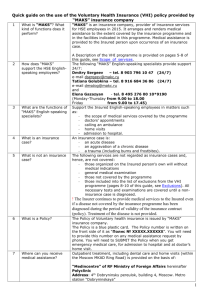
Exclusions from the VHI programme 2015
advertisement

Exclusions from the VHI programme 2015 The Insurance company does not cover the costs of medical services rendered to the Insured for the following diseases and/or their consequences and aggravation (after diagnose is established) unless the insurance programme otherwise provide: I. - - II. - - - Coverage of medical services for the following diseases and their aggravation: malignant oncological diseases, central nervous system neoplasms, malignant blood and hematopoietic diseases; congenital and hereditary diseases, congenital anomalies (organs and tissues malformations), chromosomal disorders and abnormalities; epilepsy and epileptic syndrome; mental and behavioral disorders, including alcohol, drug and toxic substance abuse; HIV and AIDS, venereal diseases (syphilis, gonorrhea, chancroid (soft chancre), lymphogranuloma venereum, venereal granuloma; STDs, including chlamydia infection, ureaplasmosis, mycoplasma, genital herpes, cytomegalovirus infection, gardnerella vaginalis, human papillomavirus (HPV)), beyond the limit covered by insurance programme; type 1 and 2 diabetes mellitus (except for outpatient care); acute and chronic viral hepatitis (except for hepatitis A and E), hepatic fibrosis and cirrhosis; tuberculosis, sarcoidosis, amyloidosis, psoriasis, deep (systemic) mycoses, onychomycosis; diseases accompanied by chronic renal and hepatic failure, requiring extracorporeal treatment; systemic autoimmune skin and connective tissue diseases, deforming dorsopathies (except for osteochondrosis), inflammatory polyarthropathies, arthrosis (except for posttraumatic arthrosis), Bechterew's disease; multiple sclerosis, Parkinson disease, other extrapyramidal and movement disorders; acute and chronic radiation sickness; occupational diseases. Coverage of the following medical services: Services not stipulated in the insurance contract, without doctor’s prescription, at the discretion of the Insured; treatment of pathological states and injuries arising from or related to alcohol, drug and other substance abuse and its residual effects, and in states caused by psychoactive substances; visits and consultations of specialists, diagnostic examination, procedures and other services connected with pregnancy and its complications (including abortion), except for emergency assistance within the scope of services provided in case of ectopic pregnancy, metrorrhagia during the first trimester, antenatal care and childbirth, postpartum condition and/or diseases and their complications; visits and consultations of specialists, diagnostic examination, procedures and other services for family planning, procedures for impregnation or its prevention, including artificial insemination or in-vitro fertilisation, drug contraception and surgical sterilization; infertility diagnostics and treatment, erectile dysfunction (including impotence, peyronie's disease), other sexual dysfunction; genetic tests; procedures on caries treatment of teeth if more than ½ of the crown is destroyed (as of the first diagnostic and therapeutic visit to a specialist, after dental cavity preparation) and on teeth with prosthetic and orthodontic devices (except for emergency acute pain relief for acute inflammation or trauma); treatment of noncarious tooth defects (wedge-shaped tooth defects, dental enamel erosion and hypoplasia); diagnostics, treatment and elimination of orthodontic defects; preventive (dental fissure sealing, plaque and calculus removal, fluoride-containing - - - - - - - - dental preparations and lacquer application, and the like) and cosmetic (cosmetic teeth restoration, including veneers and laminates, teeth whitening, and the like) procedures, including filling replacement without medical reason and beyond the limit covered by insurance programme; visits and consultations of specialists, diagnostic examination, procedures concerning prosthodontics and preparation for it, including removal of tooth pulp, dental extraction, implant dentistry and preparation for it; preventive and surgical treatment of parodontium tissue beyond the limit covered by insurance programme; visits to specialists for diagnostics and treatment of condyloma, trichopathy, and dermatopathy such as calluses, warts, papilloma, molluscum contagiosum, nevus, hyperkeratosis; skin flaws correction, including for improving mental health of the insured; diagnostics and treatment in medical institutions involving original techniques not stipulated in the insurance contract; hydrocolonotherapy, hydrotherapy and pelotherapy (except provided within restorative (health resort) treatment); dry immersion therapy; mechanical therapy, shockwave therapy, mechanic massage, course treatment of chronic diseases involving programme device treatment (“Andro-Gin”, “Yarilo”, “Multiamg”, programme complexes in ophthalmology and the like, kinesitherapy, “Gemocode” test and the like, and other methods beyond the limit covered by insurance programme; visits to specialists: kinesiotherapist, nutritionist, geneticist, speech therapist, psychologist, speech-language pathologist, phoniatrician, somnologist beyond the limit covered by insurance programme; psychotherapy and computer psychodiagnostics; specific allergen testing (skin tests, standard and/or individual allergen panel testing, except provided in cases of emergency admission and specific hyposensitisation therapy, including SIT (Specific immunotherapy); clinic and laboratory diagnostics and treatment of immune system diseases beyond the limit covered by insurance programme; diagnostics and treatment (including procedures) for cosmetic reasons and aesthetic purposes, or for improving mental health of the insured; weight management, veins sclerotherapy, colon therapy; any medical and other services for recreational, cosmetic and preventive purposes; diagnostics and treatment of eating disorders (obesity, binge eating, undernutrition) and osteoporosis; diagnostics and treatment of rhonchopathy and sleep apnea; foot deformity, including platypodia; spine curvature disorders treatment; traditional medicine for diagnostics (acupuncture, auricular, thermoacupuncture, electroacupuncture, manual, energoinformational diagnostics, iridology, pulse diagnosis and he like) and treatment (hirudotherapy, homeopathy, phytotherapy, apitherapy, chromotherapy, and the like) and recreation (chi kung, breathing practices, music therapy, and the like); extracorporeal blood treatment (including programmed hemodialysis, endovenous laser therapy, and the like), except for the cases of extracorporeal blood treatment upon medical condition in critical care unit; ozone therapy; hypobaric, normobaric and hyperbaric oxygenation, except for cases of hyperbaric oxygenation upon medical condition in critical care unit; preparation for planned inpatient treatment, if the insurance programme does not provide for “planned inpatient treatment”; diagnostics and treatment within “day hospital” basis or a “one day hospital” basis, if the insurance programme does not provide for “planned inpatient treatment”; regular medical check-up of the insured with chronic diseases and higher risks for certain disease; - - - services beyond the limit covered by insurance programme concerning individual risks (types of medical assistance); The Insurance Company does not cover: organs and tissues transplantation (implantation); corrective eye surgery, including laser surgery; hearing aid (lost hearing restoration with hearing aids – diagnostics, choice, support and service), cochlear implants); septoplasty; submucosal resection of nasal septum; elective neurosurgery treatment; elective reconstructive surgery, including in cases of disease and anomalies of cardiovascular and musculoskeletal systems; elective surgery of spinal disk herniation (protrusion); orthopedic prosthetics (restoring functions of lost or missing organs and body parts) – limbs, joints, eyes, teeth, and the like); pacemakers, prostheses, endoprostheses, implants, osteosynthesis and fixation plates, angiography, angioplasty and stenting sets (except for vena cava filter placed in emergency cases), medical equipment, medical appliances for eyesight and hearing correction, medical appliances and expendables for treatment of patients with any diseases; certificates and other medical documents for swimming pools, sports, recreation activities; for obtaining driver and firearms license; for health resorts, sanatoriums, children recreation centres, health resort records (except if the insurance programme covers restorative (health resort) treatment); certificates and medical documents for any other purposes unless the insurance programme otherwise provide.