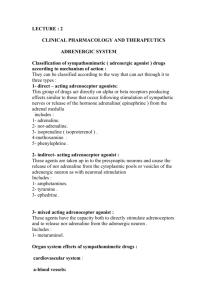
Autonomic Drugs
advertisement

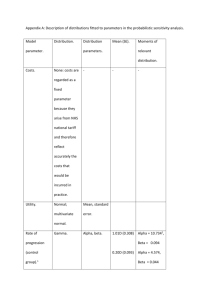
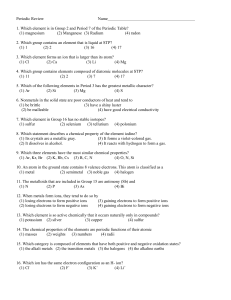
Autonomic Drugs 1. Muscarinic agonists may produce a. Mydriasis b. Vasodilatation c. Uterine contraction d. Bronchodilatation e. B and C <= 2. Effects of isoprenaline include: a. Reflex bradycardia b. Decreased peripheral resistance <= b1=b2>>>a so +ve chrono/ino and vasodilates leading to +ve CO and –ve BP c. Marked hypertension d. Reduced pulse pressure – reduced MAP e. A and C 3. In the eye a. Alpha adrenoceptors cause contraction of the circular papillary muscle - dilation b. Cyclospasm is a feature of organophosphate poisoning <= ciliary muscle contraction, opening the trabecular meshwork so useful in glaucoma (echothiophate, OGP, long duration of action) c. Beta agonist will reduce intraocular pressure – b blocker d. Antipsychotic agents such as chlorpromazine have no effect on the eye e. Diuretics have no use in glaucoma 4. Which agonist is not correctly paired with its adrenoceptor? a. Phenylephrine – alpha 1 b. Clonidine – alpha 2 – partial agonist c. Dobutamine – beta 1 – inotrope, minimal chronotopy, mild pressor d. Procaterol – beta 2 e. Prazosin – alpha 2 <=selective a1 blocker 5. Regarding beta-receptor antagonist drugs the following has no local anaesthetic action: a. Labetalol b. Atenolol <= hydrophillic b1 selective, renally excreted unchanged c. Metoprolol d. Propranolol e. Pindolol 6. regarding isoprenaline a. it is a potent bronchodilator <= b. it is a selective beta1 agonist – b1=b2 c. it can be used in tachyarrythmias to decrease AV conduction d. it has negative inotropic effects e. it causes peripheral vasoconstriction 7. regarding beta blockers a. inhibits renin release via beta2 receptors – b1 increases, a2 decreases b. metoprolol has intrinsic sympathomimetic effects c. all are well absorbed – esmolol IV only d. beta1 selective antagonists don’t cause bronchoconstriction – none are elective enough e. can treat ventricular tachycardia’s <= 8. IV drug that causes tachycardia, decreases diastolic BP, dilates pupil, doesn’t affect ejaculation, decreases sweating: a. Beta agonist b. Alpha antagonist c. Muscarinic antagonist <= d. Nicotinic antagonist e. Nicotinic agonist 9. Which has pure beta agonist effects in the circulation? a. Adrenaline b. Noradrenaline c. Isoprenaline <= b1=b2 d. ? e. ? 10. Choose the odd one out: a. Muscarine – agonist b. Acetylcholine – agonist c. Hyoscine <= is scolpolamine, a muscurinic antagonist d. Bethanachol – agonist e. ? 11. A young patient is given a normal dose of a drug in the emergency department. He develops tachycardia, increased BP and dilated pupils. The drug is most likely to be: a. Adrenaline <= b. Atropine - ? c. ? d. ? e. ? 12. dobutamine a. results in ATPàAMP b. can decrease systemic vascular resistance/afterload <= b1>b2>>>a, but complex. Is basically an inotrope with mixed a effects due to raemic mixture having opposing effects on alpha receptors. c. ? d. ? e. ? 13. regarding propranolol a. is a highly selective beta receptor antagonist – non-selective prototypical b. is poorly lipid soluble – highly, poor = atenolol c. has sodium channel blocking activity <= correct d. ? e. ? 14. A young man presents with dilated pupils, confusion and hyperpyrexia. Which of the following could not account for these effects a. Atropine b. Datura c. Morphine <= would constrict d. ? e. ? 15. pralidoxime acts to a. inhibit presynaptic acetylcholine release b. cleave organophosphates from acetylcholinesterase <= used for OGP poisoning w/ atropine nad benzos c. regenerate acetylcholine d. ? e. ? 16. A patient comes in staggering, agitated and hyperthermic with dilated pupils. Which is LEAST likely to be the cause? a. Atropine overdose b. Amphetamines c. Angels trumpet d. Tricyclic overdose – anticholinergic effects e. Aspirin overdose <= 17. benztropine causes: a. miosis b. diarrhoea c. confusion <= d. bronchorrhoea e. GIT haemorrhage 18. All of the following are characteristics of propranolol EXCEPT: a. Lipid soluble b. Local anaesthetic action c. Half life 3-6 hours d. Beta sympathetic selectivity <= is is b1=b2>>>>a e. 30% bioavailability 19. regarding prazosin, which is NOT true? a. It is a selective alpha 1 blocker - true b. It dilates arterioles only, not veins <= both arteries and veins c. It undergoes extensive first pass metabolism – 50% BA d. Recipients may develop a positive test for anti-nuclear factor e. With negative feedback of noradrenaline on its own, release can still occur 20. dopamine a. has less alpha agonist effect than dobutamine – dobutamine is b1>b2>>>a,, dopamine D1=D2>>b>>a (at high doses mimicks adrenaline) b. dilates the renal vascular bed by its action of beta 1 receptors – D1 c. causes a profound rise in peripheral vascular resistance d. is inactivated by sodium bicarbonate <= e. causes vasoconstriction at all doses 21. propranolol a. has no central effects b. can be used safely in type I respiratory failure because of its reliable beta 1 selectivity c. in overdose may be effectively treated by administering glucagons <= d. needs to be given in relatively large oral doses because of its poor absorption e. does not produce withdrawal symptoms on abrupt cessation because beta receptors do not up regulate 22. hyoscine a. may potentiate the anticholinergic effects of phenothiazines – additive effects? b. is well absorbed from the gastrointestinal tract <= true, delayed effect via transdermal patch c. readily crosses the blood brain barrier - ? d. has its main effect at nicotinic receptors e. produces pronounced tachycardia in therapeutic doses 23. beta blockers a. are class III antiarrythmic drugs - 2 b. are selective for beta 1 adrenoreceptors c. are useful agents in acute heart failure d. may mask the symptoms of hypoglycaemia <= by blunting the adrenaline response w/ tremor and palpitations AND may make the hypoglycaemia last longer e. are particularly safe and effective in combination with verapamil 24. atropine a. causes ureter and bladder wall contraction b. acts by blocking adrenoceptors c. is an example of a surmountable blockade <= d. results in miosis e. causes bradycardia in a moderate to high therapeutic dose – brady then tachy 25. noradrenaline a. is more potent than salbutamol at beta 1 receptors b. is less potent than isoprenaline at alpha receptors – isopren is b1=b2>>>a c. antagonizes the effects of dopamine d. has similar potency to adrenaline at beta 1 receptors <= e. is less potent than adrenaline at alpha receptors 26. which of the following drugs utilises camp as a second messenger? a. Adrenaline b. Dopamine c. Milrinone d. Glucagons e. All of the above <= 27. which of the following statements is incorrect? a. Noradrenaline and adrenaline exert beta effects at low doses and alpha effects at high doses b. Dobutamine exerts its actions via alpha effects <= b1>b2>a c. Inotropic agents act ultimately by increasing intracellular calcium d. Dopamine exerts different effects at different doses e. Theophylline is a positive inotrope 28. milrinone a. has a short half life because of rapid reuptake and breakdown intravascularly by COMT b. is extensively metabolized by the liver – 12% c. is in the same class of drugs as dobutamine – it is a phosphodiesterase inhibtior d. is a competitive inhibitor of phosphodiesterase <= increasing cAMP, Ca2+ and therefore contractility , also vasodilation e. is one of the most commonly used inotropes in the intensive care setting 29. alpha-adrenoceptors utilise a. camp as a second messenger – a2 decrease cAMP b. cGMP as a second messenger c. phosphodiesterase inhibition to achieve positive inotropic effects d. phospholipase C to achieve positive inotropic effects <= a1 via PLC -> IP3 and DAG e. a second messenger system that is yet to be discovered 30. beta 1 effects include a. positive inotropy <= b. peripheral vasoconstriction c. bronchodilation d. peripheral vasodilation e. a and b only 31. the following statements are true for catecholamines, EXCEPT: a. they all have a very short half life b. noradrenaline is used mainly when peripheral vasoconstriction is desirable c. dopamine in doses od <2mcg/kg/min has been proven to directly improve renal perfusion <= ??? d. dobutamine is a synthetic derivative of isoprenaline e. they increase myocardial contractility at the expense of increased oxygen consumption 32. Which of the following drugs does not cause the same effect? a. Muscarine b. Acetylchoine c. Hyoscine <= d. Carbachol e. Methacholine 33. A young man is injected with an IV drug. He shows a resultant tachycardia, midriasis, normal blood pressure and reduced sweating. The most likely drug is a. Nicotinic antagonist b. Muscarinic antagonist <= c. Cholinomimetic d. Adrenergic agonist e. Adrenergic antagonist 34. The most lipid soluble beta blocker is a. Propranolol <= b. Atenolol c. Metoprolol d. Pindolol e. Sotalol 35. propranolol a. is a highly selective beta receptor antagonist b. is poorly lipid soluble c. has sodium channel blocking action <= d. has intrinsic sympathomimetic activity e. has an oral bioavailability of >50% 36. the cholinesterase inhibitor with the shortest duration of action is a. physostigmine b. edrophonium <= c. neostigmine d. parathion e. malathion