and Pulse have stopped Start CPR Bleeding is heavy Control blood loss (see BLEEDING) Person is in shock Treat the injury (see SHOCK) 2 ABDOMINAL PAIN 1. Keep the person quiet and have him/her lie down. 2. Take a temperature. 3. Have the person point to the place where he/she hurts. 4. If the pain is severe (not relieved by position changes and/or resting) or is accompanied by other symptoms: a. Do not give anything to eat or drink. b. Notify parents. ALLERGIC REACTION Allergic reactions can be caused by medications, foods, plants, chemicals or insect bites/stings and can lead to shock (see SHOCK). Symptoms can include a sudden rash outbreak, itching, wheezing, or difficulty breathing. 1. Reassure the person. DO NOT leave the person alone. 2. If breathing problems occur, 1) Follow policy for students with severe allergic reactions, 2) EpiPen, and 3) give artificial respiration as necessary and call EMS (911). 3. Notify parents. NOTE: If you are notified that a person is allergic to bee stings/insect bites, etc., make a contingency plan for procedures in the event of such an event. AMPUTATION OF SMALL BODY PARTS 1. Apply direct pressure to affected area to control bleeding. Cover with sterile dressing. 2. Place amputated part in a plastic bag with folded gauze or paper towel moistened in tap water. DO NOT wrap the body part. Float sealed bag on top of cool water. 3. Notify parent and advise to seek medical attention. 4. Watch for shock (see SHOCK). 3 ARTIFICIAL RESPIRATION A respiratory emergency is one in which breathing stops. Artificial respiration provides rescue breathing by allowing air flow into and out of the lungs. 1. Call or have someone else call EMS (911). 2. Open the airway a. Place the victim on his/her back. b. Lift up chin gently with one hand. 3. Check for breathing by placing your ear close to the victim’s mouth and: a. Look-at the chest for movement. b. Listen-for sounds of breathing. c. Feel for breath on your cheek. 4. If victim is not breathing: a. Pinch nostrils shut. Your other hand continues to hold chin up. b. Give 2 slow breaths. If resistance is felt, reposition chin. If chest does not expand, check for obstruction. FOR ADULTS/CHILDREN OVER 8 YRS insert your finger to sweep out obstruction. FOR CHILDREN 8YEARS AND UNDER, remove a foreign object only if it is visible. DO NOT do a blind finger sweep. When airway is open, continue rescue breathing at 12 breaths per minute (or 1 every 5 seconds). 5. Continue breathing for victim: a. Open your mouth wide, take a deep breath, form a seal and blow into victim’s mouth (chest should expand). b. Raise mouth and turn head to side, listening for exhalation. 6. For head injuries, use mouth to nose. Lift victim’s chin to close mouth. Seal your mouth around the victim’s nose, and then blow into nose. 4 ASTHMA 1. Help the individual rest in the easiest position for breathing (sitting usually makes breathing easier). 2. DO NOT leave the individual alone. 3. Check breathing pattern and skin appearance. 4. Reassure the individual and remain CALM. 5. Promote relaxation techniques by having the individual take slow, deep breaths. 6. Administer medications as directed by the individual student’s doctor/parent. 7. If breathing ceases, begin artificial respiration and call EMS (9-1-1). 8. Notify parents. 9. NOTE: If you are notified that a child is prone to asthma, make an individualized health care plan for the child in the event of an attack. BACK AND NECK INJURIES 1. 2. 3. 4. 5. DO NOT move person or leave alone. Do not lift head. Immobilize head or neck in position as found. Keep person warm, quiet and calm as possible. Treat breathing or bleeding emergencies. Call EMS (9-1-1) and notify parents. 5 BITES ANIMAL AND HUMAN 1. 2. 3. 4. 5. 6. 7. Flush area with lots of running water. Scrub area with soap and water. Apply ice pack if area appears red or swollen. Apply antiseptic ointment and cover with gauze or band aid. Notify parents. Check with physician regarding the need for tetanus booster. Report animal bites to Health Department. INSECT BITES/STINGS 1. 2. 3. 4. 5. 6. 7. Identify insect if possible. Remove stinger by scraping with fingernail, plastic card or tweezers. Wash area with soap and water. Apply antiseptic ointment and cover. Apply cold pack if needed and keep affected part below level of heart. Notify parents. Observe for 15 minutes for severe reaction like shock or difficulty in breathing. If a severe reaction occurs, contact EMS (9-1-1) and begin artificial respiration if breathing ceases. SNAKE BITE 1. 2. 3. 4. 5. Immobilize individual immediately. Identify snake if possible. Wash wound. Keep bitten part still and lower than the heart. Contact EMS (9-1-1) for further instruction. 6 BLEEDING 1. Apply direct pressure over the area until bleeding stops. If clean gauze is not available, use direct pressure with hand. 2. Elevate bleeding part, if possible. 3. If direct pressure and elevation does not stop bleeding, apply pressure to artery supplying the area. 4. Do not remove pressure bandages once they have been applied. 5. Treat for shock, if indicated. 6. If bleeding is profuse or life-threatening, call EMS (9-1-1). 7. Notify parent. BRUISES/TRAUMA 1. 2. 3. 4. Elevate and rest the bruised area. Apply ice immediately. Remember R.I.C.E. (Rest, Ice, check Circulation, Elevation). Notify parents. 7 HEAD INJURIES Injuries to the head are potentially life threatening. Suspect a skull or head injury if there is: a. A deformity of the skull; b. Blood or clear fluid draining from the ear or nose; c. Loss of conscious. 1. Maintain an airway. (Lift up chin gently with one hand; if neck injury suspected. Immobilize neck and use jaw thrust maneuver to open airway if necessary). 2. Call EMS (911) if unconscious or a skull fracture is suspected. 3. Control Bleeding (Except for drainage from the ear or nose, it should be allowed to flow). 4. Treat for shock. 5. Cover open wounds. 6. Keep lying down and quiet. 7. If secretions accumulate in the throat (bleeding, vomit) position the injured to allow for drainage (log roll to side without bending neck). 8. This injury may become an emergency. Observe for symptoms of: Confusion/disorientation Pupils of eye unequal in size or do not respond to light Headache Vomiting Loss of balance, dizziness 9. Notify parent to advise them of injury and symptoms. 8 HEAT EXHAUSTION HEAT STROKE Symptoms: Symptoms: Normal body temperature high temperature (105F or higher) Profuse perspiration Hot, flushed, dry skin Rapid and weak pulse Rapid, strong pulse Tiredness, weakness, May be unconscious Headache, nausea 1. Have Person lie down in a cool, quiet place. 1. Call EMS (911). 2. Loosen clothing. Remove tight or heavy clothing 2. Place in a cool, quiet 3. Take temperature. 3. Remove outer clothing. 4. Apply cool, wet clothes or sponge with cool water. 4. Apply cold, wet clothes or sponge with cool water. 5. Give sips of cold water. 5. Take temperature. 6. Call parent. 6. If conscious, give sips of cold water. 7. Call EMS (911) if condition worsens or person shows signs of shock. 7. Notify Parent. 9 HYPERVENTILATION A condition in which breathing is too shallow and rapid, usually due to anxiety/stress. It can lead to fainting (See FAINTING). Symptoms: shortness of breath, anxiety, dizziness, numbness/tingling, possible palpitations, chest pain. 1. 2. 3. 4. Have person sit down and encourage focusing on breathing slowly. Have person sip small amounts of water. (To help slow breathing) Provide soothing, calming encouraging words. Notify parent. 10 BURNS HEAT A. 1st degree (skin is reddened) and 2nd degree (skin is blistered). 1. Apply cold water for 0-15 minutes until pain is relieved 2. Apply first aid burn cream 3. Cover with non-adhering dressing 4. Notify parent B. 3rd degree (skin is burned away). 1. DO NOT apply ice or cold water. 2. DO NOT remove clothing. 3. Cover area with clean material. 4. Treat for shock (see SHOCK). 5. Seek immediate medical attention (EMS/911). 6. Notify parent. NOTE: Electrical burns are usually 3rd degree. DO NOT TOUCH. Cover with clean material and seek medical attention (EMS/911). (see SHOCK). CHEMICAL 1. Flood area with tap water for 5 minutes to dilute the chemical. 2. Apply clean bandage. 3. In severe burns, call EMS (911). 4. Notify parents. FRICTION 1. Clean with soap and water. 2. Cover to protect. 3. Apply ice bag if needed for comfort. 11 CHOKING A foreign body in a person’s throat blocks the airway. The person will be unable to speak or breathe; the face may turn blue and if obstruction is complete, the person may collapse. If conscious: Stand behind the person and: 1. Perform abdominal thrusts. ** a. Wrap your arms around the victim’s waist allowing the upper part of the victim’s body to hang forward. b. Make a fist with one hand and place the thumb side against the victim’s abdomen slightly above the navel. Then, grasp fist with the your other hand. c. Give quick inward and upward thrusts. 2. Repeat abdominal thrusts until object is dislodged or the victim becomes unconscious. 3. Once the object is dislodged, notify parent and advise medication attention. NOTE: ** For a small child or pregnant woman, give thrusts in chest area, midway between the nipples. If the person becomes unconscious: With the person lying down: 1. Call or have someone else call EMS (911). 2. Turn the victim on his/her back. 3. Lift jaw and hold tongue to open mouth. Use your index finger to sweep the victim’s mouth to remove the foreign body. 4. Open the airway and give a rescue breathe. 5. Begin CPR. NOTE: If the victim is a child, DO NOT SWEEP THE MOUTH if you cannot see the object. 12 CONVULSIONS/SEIZURES Convulsions or epileptic seizures usually end spontaneously. Body muscles become rigid, followed by jerking movements. Unconsciousness may occur. 1. remain calm, note the time and observe the child. 2. Lower the child to the floor 3. KEEP AIRWAY OPEN- turn head and body to side. 4. Protect the victim from injury. a. DO NOT restrain movement. b. DO NOT force mouth open or force objects between teeth. c. DO NOT give fluids. d. Move objects away or people away. e. Place something soft and flat under the person’s head f. Time the seizure 5. Loosen tight clothing (especially at neck). 6. Call EMS (911) if the child is not known to have seizures. 7. Follow individual plan of care for the child if known history of seizures. 8. Notify parent. NOTE: If you are notified that a person is prone to seizures, make a contingency plan for procedures in the event of a seizure. CUTS>SCRATCHES/PUNCTURE WOUNDS 1. Wash gently with soap and water. Puncture wounds will need careful cleaning. 2. Rinse under running water if possible. 3. Cover with band aid or sterile dressing. 4. Notify parents that stitches are indicated if the wound is over a joint or more than 1/8” deep and is a fresh wound. 5. When contacting the parent, remind them to inquire about the tetanus vaccine with their physician. 13 DRUG INTOXICATION / POISONING Symptoms may vary widely according to the specific drug or substance and the route of administration. Possible Symptoms: Central Nervous System: Confusion, dizziness, drowsiness, dilated or pinpoint pupils, muscular twitching, tremors, convulsion/seizure, delusions, hallucinations, loss of consciousness, irritability. Respiratory System: Rapid or labored breathing. Gastrointestinal System: nausea, vomiting, abdominal pain, diarrhea. Circulatory System: pale, flushed or bluish skin, weak or rapid heart rate. 1. Place in a safe, quite environment- with 1 or 2 people to supervise. 2. Observe for shock and or cardiac/respiratory arrest. If these develop, begin CPR and have someone call EMS (911) 3. Try to determine type of drug or substance involved and time. 4. Call the Texas Poison Center Network @ 1-800-222-1222 for appropriate actions 5. Notify parents. 6. Notify school administrator. 14 EYES A. Foreign bodies: Note: DO NOT remove object protruding from the eye. Cover with loose fitting shield (small paper cup). Notify parent. Seek immediate medical aid. 1. DO NOT RUB EYE. 2. Lift upper eyelid outward and down over the lower lid allowing tears to wash object out of eye. 3. If particle does not wash out, keep eye closed and bandage eye lightly. 4. Notify parent. Seek medical aid. B. Cuts and punctures of eye or eyelid: 1. If no open wound-patch with clean pad and apply ice pack. 2. External open wounds-apply sterile dressing and ice pack. 3. DO NOT flush punctured eyeball with water. C. Blows to the eye: 1. Apply cold compress immediately for 15 minutes and again each hour as needed. 2. Notify parent. 3. Seek medical aid if vision is blurred or eye appears abnormal (black eye or blood in eye). D. Chemical burns: 1. IMMEDIATELY FLUSH WITH WATER FOR 15 MINUTES. Make sure lids are held open. 2. Notify parent. 3. Seek immediate medical aid. DO NOT bandage eye unless severe pain is present. 15 FRACTURES/SPLINTING Signs of a broken bone (Fracture) are not always obvious. Suspect a fracture if: Loss of motion of the part Deformity when compared to mate Arm or leg in unnatural position Localized tenderness Swelling and discoloration Person heard a “crack” or felt a “snap” Bone protruding through skin Prevent movement of suspected fracture by splinting before moving (unless the injured is in danger of further injury). Never straighten or reposition a limb. 1. 2. 3. 4. 5. Treat for shock, as needed ( see SHOCK) Control bleeding. Cover with clean (or sterile) dressing if the skin is broken. Apply ice pack. Arrange transportation-call EMS (911) and /or parent. If EMS has been called, wait for them to splint. Splints: a. Use items like newspaper, magazine, wood, pillow, and umbrella. b. Hold in place by cloth strips, triangular bandage, necktie, and roller bandage. c. Include joints above and below suspected fracture. d. Pad for protection. e. Don’t interfere with circulation. When splinting: A. never straightens or reposition limb. B. always splint in position found. 16 EAR A. If foreign bodies (insect, bean, pebble etc) are detected: 1. Notify parent 2. Urge immediate medical attention. NOTE: DO NOT ATTEMPT TO EXTRACT OR INSERT ANYTHING INTO THE EAR B. If decreased hearing, pus, bleeding in the ear, fever or complaints of pain are present: 1. Notify parent, 2. Urge immediate medical attention. JAW MOUTH INJURY Any jaw/mouth injury could interfere with breathing. 1. Maintain open airway with chin lift. 2. Check mouth for injury. 3. Remove teeth (see TEETH AND GUMS) which may have been knocked out. 4. Control any bleeding externally. 5. Apply ice pack (If injury to tongue, to suck on ice). 6. Observe for signs of complications (shock, obstructed airway, unconsciousness). 7. Call EMS (911) if necessary. 8. Notify parent. NOSE POBLEMS A. Nosebleed. 1. Have person sit up with head straight. 2. Press nostril(s) firmly against the middle partition of the nose for 5 minutes. 3. Apply ice pack over nose. 4. Instruct patient not to blow or pick at nose for several hours. B. Fall or blow to the nose. 1. Treat for nosebleed if necessary. 2. Apply ice. 3. Have person sit up if able. 4. Notify parents if severe pain, uncontrolled bleeding or nose appears deformed. 17 SHOCK Shock occurs when there is insufficient flow of blood to the brain. It can occur even after minor incidents. Shock can be caused by allergic reactions, heart failure, injury (including blood loss) and electricity. Signs of shock include: Faintness weakness paleness cold sweat weak, rapid pulse shallow irregular breathing nausea, vomiting dizziness 1. Call EMS (911). 2. Cover enough to keep warm. 3. Check breathing-if absent, start artificial respiration. 4. Check pulse-if absent, start CPR (if certified only). 5. Keep lying down with feet slightly raised (except for head or back injury-DO NOT move victim). 6. Notify parents. NOTE: For electrical shock, follow these steps first, and then proceed as above: 1. Disconnect plug or throw main switch. 2. Separate victim from current (use long dry pole, rope, or cloth and stand on dry area). 18 SPLINTERS 1. Do not attempt to remove splinter if you cannot easily grasp the splinter with tweezers. a. Gently wash area with soap and water. b. Apply sterile dressing. c. Notify parents. 2. If splinter can be grasped by tweezers and is not near a delicate structure, remove it and wash area with soap and water. SPRAINS/STRAINS 1. 2. 3. 4. 5. DO NOT allow to walk if ankle or knee is injured. Remove shoes, rings, bracelets, etc from injured part. Elevate injured part. Apply ice at intervals of 20 minutes on and 20 minutes off. Notify parents. TEETH If knocked out: 1. 2. 3. 4. Hold tooth by crown. Rinse carefully. Keep moist in a cup of water, saliva, or milk. Notify parent-recommend dental appointment within 30 minutes. If chipped, cracked or loose: 1. Notify parent. 2. Recommend dental appointment. 19