cea12468-sup-0001-tableS1-S3
advertisement

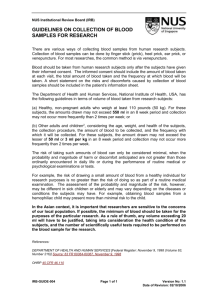
Appendices Table A1: Non-irritating test concentrations for beta-lactam antibiotics (reproduced with permission from Brockow et al. 2013) Drug SPT IDT PT Penicilloyl-poly-L-lysine 5 x 10-5 mM 5 x 10-5 mM NA Minor determinant mixture 2 x 10-2 mM 2 x 10-2 mM NA Benzylpenicillin 10.000 UI 10.000 UI 5% Amoxicillin 20 mg/ml 20 mg/ml 5% Ampicillin 20 mg/ml 20 mg/ml 5% Cephalosporins 2 mg/ml 2 mg/ml 5% SPT, skin prick test; IDT, intradermal test; PT, patch test Table A2: Examples of increasing drug doses during provocation, modified from Messaad and colleagues [150] Drug Doses1 Route Usual daily dose for adults Amoxicillin 25,100,500,1000 Oral 1000 to 2000mg Ampicillin 25,100,500,1000 Oral 2000mg Cefaclor 25,125,500 Oral 750mg Cefadroxil 25,100,500,1000 Oral 2000mg Cefuroxime 20,80,400 Oral 500mg Ceftazidime 25,100,500,2000 IV 3000mg Cefixime 25,100,225 Oral 400mg Ceftriaxone 25,100,500,1000 IV 1000-2000mg 1 Messaad and colleagues give a starting dose of 1 and 5 mg, however, current practice is to start at the higher dose as given in the table. Table A3: Penicillin oral desensitisation protocol (Adapted from Sullivan [210]) Step 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Penicillin stock concentration (mg/ml) 0.5 0.5 0.5 0.5 0.5 0.5 0.5 5 5 5 50 50 50 50 Amount (ml) Dose (mg) Cumulative dose (mg) 0.1 0.2 0.4 0.8 1.6 3.2 6.4 1.2 2.4 5 1 2 4 8 0.05 0.1 0.2 0.4 0.8 1.6 3.2 6 12 25 50 100 200 400 0.05 0.15 0.35 0.75 1.55 3.15 6.35 12.35 24.25 49.35 100 200 400 800 Intervals between doses was 15min Appendix B: Clinical Audit: Assessment of penicillin allergy 1. Do you undertake beta-lactam allergy testing in your centre? a. Yes b. No 2. Which statement(s) best describe why beta-lactam testing is not performed in your centre? a. An accurate history is adequate to make a diagnosis b. Skin testing is inaccurate and therefore not a useful tool c. Our centre does not have the time or facilities d. Our centre does not have the financial support e. Numerous other antibiotics are available 3. How many patients are seen for penicillin testing in an average year? a. 0-5 b. 6-10 c. 11-20 d. >20 4. What category of patients do you review for penicillin allergy? a. Adults only b. Paediatrics c. Adults and paediatrics 5. Which circumstance best describes why a RAST test would be performed? a. At all initial consultations b. Only if history is supportive of allergy c. Only if history is inconclusive d. Only if skin testing is negative e. Only if skin testing is positive 6. Which of the following RAST tests do you perform in your centre? (Please tick as many choices as appropriate) a. Penicillin V b. Penicillin G c. Amoxycillin d. Ampicillin e. Other (please specify) 7. Does your centre perform skin testing? a. Yes b. No 8. Would any of the following conditions preclude your centre from performing skin testing? (Please check multiple conditions if appropriate) a. Stevens-Johnson Reaction b. Toxic epidermal necrolysis syndrome c. Chronic urticaria d. Atopic dermatitis e. Dermographism f. Mastocytosis 9. Does your centre perform the following skin testing methods? (please check multiple answers if appropriate). a. Skin prick testing alone b. Intra-dermal testing alone c. Skin prick followed by intra-dermal testing if negative or indeterminate skin prick test d. Skin prick followed by intra-dermal testing in all cases e. Patch testing 10. What reagents does your centre use for skin testing? a. Diater (DPT) penicillin kit b. In house kit c. Whole drugs at known non irritant concentrations 11. Which drugs does your centre routinely use for skin prick testing? (Please check multiple answers if appropriate) a. Penicillin PPL (major) determinant b. Penicillin MDM (minor) determinant mix c. Amoxycillin d. Benzylpencillin e. Flucloxacillin f. Co-amoxiclav g. Cephalosporin (please specify in other) h. Other please specify 12. What drugs and concentrations does your centre use for intra-dermal testing? (Please check the lowest dilution that most closely applies to your regimen assuming the stated standard doses). Penicillin PPL (major) determinant (manufacturer's instructions) Penicillin MDM (minor) determinant (manufacturer's instructions) Amoxycillin 250mg/ml Benzylpenicillin 100,000 Mu/ml (60mg/ml) Yes No Specify Dose Yes No Specify Dose Yes No Yes No Specify Dose Specify Dose Other please specify 13. Which of the following questions are true of your intra-dermal test (IDT) practice? a. IDT performed at one dilution only b. IDT performed at increasing concentrations, once lower dilution shown to be negative c. IDT performed at one dilution and repeated at a lower dilution if positive 14. Has a systemic allergic reaction occurred following skin testing at your centre? a. Yes b. No 15. What method of skin testing have reactions occurred to? (please check more than one choice if appropriate) a. Skin prick test b. Intra-dermal test c. Uncertain 16. How many patients have experienced systemic reactions in the last five years following skin testing? a. 0 b. 1-5 c. 6-10 d. >10 17. Which set of symptoms best describe the worst reaction to skin testing in your centre? a. Grade I: generalized urticaria, mild lip and periorbital swelling, pruritus, nausea, anxiety b. Grade II: any grade I symptom plus angioedema, or two or more of the following: tightness, vomiting, diarrhoea, abdominal cramps, and dizziness c. Grade III: any grade I or II symptom plus dyspnoea, wheezing, or stridor or two or more of the following: dysphagia, dysarthria, hoarseness, general weakness, numbness, or fear of death d. Grade IV: any grade I, II, or III symptom plus two or more of the following: a drop in blood pressure, collapse, syncope, incontinence, or cyanosis e. Death 18. Does your centre perform drug provocation testing (DPT)? a. Yes, in all patients with no demonstrable specific IgE b. Yes, but only in 'selected patients' (please briefly describe criteria below) c. No, I am happy to reassure on the basis of absence of detectable specific IgE d. No, facilities and resources are not available Briefly describe criteria: 19. Do you have specific criteria for stopping a direct provocation test? a. Yes b. No 20. How does your centre monitor for delayed reactions? a. Patients are not routinely monitored b. Routinely review patients in clinic at 48/72 hours c. Ask the patient to contact clinic if there is a reaction to DPT or IDT d. Ask the patient to photographically record any reaction to DPT or IDT e. Patch testing is performed f. The patient is prescribed a course of drug g. Other (please specify) 21. Does your centre provide emergency treatment to be taken home in case of an allergic reaction? a. Yes b. No 22. After completing all investigations do you invite patients to return to check for resensitisation? a. Yes b. No 23. What procedure(s) do you perform to check for re-sensitisation? a. Skin prick test b. Intra-dermal test c. Drug provocation test 24. What is the interval between initial testing and retesting? a. <1 month b. 1-2 months c. 2-4 months d. 4-6 months e. > 6 months f. Other (please specify) 25. Why does your centre not assess for re-sensitisation? a. It is unnecessary b. Resources do not permit re-evaluation c. Other (please specify) 26. Which drugs do you advise avoiding following a positive test during beta-lactam testing? a. All penicillins b. 1st and 2nd generation cephalosporins c. All cephalosporins d. Carbopenems e. Monobactams f. Other (please specify) 27. If sensitisation to amoxicillin is demonstrated without specific IgE to penicillin determinants do you test for tolerance to penicillin by direct provocation testing? (to determine side chain reactors). a. Yes b. No