pharm 21 [4-20
advertisement
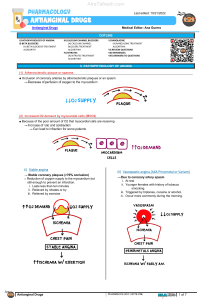
Chapter 21 Pharmacology of Vascular Tone Objectives 1. How will ventricular pressure, chamber radius, and wall thickness change O2 demand? Greater pressure and chamber radius will increase wall stress, which increases oxygen demand Greater ventricular wall thickness will decrease wall stress, which decreases oxygen demand 2. What is afterload? What is preload equal to? Afterload is the [aortic] pressure that the heart must overcome to eject its contents i. Basically, systolic pressure; think “aftercontraction” Preload is the end diastolic wall stress on ventricular fibers, just before they contract i. Approximates diastolic pressure 3. 4. Outline the steps leading from Ca++ influx to vasoconstriction: Ca++ => MLCK activation =phosphorylates=> Myoslin Light Chain => crossbridge cycle What class of drug activates guanylyl cyclase? What else does it do? nitrates (via nitric oxide) activate Guanylyl cyclase, which produces cGMP nitrates => guanylyl cyclase => cGMP => myosin light chain phosphatase => dephosphorylates myosin light chain => relaxation of smooth muscle nitrates also activate K+ channels=> cell hyperpolarizes=> Ca++ channels close => vasodilation 5. What’s the difference between endothelin-A and -B receptors? Both receptors cause constriction at vascular smooth muscle, but endothelin-B receptors also cause vasodilation at vascularendothelial cells; vasoconstriction wins out 6. Do nitrates reduce preload or afterload? What do they do to heart vasculature? Something in veins metabolizes nitrates into NO, this reduces preload (at least at low doses!) i. Don’t use nitrates on people with diastolic heart failure b/c they need preload In coronary vasculature, large arteries are dilated preferentially, which prevents coronary steal phenomenon [heart art] 7. Which nitrates can be administered sublingually (NOT swallowed)? Isosorbide dinitrate and nitroglycerin can be given sublingually 8. When is inhaled nitric oxide gas indicated? When is sodium nitroprusside used? Why is it dangerous? For newborns with primary pulmonary hypertension Hypertensive emergencies Beware the cyanide groups; acid-base disturbances, arrhythmias, toxicity in people with impaired renal function=> severe nervous system dysfunction 9. Which nitrate has a long half-life and is administered PO? Why is this quality important? Isosorbide 5-mononitrate is an excellent drug. It’s long half life means that when you need to lower the dose to prevent tolerance, the therapeutic concentration varies from high to low, not from high to zero So you don’t have to choose either tolerance or rebound angina, you can avoid both! 10. According to the sulfhydryl hypothesis, how should tolerance be reversed? What is the other hypothesis? N-acetylcysteine (like treating an acetominophen overdose) that free radicals inhibit guanylyl cyclase 11. What are the three boner drugs? What is their possible adverse effect on eyesight called? The phosphodiesterase-5 inhibitors are: Sildenafil, vardenafil, and tadalafil (=cialis: longer time to onset and longer half life than the first two) These can cause nonarteritic ischemic optic neuropathy (NION) 12. In what vessels are calcium channel blockers most effective? Calcium channel blockers have the greatest effect in arteries [Cal Art] i. Muscle is not affected because it relies on intracellular Ca++ stores 13. How do the dihydropyridines differ from the other calcium channel blockers? Dihydropyridines like amlodipine, nifedipine, and felodipine are less likely to exacerbate heart failure because they do not depress conduction, contractility, and automaticity as much 14. What are the side effects of nifedipine? What sets Amlodipine apart from the others? Nifedipine’s rapid onsent can cause reflex tachycardia, and can in rare cases causes myocardial infarction or angina Amlodipine has the slowest rise and longest half life because of its positive charge 15. What are the other two calcium channel blockers? Do they interact with each other? What special effects do they have? Are there any other interactions? Verapamil (phenylalkylamine) and diltiazem (benzothiazepine), which inhibit each others’ action Their main extra effect is depression of cardiac contractility, so they are useful for hypertension and angina combined They also treat SA and AV arrhythmias by decreasing automaticity and conduction velocity Diltiazem binds synergistically with nifedepine 16. Refractory hypertension is best treated using which drug class? What is a common adverse effect, and what class of drug can be added in order to prevent it? Potassium channel openers: minoxidil, cromakalim, pinacidil, and nicorandil Reflex tachycardia: use β-blockers since they prevent reflex sympathetic activity 17. Which vascular tone drug often causes an elevation in serum transaminase levels (a liver function test)? The endothelin receptor antagonist bosentan can cause hepatotoxicity (less pronounced in other -sentans) [the Bose blasted my liver!] 18. What weird adverse effect does hydralazine cause? Why? In slow acetylators (slower degraders), a lupus-erythematosus-like syndrome can occur 19. What do α1-adrenergic antagonists like prazosin, doxazosin, and terazosin treat besides hypertension? Benign prostatic hyperplasia 20. What ability of beta blckers is attractive for hypertension? Selective β-1 blockers (atenolol, metropolol) exert negative inotropy, which reduces both myocardial O2 demand and blood pressure gauranteed 21. What does the –sartan ending denote? Angiotensin-1 receptor antagonists end in –sartan, like losartan and valsartan [salt on the table’s sartén] Evan, Sorry for the long delay, There are a lot of good reasons to use these drugs. As is so often the case, someone may be experiencing multiple pathologies simultaneously, e.g., hypertension and angina. The vasodilatory effects are useful for the angina and the the cardiodepressor effects would decrease the work of the heart, also good for angina but also decreasing cardiac output, thus decreasing blood pressure. Verapamil and diltiazem are also useful in arrhythmias involving SA node (decrease rate of contraction) or AV node (decrease speed of conduction through AV node: prevents communicating something like atrial fibrillation(not life threatening) to the ventricles (V. fib would be life threatening). There are other good reasons to use these drugs but, as you can see, they are useful in their own right, and different from dihydropyridine Ca++ blockers. Hope that helps, Dr. Linville