IHD Management: Angina, ACS, MI - Lecture Notes
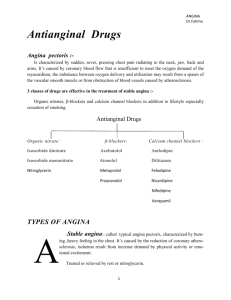
advertisement

1 Principles of Management of IHD (30-31H) By Dr Attia Jabr 1. Management of stable angina Aim of treatment: A. Treatment of the predisposing factors (HT, DM, Smoking, Dyslipidemia) B. Relieve symptoms C. Improve the prognosis Angina has a circadian rhythm and occurs most frequently in hours of waking. So, drugs given for prophylaxis should ideally provide cover to this period. The principles of management are: 1. Do not rely on symptoms and the response to treatment as a good guide for the severity of the disease. Exercise stress test is more accurate 2. Life style changes (Smoking ▼50%, Obesity, Hypertension, DM) 3. Treat provoking factors as anemia, arrhythmias, thyrotoxicosis 4. Acute attack : A. SL Nitroglycerine (begins within 1-2 minutes, but gives protection for only 20-30 min) B. SL Nitroglycerine : For immediate prophylaxis (before exercise) C. Nifedipine Caps 10 mg: Can be bitten and the contents swallowed. (in case of intolerance to nitrates) 5. Long term prophylaxis: A. B. Blockers. First line but if contraindicated give: B. Ca Channel Blockers (deltiazem & Verapamil).Why?. C. Nitrates. Second line. Why? Tolerance D. Combinations: 1. If one drug is not effective 2. B. Blockers + Nifedipine not verapamil. Why? 3. B. Blockers or CCBs + Long acting nitrates 4. Nicorandil could be used in combination therapy 5. Triple therapy (B. blockers +CCBs + Nitrates) 6. low dose aspirin reduces the risk of subsequent MI by about 35% 7. Lowering plasma cholesterol to < 160 mg/dl (LDL< 100), better by statins reduces the risk of MI by 25-30% 8. Angiotensin converting enzyme inhibitors: ▼CVS events & sudden death Indications of coronary angiography: 1. The diagnosis of angina is in doubt 2. The symptoms are not controlled by medical therapy 3. Stress tests suggest the presence of severe coronary artery disease Revascularization: Indications: 1. Poor performance in exercise stress test although medical therapy 2. Failure to respond to two prophylactic drugs in adequate dosages Types: 2 A. Coronary Artery Bypass Grafting (CABG): Better than drugs for patients with left main stem stenosis And patients with triple disease with impaired left vent. Function B. Percutaneous Transluminal Coronary Angioplasty (PTCA) often with insertion of a stent: Symptom relief only. Restenosis in 40% after 6 months. Bare-metal stent 20%, drug-eluting stents (with sirolimus) reduced restenosis to 6%. Intensive antiplatelet therapy to minimize restensosis by Aspirin + Clopidogrel for 6 w if the patient is in a high risk add abciximab (acute coronary syndrome) Management of Acute coronary syndrome 1. Unstable angina: A. Presents with symptoms at rest, or rapidly accelerating pattern angina attacks that are produced on minimal exertion. B. It requires urgent treatment to reduce the 10% risk of subsequent MI C. Steps of management are: 1. Low dose aspirin after a loading dose 2. Full dose of heparin ( 1 & 2 reduces MI and deaths by about .▼60%) 3. B. blockers (first choice) .▼15% 4. CCBs (verapamil or deltiazem) second choice if B. blockers are contraindicated. reduction MI 5. Do not use nifedipine alone but with B. blockers. Why? 6. Nitrates by all routes.SBI They relieve symptoms but do not improve the prognosis. 7. Clopidogrel is added to aspirin for 1 year if cardiac markers are raised. .▼ 20% 8. Platelet inhibition with I.V glycoprotein IIb/IIIa antagonist (abciximab). Reduces MI in high risk patients like High troponin I or T( Who need emergency revascularaization) 9. Cholesterol reduction like in stable angina.Statins.▼ 25-30% atorvastatin 80 mg 10. In acute phase of unstable angina, angiography, followed by CABG or PTCA are reserved for patients who are refractory to medical treatment (10%), raised cardiac markers, positive exercise stress test. 11. Urgent angioplasty or by pass graft is the treatment of choice Management of myocardial infraction with ST-segment elevation: A. Acute management: Objectives: 1. Pain relief 2. Reperfusion of the occluded artery 1. 2. 3. 4. Pain relief: IV diamorphine + antiemetic. Not IM. Why? Nitrates (SL or IV): Why they relieve pain? IV B. Blockers (provided no HF) Thrombolytic therapy: Indications: 1. MI with ST-segment elevation in two or more leads 2. MI with LBBB on ECG 3. A good history of MI but cannot diagnosed by ECG, high mortality a. IV thrombolytic therapy (streptokinase or Alteplase (R.t plasminogen activator). Anistreplase given IV in 5 min when no hospital. b. What is the differences between them? What are the indications of each?. c. Efficacy-Mortality-BP-Ab-Heparin 3 d. Which one of the previous thrombolytic should be followed by heparin? Why? e. The earlier the injection of the thrombolytic therapy the more lives saved. Within 6 h (30/1000& 6-12h=20/1000) 5. PTCA with stenting if thrombolytic therapy is contraindicated (primary PTCA) or failed (secondary PTCA) 6. Treatment of complications of MI which include HF, C shock, Cardiac rupture, Arrythmias, pericarditis, mural thrombus. B. Secondary prophylaxis after MI: reduce late mortality 1. 2. 3. 4. 5. 6. 7. 8. 9. Stopping smoking ….50% reduction Rehabilitation programs including Exercise……………..25% reduction Low dose aspirin: Begin with a loading dose within 24 h of MI B. blockers: orally soon after MI 25% reduction ACE inhibitors: in patients with HF or left ventricular dysfunction after their infraction…25% reduction Verapamil & deltiazem (less effective small reduction of infraction but no reduction of mortality): Indicated if there contraindications for B. blockers and in whom there is no significant left ventricular dyusfunction. Nifedipine is not indicated.Why? Prophylactic anticoagulants with SC heparin to prevent DVT. Warfarin similar to aspirin in effect. Indicated if aspirin is contraindicated? Can be combined with aspirin but with risk of bleeding. Cholestrol reduction by diet and statins reduces reinfraction by 25-30%. When do you think to use fibrates? ▼HDL Mediterranean diet + omega-3 FA(antiarryhtymic effect) Think in these minor cases: Case 1: A patient comes to your office with effort-induced angina and resting tachycardia. You choose the following drug to treat the patient because it slows the heart rate by blocking the L-type calcium channels in the SANode 1. Verapamil 2. Propranolol 3. Nitroglycerine 4. Isosorbide dinitrate 5. Metoprolol Case 2: Which of the following hemodynamic effects of nitroglycerin are primarily responsible for the beneficial results observed in patients with exertional angina? 1. Reduction in the force of myocardial contraction 2. Reduction in systemic vascular resistance (afterload) 3. Increase heart rate 4. Reduction in the venous capacitance (preload) 5. Increased blood flow to the subepicardium Case 3: 4 A woman is prescribed a combination of drugs consisting of a nitroglycerine patch and a B. blocker, such as propranolol to treat her attacks of angina. Which effect of propranolol would counteract an adverse effect of nitroglycerin? 1. A decrease in the preload 2. A decrease in the after load 3. A decrease in heart rate 4. An increase in the myocardial contractile force 5. A reduction in coronary vasospam Case 4: A patient who has been taking propranolol for a long period for secondary angina comes to your office complaining of increased frequency of chest pains on exertion. You decide to stop propranolol and give him deltiazem because you thought he has a mixture of stable and prinzmetal angina. Why would deltiazem be more likely to relieve the angina if your new diagnosis is accurate? 1. Deltiazem decreases heart rate 2. Deltiazem dilates coronary vessels in spasm 3. Prodsuces AV block 4. Reduces mycocardial contractility 5. Reduces after load Case 5. Metoprolol would produce which beneficial effect in a patient with stable angina: 1. A decrease in preload 2. An increase in the collateral blood flow 3. An increase in the after load 4. An increase in the diastolic filling time 5. An increase in blood flow through a constrict stenosis Case 6: 60-year-old man comes into the office complaining of chest pain that primarily occurs in the early morning and do not appear to be associated with stress or exercise. Following coronary angiography you determined that this patient has angina pectoris as a result of coronary artery spasm. How would you 1) Treat the patient to alleviate the acute attacks when they occur? 2) Treat chronicity to prevent their recurrence? Case 7: Ali, a 45-year-old male, long distance lorry driver, had been having episodes of chest pain that he likened to indigestion. They were brought on by moderately strenuous exercise and relieved by rest but were not relieved by antacids. They had been present for approximately 1 year but recently the frequency and intensity of the pains had become worse and they were now occurring several times a week. He was hypertensive and his serum cholesterol level was 270 mg/dl. He smoked 40 cigarettes/day and was overweight. He drank 10 units alcohol/week. He performed well on exercise test but his exercise ECG showed antero-lateral ST segment depression at peak exercise. There was no evidence of heart failure. A diagnosis of angina was made. 1. How would his acute attacks of angina be treated? 2. The frequency of attacks required prophylactic treatment. What options are available to reduce the frequency of anginal attacks? 3. What other drugs are likely to be useful to improve his prognosis? 4. Are life-style changes likely to help in this patient? 5 5. If Ali was an 80 y old, what additional precautions should you consider when prescribing his medications? 6. In unstable angina, which drug treatments are likely to reduce the progression of the episodes to myocardial infraction or sudden death? Despite continuing medication, 6 months later, Ali awoke with severe chest pain and dyspnea that was not relieved by nitroglycerin. Examination, biochemical tests and ECG all led to the diagnosis of MI 1. What is the likely cause of myocardial infraction? 2. Why is it important to give thrombolytic therapy as quickly as possible? 3. Ali was given the thrombolytic agent rt- plasminogen activator because of fears that he would get an allergic response to streptokinase. Was this justified? 4. He was given 150 mg aspirin daily orally. Does this have any benefit if thrombolytic therapy is also given? 5. The normal therapeutic dose of aspirin for headache is about 650 mg. Why was the dose given to Ali so small? 6. Considerations was given to administering IV heparin to Ali but this was considered unnecessary because he had been given rt.PA. Was this decision correct? 7. Following his MI, Ali had clinical evidence of HF and the long term prophylkactic treatment of his condition was considered. Which of the following drugs are likely to be of benefit: Low-dose aspirin, a B. blocker, An ACE inhiobitor, verapamil or deltiazem, Warfarin? Case 8; A 55-year-old man presents to his GP complaining of tightness of his chest when he digs the garden. It eases when he has a rest. On investigations, he has a raised serum glucose concentration and is considered to be a newly diagnosed NIDM. Questions; 1. What cardiovascular investigations should be done for him? 2. How can you treat this patient’ attacks? 3. How can you decrease the frequency and severity of his attacks? Case 9; The following patients are admitted for treatment of MI A. An asthmatic patient B. A man previously treated for infraction C. A patient with rheumatoid arthritis Questions 1. What are the contraindications or possible contraindications are there for the standard treatment of MI in the above people? References: 1. Medical pharmacology and therapeutics by Derek et al, 2005. 2. Modern pharmacology with clinical applications by Charles and Robert, 2004 3. Clinical pharmacy and therapeutics by Roger and Clive, 2004.