PEDIATRICS UNIT 3 Revised 2010 Hematologic Disorders Anemia
advertisement
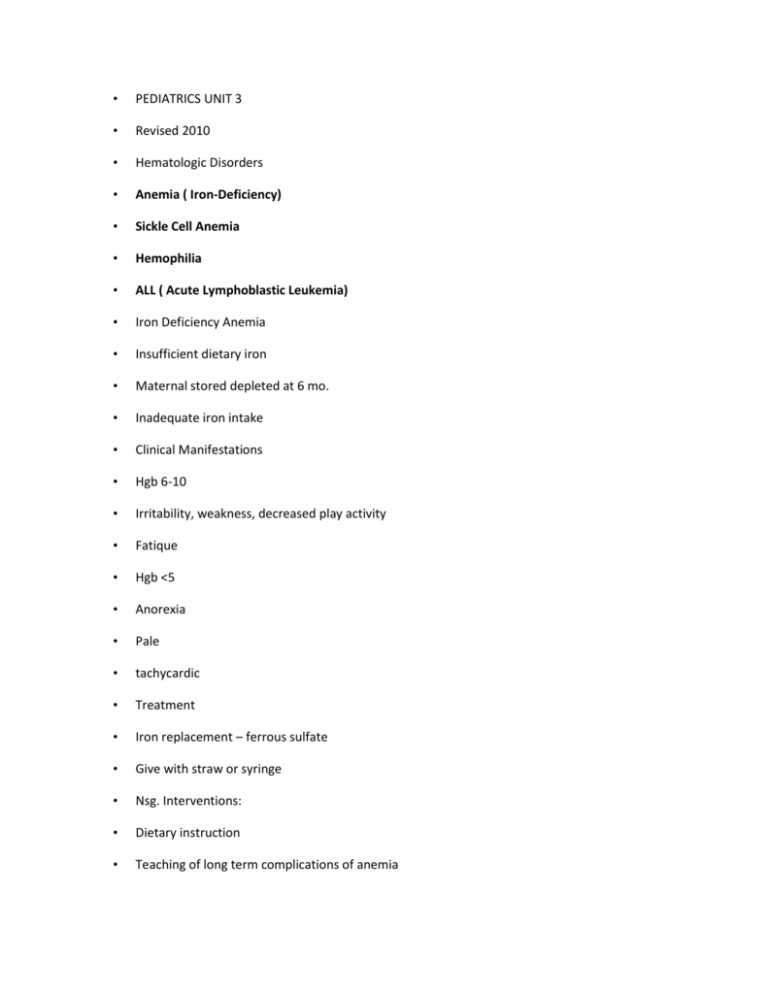
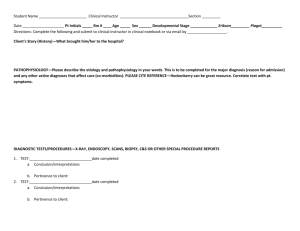
• PEDIATRICS UNIT 3 • Revised 2010 • Hematologic Disorders • Anemia ( Iron-Deficiency) • Sickle Cell Anemia • Hemophilia • ALL ( Acute Lymphoblastic Leukemia) • Iron Deficiency Anemia • Insufficient dietary iron • Maternal stored depleted at 6 mo. • Inadequate iron intake • Clinical Manifestations • Hgb 6-10 • Irritability, weakness, decreased play activity • Fatique • Hgb <5 • Anorexia • Pale • tachycardic • Treatment • Iron replacement – ferrous sulfate • Give with straw or syringe • Nsg. Interventions: • Dietary instruction • Teaching of long term complications of anemia • Sickle Cell Anemia • Inherited • African-American / Mediteranian • No cure • Sickling: • Clumping of abnormal shaped cells • Note: Sickle shaped cell in center of picture • Factors that precipitate a crisis • Infection • Dehydration • Cold • Emotional stress • Nursing Interventions • Hydration • Analgesics • O2 • Avoid precipitating factors • Coagulation Disorder • Hemophilia • Inherited – X linked • Lack clotting factors: • Factor VIII or Factor IX • s/s: • Bleeding • Bruising • Diag test: PTT • Tx: • Replace clotting factors • Nsg interventions: • Prevent injury • Family teaching • Neoplastic Disorder • Acute Lymphoblastic Leukemia • Increased blast cells • Decreased rbc’s and platelets • Tx: chemo • Nsg interventions: • Family support • Prevent infection • Monitor temp • Oral care • Nutrition • Immune Disorders • AIDS • RHEUMATOID ARTHRITIS • HIV/AIDS • Causes: • Maternal • Blood products • Sexual abuse • Tx: • Antiretroviral drugs • Nsg interventions: • Prevent infection • Nutrition / meds • Family support • Juvenile Rheumatoid Arthritis • Chronic inflammatory autoimmune connective tissue disease • Destroys cartilage • Clinical Manifestations • Stiffness, edema • Loss of motion • Warm to touch • Increase temp • Macula rash • Diagnostic Tests • Clinical findings • No specific tests • ESR • X-rays • Tx: • Preserve joint function • NSAIDS – SAARDS • Moist heat - PT • Nursing Interventions Balance rest / exercise • Pain management • Support groups • Respiratory Disorders • Respiratory Distress Syndrome • Lack surfactant to keep lungs expanded • Gestational age at birth influences severity • #1 s/s respiratory distress • Treatment Exogenous Surfactant O2 therapy Parenteral therapy • Pneumonia • Inflammation of lung tissue Most common cause: RSV = Respiratory Syncytial Virus • Tx: • O2 • Fluids • Nebs. • Nsg. Interventions: • Resp asses • Suction only if needed • Rest • Sudden Infant Death Syndrome • No cause • Occurs during sleep • Diagnosed on autopsy • Prevention: • “back to sleep” • Never prone • Nsg. Interventions • Family grief support • Allay feelings of guilt and blame • Acute Pharyngitis • “sore throat” • 80% viral • 20% strep – s/s: – Fever – Sore throat – White exudate • Diag test: strep throat culture • Tx: ABX if strep • Nsg. Interventions: • Antipyretics / analgesics • Saline gargle • Cool liquids p.o. • Tonsillitis • S/S same as pharyngitis Treatment : • 1)Same as pharyngitis 2) tonsillectomy • Pre-op: • Notify M.D. of any fever or abnormal assessment findings • Post-op: Semi prone • Monitor for bleeding • Analgesics • No straws • Laryngeotracheobronchitis • LTB = Croup • Viral • s/s: barking cough, tachypnea • retractions • Treatment • Maintain airway • Cool mist • NPO • Epinephrine • Nursing Assessment • Check for the 4 “D’s” 1) Drooling 2) Dyspnea 3) Dysphonia 4) Dysphagia • Epiglottitis • Cause: H influenzae bacteria • Life threatening airway obstruction • Signs & Symptoms Drooling High Fever Resp distress Muffled voice Progressive resp. distress Anxiety Fear • Treatment • Maintain airway • O2 • Eppi • ABX • IV fluids • Nursing Interventions ^ HOB Assess resp. status Freq. VS Trach tray @ bedside • Bronchitis • Usually viral • s/s: same as with URI + cough • Common during winter months • Children < 4 y.o. • Nsg interventions: • Cool mist • Fluids • Cough med • Cystic Fibrosis • Inherited • No cure • Excessive thick mucus produced • Obstructs lungs & GI system • s/s: steatorrhea • Barrel chest • Increased NaCl in sweat & saliva • Nsg interventions: • ^ nutrition • Pancreatic enzymes • CPT / postural drainage • Asthma • Common chronic childhood illness • Cause: allergy or hypersensitivity • Bronchospasm • Bronchial edema • s/s: SOB • Expiratory wheeze • tx: • Quick relief meds • Long term meds • Allergen testing • Nsg interventions: • ^HOB • Meds • hydration • Avoid triggers • Teach children self care and use of nebulizers • GASTROINTESTINAL DISORDERS • Cleft Lip / Cleft Palate • Facial malformation during fetal development • Cleft lip alone may feed without difficulty • Cleft palate and extensive cleft lip: • Difficulty feeding & speech • Psychological difficulty due to deformity • Tx.: • Surgical repair • Lip repaired at 1-2 mo. • Palate repaired by 1 yr • Nsg. Interventions: • Parental support • Assistive feeding devices • Post op care lip: • Breck feeder • Suture line care • Back or side lying • Post op care palate: • Semi prone • No straws, pacifier • No spoons • Follow up care: • Speech therapy • Observe for ear infections • Dehydration • Intake less then output • Determined by change in wt. • Infants and young children more easily effected • Diarrhea • Frequent liquid stools • Chronic • Acute • Infectious • Non-infectious • Tx: • Treat cause • Restore fluids and electrolytes • Modified BRAT diet, Pedialyte, • Rehydralyte, Infalyte • Nursing Interventions • I&O • Infection control • Nutrition • Daily weights • Gastroenteritis • Diarrhea caused by infection • Tx: • Same as for diarrhea plus • ABX • Constipation • Passage of hard infrequent stool • Structural disorders • Diet, meds • Repressed urge to defecate • Signs & Symptoms • Abd pain • Bloody stools • Decreased appetite • Treatment • Treat cause • Nursing Interventions • Educate parents • Stool and diet history • Bowel retraining • Hypertrophic Pyloric Stenosis • Hypertrophied pyloric muscle obstructs gastric outlet • Unknown etiology • Fig. 31-16 pg. 1028 • Signs & Symptoms • Projectile vomiting • Olive shaped mass, R. abd • Treatment • Surgical repair • Pyloromyotomy ( Fredet-Ranstedt procedure) • Intussusception • One part of intestine telescopes into another • s/s • Currant – jelly stool • Abd pain • Diag test: • Barium enema • Tx: barium enema • Surgical repair • Hirschsprungs Disease=Megacolon • Portion of colon lacks parasympathetic nerve cells • Signs & Symptoms • Vary acc. To age • Abd distention • Failure to pass meconium • Constipation & diarrhea • Decrease appetite • Two Stage Surgical Treatment • Temporary colostomy • Endo-rectal pull through • Nsg interventions: • Pre/post op care • Parent education • Colostomy care • Hernia • Organ protrudes through weakened muscle wall • Appendicitis • Inflammation of appendix • s/s • Rebound tenderness • Elevated WBC • Pain at McBurneys point • Gastroesophageal Reflux • s/s • Vomiting • Chronic cough • Heme. + stool • Tx: • Small frequent thickened feedings • Surgical repair • Nsg interventions: • Parent education • Pre/post op care • nutrition • Genitourinary Disorders • Nephrosis or Nephrotic Syndrome • Proteinuria • Edema • Hypoproteinemia • hyperlipidemia • s/s • Peri-orbital edema • Ascites • Generalized edema • Nsg interventions: • I&O • Skin care • ^pro. diet • Acute Glomerulonephritis • Inflammation of glomerulus • Most common cause: strep • s/s • Proteinuria • Tea colored urine • HTN • Tx: • Bedrest • Diuretics • Meds • Nursing Interventions • Bedrest • Restrict fluids & Na + • I&O • Wilms Tumor = Nephroblastoma • Most common malignant tumor of childhood • Develops from immature kidney cells • Prognosis greatly improved in recent decades • s/s: • Large, firm, asymptomatic abd mass • Do not palpate abd • Nursing interventions: • Pre/post op care • Family support • Structural Urinary Defects • Impact psychological well-being • Require prompt correction • See Table 31-3 • See Fig. 31-21 • Endocrine Disorders • Hypothyroidism = Cretinism • Lack thyroid hormones • Tx. Thyroid hormone replacement • Nsg. Intervention: • Teach parents importance of med administration to prevent cognitive & growth impairment • Diabetes Mellitus • Type I Diabetes (IDDM) • Lack insulin • Tx: • Insulin • Diet • exercise • Nsg interventions: • Family teaching • S/S of hyper / hypoglycemia • Blood glucose testing • Insulin admin. • Diet • Good control prevents complications