File
advertisement

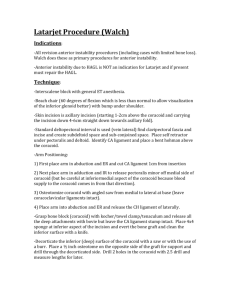
Bristow-Lataerjet Procedure for Anterior Shoulder Instability The shoulder or glenohumeral joint is an enarthrodial joint; commonly known as a balland-socket joint. The round head of the humerus articulates with the glenoid cavity which is shallow and relatively flat. It is deepened slightly by a fibrocartlaginous rim called the glenoid labrum. For this reason, stability of the shoulder is heavily dependent on the rotator cuff. The rotator cuff is made up of the subscapularis, infraspinatus, supraspinatus and teres minor. The infraspinatus and teres minor are responsible for external rotation. The supraspinatus is responsible to abduction and the subscapularis is responsible for internal rotation. Stability is also maintained in part by the long head of the biceps. The short head of the biceps brachii originates on the coracoid process. The coracoid process is located on the lateral edge of the anterior superior scapula. Over all the shoulder complex has high mobility but because of the sacrifices stability.1 The most common mechanism of injury for anterior subluxations and dislocations is when the arm is an abducted and laterally rotated position. When a force is applied posterior or lateral to the humerus or the joint is hyper extended, it can stress the anterior and inferior glenohumeral ligaments and the capsule. As they are stretched farther, and even torn, the humeral head is usually displaced anteriorly. It usually lodges between the anterior inferior glenoid rim and coracoid process.2 Chronic instability is classified by the direction of excessive translation of the humeral head. This could be anterior, inferior, posterior or multi directional. 2 “The Latarjet coracoid transfer procedure provides a “triple blocking” effect in the treatment of anterior shoulder instability. First, the coracoid bone block increases the anterior posterior diameter of the inferior portion of the glenoid fossa, making it more difficult for the Bristow-Lataerjet Procedure for Anterior Shoulder Instability humeral head to subluxate or dislocate. Second, the conjoined tendons act as a sling reinforcing the inferior capsular ligamentous complex and the inferior portion of the subscapularis. Finally, repair of the inferior capsular ligamentous complex to the stump of the coracoacromiai ligament reconstructs the capsulolabral anatomy.” 3 “The Bristow procedure and its variants, describes the transfer of the coracoid process through the subscapularis tendon as a method of treating recurrent anterior instability of the shoulder. The Coracoid tip is transferred to the anterioinferior glenoid neck and likely serves as a bone block in front of the humeral head. The transferred short head of the biceps and coracobrachialis are placed so as to produce a strong dynamic buttress across the anterior and inferior aspects of the joint when the shoulder is in the vulnerable abducted and externally rotated position.” 4 Using a limited deltopectoral approach, the skin incision starts at the tip of the coracoid and extends 3cm – 6cm towards the axillary. Next the cephalic vein is protected and laterally retracted. The deltoid is then split in order to make reaching the coracoid process and conjoined tendon possible. . Next a self-retaining retractor is inserted. This exposes the coracoid process from tip to insertion of the coracoclavicular ligaments at the base of the coracoid.2 “The coracoacromial ligament is sharply dissected from the lateral aspect of the coracoid and the pectoralis minor tendon insertion on the medial side of the coracoid is visualized.” 5 The pectoralis minor tendon insertion is released with the electrocautery from the coracoid process. The coracoacromial ligament is taken off at the level of its bony insertion. A Bristow-Lataerjet Procedure for Anterior Shoulder Instability hole with a 4.5mm diameter is then drilled into the middle of the coracoid perpendicular to its upper side. A 6.5 mm cancelous screw tap is then put through the hole. Finally a Pauwells osteotome is used to cut the coracoid at the coracoid knee.5 “Once the osteotomy of the coracoid has been performed, there is a clear view of the subscapularis tendon. The upper and inferior parts of the muscle are identified and 2 sutures are placed at its muscle and tendon junction to pull up the tendon in order to facilitate its incision.” 5 The subscapularis tendon is split horizontally at its lower part. This causes the upper part to retract. A 2.2 mm diameter k wire is hammered into the scapular neck. This is done as high as possible in order to maintain the retraction of the subscapularis tendon. Another K wire is put into the lower part of the glenoid neck to improve the exposure of the neck of the scapula. The capsule incision is performed simultaneously. Next the anterior inferior glenoid neck is prepared with osteotome to remove the top layer of the anterior surface.5 Positioning of the coracoid bone graft relative to the glenoid is crucial. Since it is not supposed to be a bone block, it must not be placed too far laterally or medially. It is placed so that it can function as an extension of the glenoid articular arc. Next a hole is drilled parallel to the joint line. It is about 1cm above the distal border of the glenoid rim. The hole is then filled with a cancelous screw tap. 5 A cancelous screw is then screwed into the bone block and then is pushed down with a screwdriver in order to put the tip of the screw into the glenoid hole. Then the graft is screwed into the right position. The subscapularis tendon is shut on the conjoined tendon. A stitch is then done between the conjoined tendon and the subscapularis. Finally a standard closing procedure is performed by using stitches to close the incision. 5 Bristow-Lataerjet Procedure for Anterior Shoulder Instability Post-operation care consists of the patient being in a shoulder immobilizer for one week. After one week the patient is then put in a sling for three to four weeks. Passive elbow flexion is encouraged but active and passive extension should be avoided because this stretches the bicep. 6 From month zero to one month post-surgery, the patient is in a sling except when performing the pendulum exercises. These exercises are to be done three times a day for 10 minutes. A soft ball may be squeezed as well as doing active scapular retraction with arms at the side of the body. 6 One of the immediate goals is to protect the repair. Another goal is to decrease inflammation and minimize pain. 7 Within the first six weeks a major goal is to gain passive range of motion. Starting week four post-surgery, passive range of motion will be worked on through many different exercises. Moist heat is used with a Swiss ball in order to work on flexion. Pulleys are also used for this. The uninvolved arm pulls one side down while the involved arm is raised passively. Supine flexion with a cane is also implemented at this time.3Sternal lifts are used to activate scapular refraction. Supine punches are also used to activate the scapula. Range of motion can also be gained through using an upper body ergometer. Short- term goals for this phase would be to externally rotate 25 to 30 degrees starting with 30 degrees of abduction and increase internal rotation to 45 degrees also with 30 degrees of abduction. These are all performed in the scapular plane. 7 Between weeks six and nine, the goal is to continue range of motion exercises while protecting the anterior capsule. At about eight weeks depending on progression of patient, Bristow-Lataerjet Procedure for Anterior Shoulder Instability open chain exercises may also be introduced. Supine cane flexion can be progressed to using a theraband. Also Supine abduction with a can be progressed to standing. Side lying exercises such as external rotation and abduction are two exercises. These provide range of motion exercises while using gravity as a form of resistance. 8 Biceps and triceps strengthening exercises would be added between weeks eight and ten depending on the patient’s progression, bicep strength is worked on by doing bicep curls with minimal weight.6 Triceps strength is worked on by doing triceps push downs with minimal weight and progressing to higher resistance. The goals for this phase are to have passive flexion to 80% of the uninvolved shoulder and to have passive external rotation within 10-15 degrees of uninvolved shoulder at 20 degrees of abduction. Criteria to continue to progress are no pain or substitutions and good shoulder mechanics. 7 During weeks 10 and 12 the goals are to improve strength, endurance and neuromuscular control.7 Weight is added to side lying exercise depending on patient’s tolerance. Push – ups using a table or wall would also be added to the patient’s program. 8 If there is full range of motion, normal joint mechanics and pain free movement by this time throwing motions may be implemented depending on if it is a functional activity for the patient.8 Difficulties would be range of motion in all planes initially. External rotation will have the biggest restrictions because this puts the patient at the biggest risk of dislocating again. 7 Internal rotation will need to be worked on due to the incision of subscapularis. The greatest strength loss would be with bicep flexion. This is expected because the biceps tendon is also Bristow-Lataerjet Procedure for Anterior Shoulder Instability moved when the coracoid process is moved. If problems with patient compliance arise, the most effective method to combat this is education. 7 Functional exercises would be incorporated based on what pain-free range of motion was achieved by the patient at each time. Functional exercises depend on the individual and what their goals are. Regardless of whether the individual is an athlete or not, activities of daily life would be the first functional exercises worked on. Activities such as pushing open a door, putting on a sweater/shirt or washing their hair would be functional for most patients. The long-term goals would be to perform tasks similar to these with no difficulty. 9 Next whatever is defined as functional for the individual would be worked on (return to play, work etc.). 9 The Bristow- Latarjet procedure is used to combat chronic anterior instability of the shoulder. This instability may be due to numerous dislocations or prior injuries. Even though this procedure helps the stability of the shoulder joint increase, the mobility of this joint will therefore decrease. Proper physical therapy must be prescribed and carried out in order for the patient to regain as much range of motion as possible.