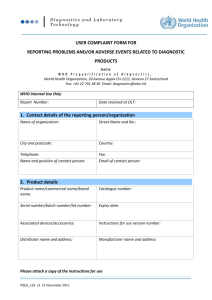
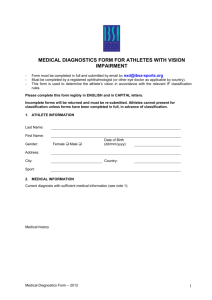
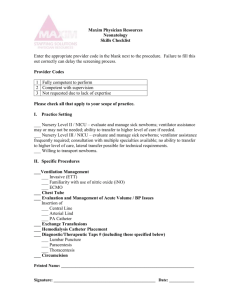
Method. instructions
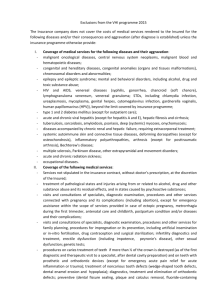
advertisement

Dnepropetrovsk State Medical Academy Hospital pediatrics department №1 Methodological instructions for 5th course students of pediatrics Module 2 Neonatology. Blood and endocrine diseases at children Dnepropetrovsk 2009 1 Author’s staff: Chief of department V.A. Kondratyev, k.med.s. Vakylenko L.I. Confirmed on departments meeting « 15 » September 2009, report № 2 Confirmed on Central methodological commission of DSMA «___»______________2009, report № ___ 2 Contents • INTRODUCTION • THE PURPOSE OF STUDYING OF THE SUBJECT • THE CURRICULUM CONTENTS • THE THEMATIC PLAN OF THE PRACTICAL CLASSES • THE TECHNIQUE OF ESTIMATION OF STUDENTS’ CURRENT KNOWLEDGE • THE FINAL MODULAR CONTROL • THE LIST OF THE MONITORING METHODS • METHODICAL INSTRUCTIONS FOR STUDENTS’ WORK DURING PRACTICAL CLASSES • APPENDICES 3 INTRODUCTION In connection with introduction in system of the higher medical education of creditmodular system of training, there were changes of distribution of hour loading between in-class and out-of-class sections of students’ preparation. Reduction in-class parts of training against increase of requirements to quality of experts’ preparation causes necessity of optimisation of educational process during a practical training. The teaching-methodical books on pediatrics for students of the 5th courses include the basic methodical approaches to studying and mastering of program themes of discipline and corresponds to the typical program confirmed by Ministry of Public Health of Ukraine (Kiev, 2008). The teaching-methodical books are intended for the students of „medical department”, "pediatrics", „medico-preventive department”. THE PURPOSE OF STUDYING THE SUBJECT Final goals of a subject "pediatrics" are based on base of the educational purposes stated in the educational professional program (EPP). They are defined in the following way: 1.To define aetiological and pathogenetic factors of blood and endocrine diseases at children, illnesses of newborns. 2. To classify and analyze a typical clinical picture of the most widespread diseases of blood and endocrine diseases at children, illnesses of newborns. 3. To reveal features of diseases of newborn children. 4. To make the plan of inspection and to analyze the data of laboratory and instrumental investigations at a typical clinical course of diseases of endocrine and hematopoietic systems at children, illnesses of newborns. 5. To show skills in treatment principles, rehabilitation and preventive measures of illnesses of newborn and most widespread diseases of endocrine and hematopoietic systems at children. 6. To diagnose and to render the emergency aid at the basic urgent conditions at newborns and at children with the most widespread diseases of endocrine and hematopoietic systems. 7. To carry out differential diagnostics and to make the preliminary diagnosis at a typical clinical course of illnesses of newborns and diseases of endocrine and hematopoietic systems at children. 8. To carry out an estimation of the prognosis of diseases of endocrinen and hematopoietic systems at children, illnesses of newborns. 9.To show skills in morally-deontological principles of the medical expert and principles of a professional subordination in pediatrics. The SUBSTANTIAL MODULE 7. Preterm infants Specific goals: 1. To define etiological factors of newborn prematurity. 2. To classify and analyze a typical clinical picture of various degrees of a morphological and neuro-functional maturity of preterm infants. 3. To define features of adaptation of preterm infants and to diagnose desadaptation syndromes. 4. To make the plan of investigation and to analyze the data of laboratory and instrumental investigation of preterm infants. 4 5. To demonstrate the possession of nursing principles of preterm infants, treatment and preventive measures of desadaptation syndromes, rehabilitation of preterm infants. 6. To make the diagnosis and to render the emergency help at the basic urgent conditions at preterm infants: respiratory failure, enteroparesis, hyperbilirubinemia, hypoglycemia. 7. To carry out differential diagnostics of hyperbilirubinemia at preterm infants and to make the preliminary diagnosis. 8. To carry out the life forecast of preterm infants. 9. To show the possession of etiko-deontological principles of the medical expert and principles of a professional subordination in neonatology. Theme 1. Features of adaptation, the nursing and feeding organisation of newborns. Preterm infants. Etiological factors of prematurity. Anatomo-physiological features. Degrees of morphological and neurofunctional maturity of preterm infants. Features of adaptation of preterm infants and desadaptation syndromes. Differential diagnostics of hyperbilirubinemia at preterm infants. A delay of intrauterine fetal growth: the causes, diagnostics, treatment, preventive measures. Nursing principles of preterm infants in maternity hospital and at the second stage of nursing. Features of feeding strategies for preterm infants. The urgent help at the basic urgent states of preterm infants: respiratory insufficiency, парезе intestines, hypoglycemia, hyperbilirubinemia. The SUBSTANTIAL MODULE 8. The Most widespread noninfectious diseases of newborns Specific goals: 1. To define etiological and pathogenetic factors of asphyxia and birth trauma of newborns, respiratory diseases at newborns, hemolytic and hemorrhagic diseases of newborns. 2. To classify and analyze the typical clinical picture of asphyxia and birth trauma of newborns, respiratory diseases at newborns, hemolytic and hemorrhagic diseases of newborns. 3. To define features of the course of asphyxia and birth trauma of newborns, respiratory diseases at newborns, hemolytic and hemorrhagic diseases of newborns and to make the preliminary clinical diagnosis. 4. To make the plan of investigation and to analyze the data of laboratory and instrumental investigation at the typical course of asphyxia and birth trauma of newborns, respiratory diseases at newborns, hemolytic and hemorrhagic diseases of newborns and to make the preliminary clinical diagnosis. 5. To show the possession of principles of treatment, rehabilitation and preventive measures of asphyxia and birth trauma of newborns, respiratory diseases at newborns, hemolytic and hemorrhagic diseases of newborns and to make the preliminary clinical diagnosis. 6. To make the diagnosis and to render the emergency help at the basic urgent conditions at newborns, having manifestations of asphyxia and birth trauma of newborns, respiratory diseases at newborns, hemolytic and hemorrhagic diseases: the syndrome of intracranial hypertension, convulsive syndrome, аpnea, bradycardia, enteroparesis, respiratory insufficiency, syndrome of meconial aspiration and bleedings at newborns. 5 7. To carry out differential diagnostics of asphyxia and birth trauma of newborns, respiratory diseases at newborns, hemolytic and hemorrhagic diseases of newborns and to make the preliminary clinical diagnosis. 8. To carry out the life forecast at asphyxia and birth trauma of newborns, respiratory diseases at newborns, hemolytic and hemorrhagic diseases of newborns 9. To show the possession of etiko-deontological principles of the medical expert and principles of a professional subordination in neonatology. Theme 2. Asphyxia of the newborn. Aetiology. Pathogenesis. Classification. Clinical manifestations. Diagnostics. Differential diagnostics. Primary resuscitation of newborns. Treatment. Preventive measures. Prognosis. Theme 3. Birth trauma. Aetiology. Pathogenesis. Classification. Clinical manifestations. Diagnostics. Differential diagnostics. Treatment. Preventive measures. Prognosis. Theme 4. Respiratory diseases at newborns. Aetiology. Pathogenesis. Classification. Clinical manifestations. Diagnostics. Differential diagnostics. Treatment. Preventive measures. Prognosis. Theme 5. Haemolytical and hemorrhagic diseases of newborns. Aetiology. Pathogenesis. Classification. Clinical manifestations. Diagnostics. Differential diagnostics. Treatment. Preventive measures. Prognosis. The SUBSTANTIAL MODULE 9. Congenital infections Specific goals: 1. To define etiological, pathogenetic factors and risk factors of congenital infections at newborns. 2. To classify and analyze the typical clinical picture of perinatal infectious diseases at newborns: intrauterine (congenital) infection, local and generalised infection. 3. To define features of perinatal infectious diseases at newborns (congenital infection, local and generalised infection) and to make the preliminary clinical diagnosis. 4. To make the plan of investigation at perinatal infectious diseases at newborns (congenital infection, local and generalised infection) and to analyze the data of laboratory and instrumental investigations at their typical course. 5. To show the possession of treatment principles, rehabilitation and preventive measures of perinatal infectious diseases at newborns (congenital infection, local and generalised infection). 6. To make the diagnosis and to give the emergency help at acute respiratory failure, acute renal failure, convulsive syndrome, necrotic enterocolitis, syndrome of disseminated intravascular coagulation at perinatal infectious diseases in newborns. 7. To carry out differential diagnostics of perinatal infections and to make the preliminary diagnosis. 8. To carry out the life forecast at perinatal infectious diseases of newborns (congenital infection, local and generalised infection). 6 9. To show the possession of etiko-deontological principles of the medical expert and principles of a professional subordination in neonatology. Theme 6. Congenital infections of the newborn (TORCH – infections) Classification, aetiology, pathogenesis, clinical manifestations, diagnostics, differential diagnostics, treatment, preventive measures end prognosis. Theme 7. Bacterial infections of the newborn. Pyoinflammatory diseases of the skin and subcutaneous basis, diseases of umbilical cord, umbilical wound and umbilical vessels: classification, aetiology, pathogenesis, clinical manifestations, diagnostics, differential diagnostics, treatment, preventive measures end prognosis. A sepsis of newborns: classification, aetiology, pathogenesis, clinical manifestations, diagnostics, differential diagnostics, treatment, preventive measures end prognosis. The SUBSTANTIAL MODULE 10. Blood diseases at children Specific goals: 1. To define etiological and pathogenetic factors of anemias of deficiency, leukaemias and lymphomas, hemophilias, thrombocytopenias and thrombocytopathies at children. 2. To classify and analyze the typical clinical picture of anemias of deficiency, leukaemias and lymphomas, hemophilias, thrombocytopenias and thrombocytopathies at children. 3. To define clinical features of of anemias of deficiency, leukaemias and lymphomas, hemophilias, thrombocytopenias and thrombocytopathies at children and to make the preliminary clinical diagnosis. 4. To make the plan of investigation and to analyze the data of laboratory and instrument investigations at the typical course of anemias of deficiency at children, at the typical course of leukaemias and lymphomas at children, at the typical current of a hemophilia, thrombocytopenias and thrombocytopathies at children. 5. To show the possession of principles of treatment and prophylaxis of deficiency anemias, treatment, prophylaxis and rehabilitation of leukaemias and lymphomas, hemophilias, thrombocytopenias and thrombocytopathies at children. 6. To make the diagnosis and to render the urgent help at acute bleeding, hemorrhagic shock and the syndrome of squeezing at children. 7. To carry out differential diagnostics of deficiency anemias, leukaemias and lymphomas, hemophilias, thrombocytopenias and thrombocytopathies with other blood diseases at children. 8. To carry out the life forecast at deficiency anemias, leukaemias and lymphomas, hemophilias, thrombocytopenias and thrombocytopathies at children. 9. To show the possession of etiko-deontological principles of the medical expert and principles of a professional subordination in pediatrics. Theme 8. Iron -, protein - and vitamin-deficiency anemias at children. Aetiology. Pathogenesis. Classification. Clinical manifestations. Diagnostics. Differential diagnostics. The urgent help at bleedings Treatment. Preventive measures. Prognosis. 7 Theme 9. Childhood hemoblastoses. Leukaemias and lymphomas at children. Aetiology. Pathogenesis. Classification.. Diagnostics. Differential diagnostics with other blood diseases which is accompanied by hyperplastic syndrome. Treatment. The urgent help at hemorrhagic syndrome and the syndrome of squeezing. Prognosis. Theme 10. Haemorrhagic diseases at children Hemophilia, thrombocytopenias and thrombocytopathies at children. Aetiology. Pathogenesis. Classification.. Diagnostics. Differential diagnostics with other hemorrhagic conditions at children. Treatment. The urgent help at bleedings and hemorrhagic conditions. Prognosis. The SUBSTANTIAL MODULE 11. Endocrine disorders at children Specific goals: 1. To define etiological and pathogenetic factors of development of diabetes mellitus, diffuse toxic goiter, hypothyroidism, autoimmune thyreoiditis, endemic goiter at children; various clinical forms of growth disturbances, obesity, pubertal dyspituitarism, various forms of genital glands disturbances. 2. To classify and analyze the typical clinical picture of diabetes mellitus, diffuse toxic goiter, hypothyroidism, autoimmune thyreoiditis, endemic goiter at children; various clinical forms of growth disturbances, obesity, pubertal dyspituitarism, various forms of genital glands disturbances. 3. To define features of congenital hypothyroidism and adreno-genital syndrome at newborns and to make the preliminary clinical diagnosis. 4. To make the plan of investigation and to analyze the data of laboratory and instrument investigations at the typical course of diabetes, at the typical course of diffuse toxic goiter, hypothyroidism, autoimmune thyreoiditis, endemic goiter at children; various clinical forms of growth disturbances, obesity, pubertal dyspituitarism, various forms of genital glands disturbances. 5. To show the possession of principles of treatment, rehabilitation and prophylaxis of diabetes mellitus, diffuse toxic goiter, hypothyroidism, autoimmune thyreoiditis, endemic goiter at children; various clinical forms of growth disturbances, obesity, pubertal dyspituitarism, various forms of genital glands disturbances. 6. To make the diagnosis and to give the urgent help at hyperglycemic and hypoglycemic comas, at thyreotoxic crisis at children. 7. To carry out differential diagnostics of diabetes mellitus at children, various kinds of comas; diffuse toxic goiter, hypothyroidism, autoimmune thyreoiditis, endemic goiter at children; various clinical forms of growth disturbances, obesity, pubertal dyspituitarism, various forms of genital glands disturbances and to make the preliminary diagnosis. 8. To carry out the life forecast at diabetes mellitus at children, various kinds of comas; diffuse toxic goiter, hypothyroidism, autoimmune thyreoiditis, endemic goiter at children; various clinical forms of growth disturbances, obesity, pubertal dyspituitarism, various forms of genital glands disturbances. 9. To show the possession of etiko-deontological principles of the medical expert and principles of a professional subordination in pediatrics. 8 Theme 11. Diabetes mellitus at children. Aetiology. Pathogenesis. Classification. Clinical manifestations. Diagnostics. Differential diagnostics. Treatment. Preventive measures. Prognosis of diabetes mellitus at children. Insulinotherapy. Hyperglycemic and hypoglycemic comas: an aetiology, pathogenesis, classification, clinical manifestations, diagnostics, differential diagnostics, granting of the urgent help and prophylaxis. Prognosis. Theme 12. Thyroid disorders at children. Classification of thyroid diseases at children. Aetiology, pathogenesis, classification, clinical manifestations, diagnostics, differential diagnostics, treatment, preventive measures of diffuse toxic goiter, hypothyroidism, autoimmune thyreoiditis, endemic goiter at children. Degrees of the goiter. The urgent help at thyreotoxic crisis at children. Prognosis. Theme 13. Hypothalamic-pituitary and genital glands disorders. Aetiology, pathogenesis, classification, clinical manifestations, diagnostics, differential diagnostics, treatment, preventive measures of different clinical forms of growth disturbances (exogenic-constitutional, pituitary, somatogenic); obesity (exogenic-constitutional, hypothalamic), pubertal dyspituitarism at children, different forms of the pathology of sexual glands at children (congenital disorders of sexual differentiation, disturbances of sexual development in boys and girls). Prognosis. THE THEMATIC PLAN OF THE PRACTICAL lessons, lecture(s), studies. DISCIPLINE "PEDIATRICS" THE MODULE 2. NEONATOLOGY, BLOOD AND ENDOCRINE DISEASES AT CHILDREN LESSON № 1. 6 hours, 11 points 1) Asphyxia of the newborn. 2) Birth trauma. Aetiology. Pathogenesis. Classification. Clinical manifestations. Diagnostics. LESSON № 2. 6 hours, 10 points 1)Birth trauma. Differential diagnostics. Treatment. Prophylaxis. Prognosis. 2) Haemolytic and hemorrhagic disease of the newborn. LESSON № 3. 6 hours, 11 points 1)Features of adaptation of newborns. The nursing and feeding organization of newborns. 2) Respiratory diseases at newborns. Syndrome of respiratory disorders of newborns. LESSON № 4. 6 hours, 10 points 1) Bacterial infections at newborns. 2) Respiratory diseases at newborns. Pneumonia in the neonate. LESSON № 5. 6 hours, 11 points 1) Childhood deficiency anemias. 2) Hemoblastoses at children. Leukaemias. LESSON № 6. 6 hours, 10 points 1) Hemoblastoses at children. Hodgkin`s disease. 2) Hemorrhagic disorders at children. 9 LESSON № 7. 6 hours, 11 points 1) Diabetes mellitus at children. 2) Hypothalamic-pituitary and genital glands disorders. Obesity, pubertal dyspituitarism, disorders of sexual development. LESSON № 8. 6 hours, 10 points 1) Thyroid disorders at children. 2) Hypothalamic-pituitary and genital glands disorders. Growth disturbances. LESSON № 9. 6 hours 1) Congenital infections (TORCH – infections) - 4 hours, 7 points 2) Total modular control: - control of practical skills - 2 hours, 30 points LESSON № 10. 6 hours, 50 points (30+20) 1) Total modular control: - The test control - Interview by program questions. TECHNIQUE OF ESTIMATION OF STUDENTS’ KNOWLEDGE For mastering of the themes a student gets points according to the traditional system. Lesson 1-8: «5» - 10-11 points «4» - 8 points «3» - 6 points «2» - 0. points Lesson 9: «5» - 7 points «4» - 6 points «3» - 4 points «2» - 0 points Fo the case history «5» - 29 points «4» - 23 points «3» - 18 points «2» - 0 points Maximum quantity of points for current educational activity of the student – 120. The students are allowed to the total modular control under condition of performance of requirements of the curriculum and in case if they got not less than 70 points for the current educational activity: not less than 52 points during a practical training and 18 points for a case history. 10 THE CONCLUDING MODULAR CONTROL The concluding modular control consists of 3 parts: The estimation of mastering of practical skills The test control Interview on thematic questions During the interview a student get points according to the traditional system. -The estimation of mastering of practical skills «5» - 30 points «4» - 26 points «3» - 19 points «2» -0 points - The test control «5» - 30 points «4» - 26 points «3» - 19 points «2» - 0 points. - Interview on thematic questions «5» -20 points «4» - 18 points «3» - 12 points «2» - 0 points The concluding modular control is enlisted to the student if he gets not less than 50 of 80 points. THE GENERAL ESTIMATION FOR THE MODULE (CURRENT EDUCATIONAL ACTIVITY + CONCLUDING MODULAR CONTROL ): 200 - 180 POINTS - «5» 179 - 160 POINTS - «4» 159 - 120 POINTS - «3» <120 POINTS - «2» THE LIST OF THE CONTROL METHODS І. THE CURRENT CONTROL On practical classes the following factors are estimated: a) Theoretical and practical preparation, i.e. independent out-of-class preparation of the student b) All kinds of educational activity of the student during practical classes Control methods: a) Individual oral interrogation b) Written theoretical work c) The solution of typical or situational problems d) The solution of test tasks e) Estimation of quality of performance of practical skills f) Performance of individual tasks 11 The gain score of the student is integrated (all kinds of works before the classes and during them) Repeating an examination The Student has the right to repeat only a mark „2” The Student is obliged to repeat „2” if the score of current progress does not reach minimum for the admission to the final modular control. The Quantity of a repeating an examination current mark „2” is not limited. The Student has the right to repeat current mark „2” throughout all period of studying of discipline, but not later than during the additional term regulated by educational department DSMA. Throughout one consultation the student can repeat only one current mark „2” ІІ. THE FINAL MODULAR CONTROL It is carried out at the last lesson of the test module Control methods: A) Estimation of quality of performance of practical skills B) The solution of test tasks C) Individual oral interrogation on the theoretical questions provided by the program The score for the final modular control – the sum of points for all kinds of the control (A,B,C,) The possible reasons to fail the final modular control: - The student has not got a minimum quantity of points for current educational activity and is not admitted to the concluding modular control - The student has passed the concluding modular control, but has got on it less than 50 points. - The student has unfinished admissions of classes and (or) lectures - The student was not on the concluding modular control Repeating an examination 1. The repeating an examination of the final modular control is held no more than 2 times 2. The first repeating an examination of the final modular control is held according to the department schedule on Saturday in the presence of the modular group in the period not more than three weeks after the primary attempt according to the plan, but not later than the last day of semestre. The repeating an examination is carried out exclusively under the dean's office sheet. 3. The repeated (second) repeating an examination of the final modular control (or controls if there are some of them) is carried out by commissions after discipline end under the dean's office sheet in additional term. A repeating an examination is held in the presence of modular group in the day defined by the schedule of educational department DSMA. Maximum quantity of points which is given to students at mastering of each module - 200. Converting to a traditional mark: ‘’5’’: 200" - 181 points ‘’4’’: 180" - 141 points ‘’3’’: 140" - 121 points „2”: less than 121 points PRACTICAL SKILLS WHICH ARE CHECKED 12 DURING THE FINAL MODULAR CONTROL ON THE MODULE 2. Neonatology 1. To be able to carry out objective investigation of the healthy neonate. 2. To be able to define gestational age of the preterm infant using Dubovich`s and Balard`s scales. 3. To be able to perform an umbilical cord debridement and to look after umbilical rest, skin and umbilical wound of the newborn. 4. To be able to organize adequate feeding of preterm and full-term with severe diseases. 5. To be proficient in nursing procedure and technique of preterm and injured children in incubators. 5. To be able to estimate asphyxia severity using Apgar scale. 6. To be able to perform primary immobilisation at clavicular, humeral and femoral bones fractures. 7. To be able to determine indications and to perform exchange transfusion. 8. To be able to evaluate degree of respiratory failure at the newborn and to order oxygen therapy depending upon the severity level. 9. To be able to evaluate the data of laboratory and instrumental investigations at different diseases of the newborn. 10. To be able to perform and evaluate the Apt test. 11. To be able to give the urgent help at following states: - asphyxia of the newborn - hemolytic disease of the newborn - syndrome of respiratory disorders. Blood and endocrine diseases at children 1. To be able to carry out clinical investigation (anamnesis, inspection, palpation, percussion, auscultation) of children having blood and endocrine diseases, evaluating physical and sexual development of the child, definition of increase in body weight, a syndrome of growth delay and growth acceleration using sygmal deviations. 2. To be able to evaluate the blood count at children of different age in normal state and in pathological conditions, indicators of nonhemoglobin iron in normal state and in pathological conditions, coagulogram, bone marrow aspirates, the data of investigation of hemostatical system, to evaluate bone age of the child, express diagnostics of diabetes mellitus at children. 3. To be able to investigate vascular resistance, to palpate a thyroid gland, to estimate its function. 4. To be able to calculate total quantity of alimentary iron on treatment course, an insulin dosage according to the state of the patient, to master the technique of its administration. 5. To be able to give the urgent help at following conditions: - hemorrhage at the hemophilia - hemorrhagic shock - syndromes of сдавления - ketoasidotic coma - hypoglycemic coma - thyrotoxic crisis THE LIST OF QUESTIONS TO THE FINAL MODULAR CONTROL OF THE MODULE 2. Neonatology 13 1. Definition of the term “prematurity”. Classification of preterm infants by parameters”weight of a body at a birth” and correlation of physical development and gestational age. 2. The reasons of fetal intrauterine growth delay. Features of adaptation of children with intrauterine growth delay and nursing principles. 3. Evaluation of a morphological and neurofunctional maturity of preterm (using Balard`s scale). 4. Features of thermoregulation of preterm infants, methods of prophylaxis of hypothermia. 5. Prophylaxis and treatment of hypoglycemia in the preterm infant. 6. Mechanisms of the development of hyperbilirubinemia in the preterm infant, possible consequences. Management tactics. 7. The urgent help at apnoe in the preterm infant. The indication to the application of mechanical ventilation. Complications of prolong mechanical ventilation: bronchopulmonary dysplasia, retinopathy of preterm infants. 8. Nursing stages of preterm infants. Transportation principles. Criteria of the hospital discharge. 9. Features of dispensary supervision for preterm infants in polyclinic. Anaemia prophylaxis, lactase insufficiency, a dysbacteriosis, rickets. 10. Feeding principles of preterm infants. A choice of a way of feeding depending on gestational age and a condition of the child. The recommended volumes of enteral feeding. 11. Etiological, clinical and laboratory criteria of the diagnosis „ asphyxia of the newborn”. 12. Contemporary conceptions about asphyxia pathogenesis. Compensatory mechanisms of the fetus to hypoxia. 13. Criteria of asphyxia severity depending on the evaluation of Apgar scale, indicators РН and signs of body system dysfunction. 14. Algorithm of rendering of the urgent help to the child having asphyxia at a birth depending on the presence or absence of signs of meconial aspiration. 15. Definition of the term „birth trauma” and the courses of its development. 16. Birth traumas of soft tissues. Adiponecrosis. Injury of sterno-cleido-mastoideus muscle. The differential diagnosis of birth tumour and cephalogematoma. 17. Birth trauma of the spinal cord and brachial plexus injuries. Erb and Klumpke palsies. 18. Differential diagnostics of intracranial hemorrhages of hypoxic and traumatic origin at newborns. 19. Definition of the surfactant system of lungs. Factors of the development of the syndrome of respiratory disorders in the neonate. Mechanism of the development of the disease of hyoline membranes. Methods of antenatal prophylaxis. 20. Evaluation of the severity of respiratory failure at the syndrome of respiratory disorders (SRD) using Silverman`s and Downes` scales. 21. Methods of antenatal prediction and postnatal diagnostics of SRD. Radiological signs of SRD. 22. Principles of SRD treatment at newborns. Respiratory support. Surfactant therapy. 23. Classification of the pneumonia in the neonate depending on the way and term of infection. An aetiology. 24. Risk factors of the development of the pneumonia in the neonate. Pathogenesis. 25. Features of the course of pneumonia at newborns depending on the sources of infection and aetiology. 25. Principles of diagnostics and treatment of the pneumonia in the neonate. Features of aethiological therapy. 27. Erythrocyte blood antigene systems of the person. Aetiology, pathogenesis of haemolytic disease of the newborn (HDN). 28. Classification of HDN. Clinical and laboratory criteria of anemic, icteric and adematous forms of HDN. 29. Criteria of the severity of HDN. Stages of bilirubin encephalopathy. 30 Methods of antenatal diagnostics and prophylaxis of haemolytic disease of the fetus. 31 Indications to the exchange transfusion. Technics of the operation and its possible complications. 32 Methods of conservative therapy of HDN. The mechanism of action of phototherapy. 14 33 Features of the system of hemostasis in the neonate. Development factors of hemorrhagic disease. Clinical features of early, classical and late forms of hemorrhagic disease. 34. Differential diagnostics of the hemorrhagic disease and the syndrome „swallowed blood”. The urgent help at the gastroenteric bleeding. Treatment and prophylaxis of hemorrhagic disease. 35. Definition of the term „ТОRСН-infections”. Risk factors of intrauterine infection (congenital infections - CI). 36. Character of damage at congenital infections depending upon the term and the way of fetus infection. 37. Methods of early diagnostics and prophylaxis of CI. 38. Clinical manifestations of CI depending upon the aetiology (congenital toxoplasmosis, rubella, neonatal herpetic and cypomegalovirus infection). 39. Principles of treatment of CI. Aetiotropic and immunotherapy. 40. Omphalitis. Aetiology. Pathogenesis. Classification. Diagnostics. Prophylaxis and treatment. 41. Vesiculopustulosis, neonatal pemphigus, Ritter`s exfoliative dermatitis. Aetiology, clinical presentations, treatment. Prophylaxis. 42. Definition of the term „neonatal sepsis”. Developmental factors. 43. Classification and an aetiology of neonatal sepsis. 44. Clinical and laboratory criteria of neonatal sepsis. 45. Treatment and prophylaxis principles of neonatal sepsis. Blood and endocrine diseases at children 1. Definition of the term «anaemia» Classification of childhood anemias. 2. Irondeficiency anaemia at children. The causes, clinical manifestations, diagnostics, differential diagnostics. 3. Treatment and prophylaxis of irondeficiency anaemia at children. 4. Chronic posthemorrhagic anaemia at children. Aetiology, pathogenesis, diagnostics. The urgent help at bleedings. 5. Leukaemias at children. The causes. Classification of leukaemias. Its association with the scheme of blood production. 6. Clinical variants of the course, diagnostics and differential diagnostics of acute lymphoblastic leukemia at children. 7. Programs of treatment of leukaemias at children (acute lymphoblastic leukemia, acute mieloblastic leukemia, chronic myeloid leukaemias). Cytostatics. Indications to their application. Complications of cytostatic therapy (immediate, delayed). 8. Classification of hemoblastoses. Hodgkin`s disease at children. Aetiology, pathogenesis, disease stages (by Ann Arbor). 9. Diagnostics, differential diagnostics of Hodgkin`s disease at children having other lymphadenopathy, lymphadenitis; hemoblastoses. 10. Clinical manifestations, treatment, prognosis of Hodgkin`s disease at children. The urgent help at a syndrome of squazing the superior vein cava. 11. Definition of the term hemorrhagic diatheses. Classification. 12. Hemophilia A and and B. Aetiology, pathogenesis, clinical manifestations, diagnostics. Prognosis at children. 13. Substitutional therapy at rendering of the urgent help by the patient having hemophilia. Antihemophilic medications (concentrates of clotting factors, fresh frozen plasma) and their application. 14. Hemorrhagic vasculitis at children. Aetiology, pathogenesis, clinical forms, diagnostics and differential diagnostics, treatment, prognosis. 15. Thrombocytopenic purpura at children. Aetiology, pathogenesis, clinical manifestations, diagnostics, differential diagnostics, treatment, prognosis. The urgent help at bleedings. 16. Diabetes mellitus at children. Aetiology, pathogenesis, clinical manifestations, diagnostics, treatment principles, criteria of diabetes compensation at children. 17. Features of the diabetes course at preschool children and at teenagers. 15 18. Regimens of insulinotherapy at children. Insulin preparations. 19. Features of the diet at the compensated and not compensated diabetes at children. 20. Hyperglycemic ketoacidotic coma at children. The causes, clinical manifestations, diagnostics, the urgent help. 21. The hypoglycemic coma at children. The causes, clinical manifestations, diagnostics, the urgent help. 23. Differential diagnostics of hyperglycemic and hypoglycemic comas at children. 24. Growth disturbances at children. Pituitary nanism. The causes, clinical manifestations, the differential diagnosis. Treatment and prognosis. 25. Obesity at children. The causes, clinical forms. 26. Principles of complex treatment of various clinical forms of obesity at children. Prophylaxis 27. Autoimmune thyroiditis at children. Aetiology. Pathogenesis. Clinical manifestations. Differential diagnostics. Treatment. Prognosis. 28. Diffuse toxic goiter at children. Aetiology. Pathogenesis. Clinical manifestations. Differential diagnostics. Treatment. Prognosis. 29. Endemic goiter at children. Causes, clinical manifestations, diagnostics, treatment, prophylaxis. 30. Hypothyroidism at children. Aetiology, pathogenesis, clinical manifestations, early diagnostics. Treatment, prognosis. 31. Clinical manifestations and diagnostics of congenital hypothyroidism at children. Treatment. Prognosis. 31. Disorders of sexual development in boys and girls. Aetiology, pathogenesis, clinical manifestations, diagnostics, differential diagnostics, treatment. 32. Differential diagnostics of variants of intersexualism. Methods of investigation. Treatment principles. Practical works (task) which are carried out at the lesson: 1. To collect complaints, the life and disease anamnesis. 2. Consistently to inspect the child. 3. To reveal early signs of disease. 4. To reveal signs of complications of the basic disease. 5. To evaluate the condition of the child to available clinical symptoms. 6. To evaluate additional methods of investigation and to make correction of inspection of the child. 7. To make the clinical diagnosis behind classification. 8. To make the plan of contemporary treatment using protocoks. 9. To make recommendations towards dispensary supervision. Asphyxia of new-born 1. Actuality of the topic: Intrahospital hypoxia – polyetiologic phenomenon which occurs quite often nowadays. It is hard to find a pregnancy which would pass without any complications (mother’s illness, toxicosis, external influence on fetus and so on). Most often chronic hypoxia is the affection factor of internal organs and systems, first of all – nervous system, therefore the knowledge of asphyxia causes, ability to render urgent medical help to a new-born baby, ability to diagnose abnormality in child’s health and carry our correcting procedures are necessary skills for each doctor. 2. Certain purposes: 1. 2. 3. 4. А. A student should know: Basic causes which lead to oxygen hunger in intranatal period Definition of term “asphyxia of a new-born baby” Methodology of estimation of new born baby’s condition according to Apgar Algorithm of rendering urgent help to a child born in asphyxia 16 5. Principles of intensive therapy and observation at early post-asphyxia period. 6. Consequences of new born baby’s asphyxia - in nervous system - in cardio-vascular system - in respiratory system - in kidneys - in adrenal glands - in gut - in immune system - in metabolism 7. Notion of hypoxic-ischemic encephalopathy 8. Mechanical formations of HIE 9. Clinical manifestations of HIE 10. Principles of treatment and rehabilitation of children with HIE 11. HIE outcomes 1. 2. 3. 4. 5. 6. 7. 8. B. A student should be able: To determine signs of asphyxia in new-born babies To estimate condition of a new-born baby according to Apgar scale To determine the degree of AN To draw up a plan of rendering urgent aid to a certain child To draw up a plan of further child’s treatment with AN To reveal signs of HIE in a new-born baby To reveal signs of post-hypoxic abnormalities in other systems and organs To draw up a plan of in-patient observation over children who suffered new-born asphyxia (AN) 3. Tasks for self-study work whilke preparing for the lesson 3.1. A list of basic terms, parameters, characteristics a student should master while preparing for the lesson: Term Definition 1. Asphyxia of a new-born baby Pathological condition caused by gas disorders in the need of 02 necessity, superficiality of С02 which takes place along with metabolic acidosis Brain damage caused by perinatal hypoxia which is manifested by morphological-functional disorders and signs of cerebral insufficiency First revealed before birth First revealed during the delivery Mild asphyxia which develops due to depression of respiratory center which most often occurs while using sedative, pain-killers, in narcosis without acidosis development It is manifested by worry, sleep disorders, regurgitation, painful cry, increase of muscular tone, tremor of extremities and chin, hyperreflexia Most often it occurs in pre-term babies due to immaturity of CNS, which is a generalized slow-down, languor, adynamy, hyporeflexia, muscular hypotonia It is manifested by the presence of a necessary condition – head is thrown back, extremities are bent, fists are squeezed (a “boxer” pose), presence of “cerebral” cry, regurgitation and vomiting, hyper and tremor of extremities, vertical and rotator nystagmus, Grefe symptom 17 2. Hipoxic-ischemic encephalopathy 3. Antenatal hypoxia 4. Intranatal hypoxia 5. Cardiac-respiratory syndrome 6. Syndrome of increased nervous anxiety 7. Syndrome of general depression 8. Hypertension syndrome 9. Hydrocephalic syndrome 10. Cramp syndrome 11. Comatose condition 12. Neurosonography It develops closer to the end of acute period and it is manifested by increase of head in volume, domination of cerebral cranium over facial, bridge changes with hanging of forehead part, increase of venous picture on the head, widening of liquor system and increase of ventricular index according to data of brain ultrasound It is most often manifested by generalized clonic-tonic cramps. More seldom focal and multifocal, mioclonic cramps take place. It develops in case of brain edema and it is characterized by unconsciousness, absence of motor activity, cry, emotions and reaction to pain Ultrasound of brain structures with sensor in big fontanel Infant’s birth trauma 1. Actuality of the topic: Injuries of organs and tissues which occur during the birth can cause further function disorders of corresponding organs and systems. The most essential is the injury of Central Nervous System. Early diagnostic and treatment as well as adequate rehabilitation considerably enhance the prognosis. 2. Specific aims: А. A student should know: 1. Definition of term “birth injury.” 2. Causes of birth traumas. 3. Classification of birth injuries. 4. Clinical signs of birth injuries of different localization: А. Fracture of clavicle. B. Trauma of muscle sternocleidomastoideus. C. Cephalohematoma. D. Intracranial birth injury. E. Trauma of spine. 5. Additional diagnosing methods in patients with birth traumas. 6. Main complications which occur during birth traumas. 7. Phases of course in patients with birth CNS injury. 8. Principles of treatment of new-born after birth trauma depending on location. 9. Principles of rehabilitation after birth injuries. В. A student should be able: 1. To determine clinical signs of birth injury. 2. To detect and analyze anamnesis factors which could have promoted birth injury during the birth. 3. To carry out differential diagnosing between traumatic and other injuries of organs and systems. 4. To formulate diagnosis of birth trauma. 6. To draw up a plan of the new-born baby with birth trauma. 7. To draw up a plan of treatment for infants with birth injury: А. Fracture of clavicle. Б. Injury of muscle sternocleidomastoideus. 18 C. Cerebral hemorrhage. D. Spine injury. 8. To determine signs of complications for the child with birth trauma. 9. To draw up a plan of rehabilitation for children with birth injury. 3. Tasks for self work while preparing for the lesson. 3.1. List of main terms, parameters, characteristics a student has to master while preparing for the lesson: Term Birth trauma of infants Birth tumor Cephalohematoma Interbrain traumatic hematoma Hemorrhage Paralysis of diaphragm nerve (СЗ, 4 or 5) Fracture of clavicle Paralysis of Erb Intraventricular hemorrhage Subdural hemorrhage Subarachnoid hemorrhage Definition Injury of organs and tissues of a fetus which happens during the birth. The most severe injuries are those with cerebral hemorrhage and they require special treatment Gathering of serous-blood fluid subcutaneously, outside periosteum, with badly delineated edges; it can spread through linea media and through stitch lines and is usually related to compression of fetus head during the birth Periosteum hemorrhage in infant’s skull area Gathering of blood in brain matter which appears due to traumatic hemorrhage and can cause brain compression. Being in the white matter of brain it can create a cavity Gathering of blood in tissues or body cavities due to increase of penetrability or disorders in blood vessel integrity It is a result of overstraining of lateral cervical muscles. It is practically always one-sided and it is often connected with injuries of plexus brachialis Most often it is neonatal orthopedic injury. An infant has pseudoparalysis on the injured side, crepitation, bone displacement, spasm of muscle sternocleidomastoideus. Bone breaks (not complete) can be without signs Injury of the fifth and sixth cervical spinal nerves. The injured arm is brought into motion and makes a rotation with straightened elbow, forearm remains in prone position, wrist is arcuated. Morpho, biceps, radiocarpal reflexes on the injured side are absent. Grasp reflex is normal It happens more often with pre-term children as a result of hypoxic influences and small gestation age. Acute adynamy, tonic cramps are typical, tremor of high magnitude, hypertension syndrome, strabismus, vertical nystagmus, thermoregulation disorders, abnormal breath rhythm and cardiac activity are present, congenital and tendinous reflexes, sucking, swallowing are suppressed Birth injury which happens most often during prolonged or fast birth and causes displacement of brain ventriclesи, liquor ways, increase of intracranial pressure. One of main death causes of infants is compression of vital centers in medulla Birth injury which occurs in children during prolonged birth, especially in case of obstetrician interventions; most often in preterm babies and it is accompanied by anxiety, clonic-tonic cramps, manifested vegetative-visceraldisorders, increase of muscular tone 19 Adiponecrosis Neurosonography Computer tomography Magnetic-resonant tomography. and tendious reflexes, bulging of fontanel, Gref-s symptome, strabismus, horizontal nystagmus; typical changes in spinal liquid: xanthochromia, blood presence, cytosis up to 1,000 and more, lymphoid cells, strongly positive Pandy’s reaction, general protein 0.3 – 1.3 g/l Focal necrosis of subcutaneous fat, well-defined solid nodes 1-5 cm in diameter in subcutaneous layer of buttocks, back, shoulders, extremities. It develops at the age of 1-2 weeks old Ultrasound brain study of an infant with a sensor in fontanel major An X-ray method (unlike plain X-ray), which provides us with the opportunity to get the screen of a specific cross-section of a human body. The body can be studied by layers with the step of 1 mm This method with the use of electric-magnetic waves gives us a chance to visualize brain, spinal cord and other internal organs with high quality 3.2. Theoretical topics for the lesson: Definition of term ”birth injury " (BI). Frequency of BI among other infant’s diseases. Causes of BI development. Conditions impacting BI appearance. Localization of BI. Pathogenesis of different BI forms. Clinical symptoms typical for BI of different location: muscle BI, bone BI, brain BI, spine BI , BI of peripheral nervous system. 8. Value of additional methods while diagnosing BI. 9. Classification of birth injuries in nervous system. 10. Complications of BI . 11. Principles of therapy and rehabilitation of children with BI. 12. Prophylaxis of BI and their complications. 13. Outcomes of BI. 1. 2. 3. 4. 5. 6. 7. 3.2. Theoretical questions to the lesson: 1. Definition of term “asphyxia of a new-born baby” 2. Reasons of new-born asphyxia 3. Reasons of chronic and acute intranatal fetus hypoxia 4. Pathogenesis of changes in case of fetus hypoxia 5. Use of contemporary diagnosing methods for fetus estimation (CT, ECG, US and so on) 6. Clinical signs of asphyxia in new-born babies 7. Methodology of estimation of new born baby’s condition according to Apgar 8. Determination of asphyxia degree 9. Urgent help to a new-born child in asphyxia 10. Contemporary equipment used for reanimation and intensive care. Methods of ALV 11. Correction of metabolism disorders 12. Complications of asphyxia in new born children - in nervous system - in cardio-vascular system - in respiratory system - in kidneys - in adrenal glands - in gut - in immune system 20 - in metabolism 13. Complications of reanimation and intensive care 14. Notion of hypoxic-ischemic encephalopathy 15. Pathogenesis in development of hypoxic-ischemic encephalopathy 16. Clinical signs of hypoxic-ischemic encephalopathy. Neurological, somatic and metabolism disorders 17. Contemporary methods of diagnosing CNS disorders (neurosonography, CT, NMR, etc.) 18. Classification of hypoxic-ischemic encephalopathy 19. Treatment and rehabilitation of children with hypoxic-ischemic encephalopathy 20. Principles of treatment and control on pediatrics regions and its effectiveness 21. Outcomes of hypoxic-ischemic encephalopathy H(A)EMOLYTIC DISEASE OF THE NEWBORN HEMORRAGIC DISEASE OF THE NEWBORN 1. Theme urgency: Coagulopathy takes first place among hemostatic disorders of the newborn. Hemorragic disease of the newborn (HrDN) is caused by severe depression of vitamin-K-dependent cofactors (ІІ,VІІ,X,ІХ). So newborns become at risk for developing severe life-threatening hemorrhages. Hemolytic disease of the newborn (HDN) often has severe course and in some cases unfavorable prognosis (through the complications). Therefore prophylaxis, timely diagnostics and appropriate treatment of HDN has importance in neonatology and pediatrics in the whole. 2. Specific purposes А. Student has to know: 1. Features of hemostasis at term and preterm infants. 2. Etiology of HrDN. 3. Clinical findings consistent with HrDN. 4. Auxiliary diagnostic criteria of HrDN. 5. Complications of HrDN. 6. Principles of rendering treatment at urgent states at umbilical bleeding, gastrointestinal haemorrhages. 7. Form plan of treatment of HrDN. 8. Carry out prophylaxis of HrDN.. 9. Definition of term «hemolytic disease of the newborn». 10. Settings, in which HDN most likely to occur. 11. Essential pathogenetic mechanisms of developing various variants of HDN. 12. Clinical findings consistent with various variants of HDN. 13 Additional methods of examination for confirmation the diagnosis of HDN. 14. Basic complications of HDN 15. Causes and developmental phases of bilirubin encephalopathy. 16. Principles of treatment of HDN depending upon clinical form. 17. Indications and technique of exchange transfusions. 18. Principles of prophylaxis of HDN. B. Student has to be able to: 1. Determine clinical symptoms of HrDN. 21 2. Carry out auxiliary investigations and evaluate its results. 3. Carry out differential diagnosis among other hemorrhagic disorders of infants. 4. Make the diagnosis of HrDN. 5. Form plan of treatment of chidren having HrDN. 6. Give emergency medical care to newborns having haemorrhage. 7. Determine clinical symptoms of HDN. 8. Reveal and и analyse anamnestic factors, which could contribute to the development of HDN. 9. Carry out differential diagnosis among HDN and other diseases, which is accompanied by jaundice. 10. Carry out differential diagnosis among various forms of HDN. 11. Make the diagnosis of HDN. 12. Make plan of investigation of chidren having HDN. 13. Make plan of treatment of chidren having HDN 14. Reveal signs of complications of chidren having HDN. 15. Determine indications and make the plan of performing exchange transfusions. 3.Tasks for students` self-dependent work during preparation for the classes. 3.1 List of main terms, parameters, characteristics, which students has to master preparing for the classes. Term 1.Hemolytic disease of the newborn (HDN) 2.Icteric form of HDN 3.Anemic form of HDN 4.Edematous form of HDN 5. Bilirubin encephalopathy 6. Syndrome of bile clotting 7. Coombs` test 8. Phototherapy 9. Hemorragic disease of the newborn (HrDN). definition Disease, which is caused by Rh D alloimmunisation or by maternal and fetus ABO incompatibility, or by other erythrocyte antigens. Accompanied by significant increase of indirect bilirubin and first of all manifested by yellowish colouring of skin and mucous membranes. Manifested predominantly by low hemoglobin (<120 g/l) and hematocrit (< 40%) level since birth. Characterized by signs of anemic syndrome. Almost always caused by \ maternal and infant Rh-incompatibility. Manifested in generalized edema and anemia since birth. Has high percentage of lethality. Complication of HDN HDN related to toxic effect of bilirubin to nerve cells. Complication of HDN related to intense production of direct bilirubin and change of bile biophysical features. Serologic method for revealing antibodies. Indirect hyperbilirubinemia`s method of treatment with usage of light energy with wavelength according to spectrum of visible light. Primary hemorrhagic syndrome, caused by deficiency of plasmatic clotting factors in the 22 10. Vitamin-K-dependent cofactors 11. Melena 12. Hematemesis 13. The Apt test neonate, predominantly vitamin-K-dependent. Plasmatic clotting factors, synthesis of which in liver requires the presense of vitamin K (ІІ, VІІ, ІХ, Х). Presense of blood in stool. Presense of blood in vomiting Can determine if it is swallowed maternal blood or fetal hemorrhage. This test relies on the increased sensitivity of adult hemoglobin to alkali (NaOH) compared with fetal hemoglobin. 3.2. Theoretical questions for classes: 1. Kinds of hemorrhagic disorders at children. 2. Hemostasis features at infants. 3. Causes of hemorrhagic disorders of the newborn. 4. Causes of HrDN development. 5. Clinical characteristics of HrDN. 6. Bleeding types among HrDN. 7. Principles of rendering treatment at urgent states at newborn hemorrhages. 8. Auxiliary diagnostic methods of HrDN. 9. Complications of HrDN. 10. Treatment of HrDN. 11.Nutrition of children having HrDN. 12. HrDN profilaxis. 13. Definition of term ” HDN ". 14. Freguency of HDN among other infant diseases. 15. Causes of HDN development. 16. Conditions causing HDN. 18. Features of developing various forms of HDN. 19. General clinical symptoms consistent with HDN . 20. Clinical characteristics of particular HDN forms. - edematous - icteric - anemic - mixed 21. Significance of auxiliary research procedures in HDN diagnostics. 22. Classification of HDN. 23. Complications of HDN. 24 Settings, in which bilirubin encephalopathy most likely to occur. 25. Bilirubin encephalopathy prophylaxis. 26. Syndrome of bile clotting 27. Principles of HDS treatment. 28. Prophylaxis of HDS and its complications. 23 Features of adaptation of newborns. The organization of newborn nursing. 1. A theme urgency: Prematurity is one of the major problems of public health services in the world. The statistics testifies to presence of high death rate among preterm children in perinatal period and about the big percentage among children, who have survived, physical, intellectual and emotional disability, the ethical problems connected with the price and efficiency of treatment of very low birth weight infants. 2. Specific goals: А. Student should know: 1. Definition of term “prematurity”. 2. Degrees of prematurity. 3. Causes of prematurity. 4. Influence of a course of premature labour of preterm infants. 5. Anatomo-physiological features of the central nervous system of preterm infants. 6. Anatomo-physiological features of cardiovascular system of preterm infants. 7. Anatomo-physiological features of respiratory system of preterm infants. 8. Anatomo-physiological features of endocrine system of preterm infants. 9. Anatomo-physiological features of skin, subcutaneous fat, osteomuscular and urinogenital systems, thermoregulation. 10. Definition of physical development of preterm infants. 11. Definition of functional maturity of premature infants. 12. Features of the course of the period of early neonatal adaptation at these children: - state of of haemodynamics, - degree of lungs maturity - features of metabolic adaptation. 13. Nursing principles of premature infants depending on degree of prematurity. 14. Use of incubator, beds with heating, hot-water bottles. 15. Temperature regimens of incubator depending on the degree of prematurity and child condition. 16. Humidity regimens of incubator depending on the degree of prematurity and child condition. 17. Feeding strategies for preterm infant. 18. Methods of calculation of daily volume of feeding. 19. Enteral feeding, indications, a carrying out technique. 20. Probe feeding, indications, a carrying out technique. 17. The technique of an establishment of tolerance to food. 21. Parenteral feeding, indications, a carrying out technique. 18. Transferring of preterm infants on ІІ a nursing stage. 22. Structure of perinatal morbidity and mortality among preterm infants. 23. Features of course of asphyxia, birth trauma and other diseases. 24. Features of neuropsychological development of preterm infants. 21. Indications to the discharge of the preterm infants, nursing organisation on pediatric sites. В. Student should be able: 1. To determine aetiological factors of prematurity. 2. To establish degree of prematurity. 3. To evaluate functional maturity of premature infant. 4. To determine features of adaptation of preterm infants and to diagnose disadaptational syndrome. 24 5. To classify and analyze a typical clinical picture of degrees of morphological and neurofunctional maturity of preterm infants. 3. To reveal presence of a disorder at the child. 4. To make the plan of investigation and to analyze the data of laboratory and instrumental investigations of preterm infants. 5. To diagnose and render the emergency help at the basic urgent conditions at preterm infants: respiratory insufficiency, intestinal paresis, hyperbilirubinaemia, hypoglycemia. 6. To appoint a nursing method of premature infant. 7. To appoint a kind of feeding of the child and to calculate daily volume of food. 7. To establish the indication for transferring of the child on ІІ a nursing stage. 8. To show proficiency in moral and deontologal principles of the medical expert and in principles of professional subordination in neonatology. 3. Tasks for students` self-dependent work during preparation for the classes. 3.1. List of main terms, parameters, characteristics, which students has to master preparing for the classes. The term Preterm infant The newborn child with a delay of prenatal development (small for gestational age) Preterm infant with a delay of prenatal development Low birth weight infants Very low birth weight infants Extreme low birth weight infants Apnea Heating chain «Skin to skin» contact Optimum body temperature Severe hypothermia Incubator "Mother-kangaroo" Open arterial canal (Botallo`s duct) Definition Infants born at 22-37 full weeks` gestation irrespective of body weight and growth at birth. Infants who were born at 37 full weeks` gestation and have indexes of physical development smaller than appropriate for gestational age (<10 percentile) Child who was born preterm and has indexes of physical development smaller than appropriate for gestational age (<10 percentile) < 2500 grammes < 1500 grammes < 1000 grammes The discontinuation of independent breathing with duration over 20 seconds. Set of organizational measures at the time of delivery and after child birth to prevent further heat losses at the newborn child. Is carried out by putting the child on the breast or abdomen of mother right after birth. Lasts not less than 2 hours in case of a stable clinical condition of the child. The body temperature 36,5-37,5ºС in the first days and 36,8-37,2ºС the next days. The body temperature 35,0ºС and lower The incubator for nursing of very low birth weight infants or sick newborns with possibility of regulation of temperature and humidity in the device. Nonconventional method of taking care after premature infants and/or low birth weight infants after stabilization of their condition, which provides direct corporal contact of mother and the child. Functioning of a channel, which connects an initial part of an arch of an aorta to a pulmonary artery in the area of it bifurcation. 25 Bollard`s scale The scale, according to which it is possible to define functional maturity of preterm infants. It is based on the registration of indicators of a neuromuscular and physical maturity for the establishment of gestational age of the child within 20-44 weeks` gestation/ Level of glucose below 2,2 mmol/l. Hypoglycemia 3.2. Theoretical questions for classes Definition of term “prematurity”. Causes of prematurity. Degrees of prematurity. Anatomo-physiological features of respiratory, cardiovascular, endocrine, immune, central nervous systems. 5. Anatomo-physiological features of skin, subcutaneous fat, urinogenital systems. 6. Features of the course of the period of early neonatal adaptation at these children: state of of haemodynamics, degree of lungs maturity features of metabolic adaptation. 7. Features of thermoregulation, water-electrolytic balance, metabolic processes 8. Nursing principles of preterm infant in maternity hospital on the І stage. 9. Feeding strategies for preterm infant in maternity hospital on the ІI stage. 10. Observational principles for preterm infants on a pediatric site. 1. 2. 3. 4. - Respiratory diseases in the neonate 1. Theme urgency: The syndrome of the respiratory disorders takes first place among the causes of the lethality of the preterm infants. This syndrome is caused by pneumopathies. This problem is extremely actual because of the severity of pneumopathies` course and disadvantageous prognosis in most cases. Problems of diagnostics and treatment of pneumonia at newborn children also should be taken into account. Even nowadays pneumonia can cause lethality among newborns and infants. Early revealing and timely liquidation of inflammatory pulmonary process in the neonate provides favorable outcome and more proper development of the child in the future. 2. Specific goals: А. Student should know: 1. Definition of term “the syndrome of respiratory disorders” (SRD). 2. Principal causes of SRD development. 3. Pathogenesis of pneumopathies. 4. Structure and functions of surfactant. 5. Principles of estimation of SRD severity at newborns. 6. Clinical manifestations of pneumopathies: - disease of gialine membranes - atelectasis of the lungs -edematous-hemorrhagic syndrome 7. Laboratory and instrumental diagnostics of pneumopathies. 8. Principles of the urgent help to children having SRD. 9. Principles of treatment of children having pneumopathies. 26 10. Complications and the prognosis of pneumopathies. 11. Outcomes of SRD. 12. Etiologial structure of pneumonia of newborns (PN). 13. The reasons of susceptibility of the fetus and the newborn to infectious agents - factors of pneumonia. 14. Factors which assist development of PN. 15. Pathogenesis of disorders which occur in the organism of the child at PN. 16. Features of the clinical picture at PN. 17. Features of the pneumonia depending upon the etiological factor. 18. Differences between congenital and postnatal PN. 19. Early signs of PN. 20. Classification of PN. 21. Principles of treatment of children with PN. 22. Principles of dispensary supervision over reconvalescents of PN. В. Student should be able:: 1. To reveal clinical signs of «the syndrome of respiratory disorders” (SRD) at the newborn. 2. To define the SRD severity. 3. To appoint investigation for the specification of the SRD origin. 4. To estimate the obtained data. 5. To make a plan of treatment of the child having SRD. 6. To define complications of SRD. 7. To carry out prophylaxis of pulmonary infectious and non infectious diseases at newborns. 8. To define the severity of respiratory disorders at PN. 9. To reveal clinical signs of PN. 10. To appoint investigation to the child for the confirmation of diagnosis of PN. 11. To carry out differential diagnostics of antenatal and postnatal PN. 12. To formulate the pneumonia diagnosis according to classification. 13. To make the plan of treatment of the child with PN. 14. To appoint etiotropic therapy to the child with PN. 3. Tasks for students` self-dependent work during preparation for the classes. 3.1. List of main terms, parameters, characteristics, which students has to master preparing for the classes. The term Definition 27 1. The syndrome of respiratory disorders 2. Pneumopathies 3. Gialine membranes. 4.Surfactant 5. Pneumonia of newborns 6. Sylverman-Andersen and Dawns` scales Acute respiratory insufficiency with expressed arterial hypoxia, which arises during the first hours and days of the newborn life. Alterations in lungs which causes asphyxia of newborns. Pneumopathies: disease of gialine membranes, edematous-hemorrhagic syndrome, disseminated pulmonary atelectases and edematous syndrome. The most severe form of pneumopathies. High-molecular lipoproteid which provides antiatelectatic function. Deficiency of which causes diosorders of ventilatory-perfusional relation in lungs with the development of hypoxia, hypercapnia, metabolic-respiratory acidosis. Infectious disease with localisation of inflammatory process in pulmonary parenhima and disorders of functions of other systems of an organism Scales for the estimation of the severity of the syndrome of respiratory disorders at newborns. 3.2. Theoretical questions for classes: 1. Definition of the term “the syndrome of respiratory disorders” (SRD). 2. Causes of SRD. 3. Pneumopathies, as the most frequent cause of SRD at premature infants. 4. Causes of pneumopathies . 5. Estimation of SDR severity. 6. Surfaktant, its structure and functions. 7. Clinical manifestations of pneumopathies . 8. Additional methods of pneumopathies` diagnostics. 9. Complications of pneumopathies. 10. Main principles of treatment of pneumopathies. Pathogenetic and replacement therapy. 11. Outcomes of SDR. 12. Definition of the term «pneumonia of the newborn». 13. Features of the aetiology of PN. 14. Oxygen starvation as the basic pathogenetic mechanism at PN. 15. Classification of PN. 16. The basic clinical manifestations of PN, features of various forms. 17. Features of the pneumonia depending upon etiologic factor. 18. Features of the pneumonia depending upon the term of infection. 19. Outcomes of PN. 20. The basic therapeutic approaches to PN. 21. Principles of the antibiotic prescription to the newbor having PN. 22. Rehabilitation and dispensary supervision at PN. Сongenital infections (TORCH – infections) 1. Urgency of the theme: Congenital infections (CI) are transmitted to a fetus in ante- and intranatal periods. During the last decade, despite the progress in diagnostics and treatment of CI, we can trace their growth. Infectious pathology is one of the leading causes of stillbirth and 28 perinatal death of babies. It leads to a necessity of profound studying of diagnostic methods, treatment and prevention of CI. 2. Specific aims: А. Student must know: 1. CI definition. 2. Aetiological structure of CI. 3. Basic pathogenetic stages of infectious process of CI’s development. 4. Clinical signs of CI. 5.Features of clinical symptoms at cytomegalovirus infections, toxoplasmosis, chlamydiosis, mycoplasmosis, herpetic infections, rubella. 6. Features of clinical symptoms of CI depending upon the term of fetus’ infection. 7. Auxillary methods of CI diagnostics. 8. Methods of CI’ treatment depending on infectious agent. 9. CI prevention. B. A student must have the abilities to: 1. Discover typical anamnestic data and clinical symptoms of CI. 2. Make a differential diagnosis between CI and other newborns’ diseases. 3. Make a differential diagnosis between separate forms of CI. 4. Make a plan of examining a sick person having CI. 5. Make a plan of treating a sick person having CI. 3.Tasks for student’s self-work to prepare for practical studies. 3.1. The list of basic terms, parameters, descriptions, which students must master preparing for lessons. Term 1. CI Definition Congenital infections 2. HSV Herpes simplex virus 3. Blastopathies Affection (infectious) in a blastogenesis stage. As a rule it is concluded with miscarriage. 4. Embryopathy 5. Fetopathy Affection on a stage of embryogenesis. It is ended with a forming of small and big congenital defects. Affection on a stage of fetogenesis. More frequent generalized affection with typical 29 symptoms for infectious agent. 6. TORCH Congenital infections (cytomegalovirus, herpetic, toxoplasmosis, listeriosis, mycoplasmosis, rubella). 7. PCR(polymerase chain reaction) Method of DNA/RNA diagnostics is a complete equivalent of cultural methods of agent’s excretion. 8. Innate CMV CMV – herpetic virus №5, antenatal transplacental infection. 9. Children’s CMV contamination > 90% - In an antenatal period 5% - in an intranatal period 1% - in a postnatal period 10. Opportunistic infection Clinical manifestations are possible only in the case of immunodeficiency. 11. Chlamydia Representative of intermediate existence form. 3.2. Thereotical questions for the lesson: 1. CI definition. 2. CI frequency among other newborns’ diseases. 3. Etiological structure of CI. 4. Features of fetus’s inflammatory process depending on gestation term. 5. Channels of CI’s infection. 6. Features of fetus and newborns’ immunity. 7. Fetoplacental barrier influence on fetus infections. 8. Basic pathogenetic links of CI’s development. 9. General clinical symptoms which are typical for CI. 10. Clinical features of separate CI (cytomegalovirus infections, toxoplasmosis, chlamydiosis, mycoplasmosis, herpetic infections, rubella and other). Meaning of additional investigations in CI diagnostics. CI complications. 11. Possibilities of laboratory and instrumental diagnostics. 12. The principles of CI therapy. 13. Prevention of CI. Bacterial infections in the newborn 1. Theme urgency: During the last years the problem of sepsis has got a special urgency. It is caused by the application of modern methods of treatment and occurrence persistent to antibiotics gram negative flora (intrahospital) that has led to increase of disease and death rate from this serious illness. 2. Specific goals: А. Student should know: 1. Definition of the term "sepsis". 2. Classification of purulent-septic diseases and sepsis at children. 30 3. Etiopathogenesis of sepsis. 4. Clinical signs of "minor" purulent-septic diseases at newborns. 5. Clinical signs of sepsis at children. Additional methods for confirming the diagnosis. 6. Features of the course of septicemic and septicopyemic septic forms. 7. Principles of treatment of purulent-septic diseases and sepsis at children of early age. 8. Principles of rendering the urgent help at an infectious-toxic shock. 9. Consequences of purulent-septic diseases and sepsis at children. 10. Dispensary supervision over children who have suffered sepsis. В. Student should be able:: 1 To diagnose clinical signs of pyoinflammatory process, including sepsis in the child. 2 3 To appoint investigation to the child for confirming the diagnosis. To diagnose "sepsis" according to classification. 4 To evaluate additional methods of investigation. 5 To carry out differential diagnostics of sepsis with other purulent-septic diseases. 6 To make the plan of investigation of person having sepsis. 7 To make the plan of treatment of person having sepsis. 8 To apply deontological receptions during gathering of complaints and the anamnesis. 3. Tasks for students` self-dependent work during preparation for the classes. 3.1. List of main terms, parameters, characteristics, which students has to master preparing for the classes. The term Definition 1. Syndrome of the systemic inflammatory answer Complex of symptoms which includes the general intoxication, signs of respiratory insufficiency (tachypnea, apnea), tachycardia, clinical manifestations of perinatal encephalopathy, leucocytosis or leucopeny, increase in level of C-reactive protein.. 2. Septic shock Occur in the case of decompensation of haemodynamics at patients with the syndrome of the systemic inflammatory answer. 31 3. Multiple organ failure Simultaneous disorders of function of two and more organs and systems as a result of the syndrome of the systemic inflammatory answer. 4. Staphylodermia Pyoinflammatory damage of the skin of staphylococcal aetiology. 4. Septicemia Clinical variant of sepsis without formation of foci of purulent inflammation. Predominate general toxic manifestations. 5. Septicopyemia Clinical variant of sepsis with the formation of not less than two local pyoinflammatory sites (pneumonia, otitis, omphalytis, meningitis, etc.) 6. Passive immunotherapy Administaration to the child specific or not specific antibodies. This method is used predominantly at children. 7. Active immunotherapy Administaration to the child agents which stimulate production of own antibodies 3.2. Theoretical questions for classes: 1. Definition of the term "sepsis". 2. Definition of the term "minor" purulent-septic diseases 3. Etiopathogenesis of sepsis and purulent-septic diseases. 4. Sepsis classification. 5. Clinical manifestations of purulent-septic diseases (vesiculopustulosis, impetigo neonatorum, Ritter`s exfoliative dermatitis, conjunctivitis, omphalytis, umbilicytis, osteomyelitis, etc.). 6. Clinical manifestations of septicopyemic and septicemic septic forms. 7. Features of the course depending upon the causative agent. 8. Laboratory diagnostics of purulent-septic diseases and sepsis at children. Value of the blood count, urinalysis, inoculation of pathological material, blood inoculation on sterility, biochemical and immunological blood tests. 9. Treatment and prophylaxis of purulent-septic diseases and sepsis at children. 10. Prophylaxis of purulent-septic diseases and sepsis at infants. DIABETES MELLITUS AT CHILDREN 1.Urgency of the theme: Insulin-dependent diabetes mellitus (DM) is one of the most widespread diseases of endocrine system at children and adolescents. In Ukraine there is more than 5 thousand children having diabetes. Thus it is annually registered from 500 to 1000 cases of again revealed sick children which forms 5-10 per 100 thousand children's population of Ukraine. DM is chronic disease, basis of which is quickly progressing absolute or relative insulin insufficiency and hyperglycemia, which causes severe metabolic disorders, up to development of comas. High morbidity, severity of the course of the disease, fast progressing development of complications, disability and high death rate of persons of young and mature age, having DM in the childhood, define an urgency of a problem of type I diabetes. 32 Timely diagnostics and the organisation of contemporary adequate treatment of type I diabetes at children allow not only to improve quality of a life of person, having incurable disease, but also considerably increase the life time. 2. Specific goals: A.Student should know: 1. Definition of "diabetes mellitus ". 2. Classification of DM at children. 3. Contemporary considerations on the aetiology and pathogenesis of diabetes: Value of genetic factors . Value of infectious diseases. Immunity disorder. Value of pancreatic diseases. Value of mental and physical factors. 4. Clinical symptoms of different variants of diabetes course at children. 5. An insulin-dependent diabetes at children. 6. A latent diabetes at children. 7. A manifested diabetes at children. 8. Criteria of compensation of diabetes at children. 9. Contemporary requirements to insulin-therapy of diabetes. 10. Complications of insulin-therapy, prevention and treatment. 11. Principles of dietotherapy of diabetes mellitus at children. 12. Principles of urgent help at different kinds of comas in children. 13. Principles of dispensary measures of children having DM. B.Student should be able: 1. To develop the scheme of diagnostic search at DM. 2. To take the history of the patient with DM. 3. To examine the patient. 4. To evaluate the laboratory data. To choose from analyses the data which testify the DM. 5. To reveal clinical criteria of diagnosis of different forms of DM. 6. To formulate the developed clinical diagnosis according to classification. 7. To make the differential diagnosis of diabetes with other childhood diseases. 8. Make a differential diagnosis of DM’s comas with comas of other origin. 9. To appoint treatment taking into account the disease form. 10. To carry out disease prophylaxis. 8. Tasks for student’s self-work to prepare for practical studies. 3.1. The list of basic terms, parameters, descriptions, which students must master preparing for lessons. Term 1. Preprandial glycemia 2. Postprandial glycemia 3. Glycosuria 4. Tolerance to carbohydrates 5.Glycosylated haemoglobin (НвА1, НвА1с) Definition Fasting blood glucose level. N - 3, 3-5,5 Mmol/l Blood glucose level after food intake. N - 4, 47,0 Mmol/l Urine glucose level. N - 0. Ability of carbohydrates uptake; it is defined by means of glucose tolerance test. Defines quality of control of the disorder of carbohydrate metabolism. N - до 6%. 33 6. DM compensation (optimal glycemic control) 15. Analogues of insulin of long action (Lantus, Levemir). (are not allowed in treatment of children till 6 years). 16. Рh of arterial blood. Fasting glycemia 7, 0-9,0, Mmol/l postprandial 11, 1-14,0 Mmol/l, at night – no less < 3,6 Mmol/l, НвА1<7,6%. Fasting glycemia 4, 0-7,0 Mmol/l, postprandial 5, 0-11,0 Mmol/l, at night- no less < 3,6 or >9,0 Mmol/l, Нва1 7, 6-9,0 %. Fasting glycemia >9,0 Mmol/l, postprandial>14,0 Mmol/l, at night -< 3,0 or >11,0 Mmol/l, НвА1 >9,0 %. Quantity of the product which contains 12 g of light carbohydrates. Beginning of action: 30 (10-20) minutes, action peak: 1-3 hour, the maximum duration of action: 6-8 (3-5) h. Beginning of action: 1-2 hour, action peak: 4-12 hour, the maximum duration of action: 18-24 hour. Beginning of action: 0, 5-1,0 h., action peak: 5-9 h., the maximum duration of action: 18-24 h.. Beginning of action: 0,5-1,0 h., action peak: 5-9 h., the maximum duration of action: 18-24 h. Beginning of action: 10-20 min., action peak: 13h., 4-12 hour., the maximum duration of action: 18-24 hour. Beginning of action: 1, 0-2,0 h., without peak, the maximum duration of action: 11-24 hour (Lantus), 16-24 hour (Levemir). 7,34 17. Urine ketones Negative 18. Serum ketones 0, 6-1,7 Mmol/l 19. Plasma’s osmolation 300 mоsm/l 7. DM subcompensation (suboptimal glycemic control) 8. DM decompensation (glycemic control of high risk) 9. Grain unit 10. Insulin of short action (Actrapid NM, Humulin Regular, Insuman Rapid) and its analoges ( Novorapid, Epaidra, Humalog) 11. Insulin of long action (Protafan NM , Humulin NPH, Insuman Bazal) 12. Preliminary mixed 30/70 (Mikstard 30/70, Humulin М3) 13.Preliminari mixed 50/50 14 Preliminari mixed analog of insulin. (Novomix 30) 3.2. Theoretical questions for lessons: 1. DM definition. 2. DM classification at children. 3. Etiopathogenetic theories of DM at children. 4. Clinical symptoms of DM in children. 5. Criteria of the diagnosis. 6. Contemporary principles of DM therapy at children. 7. Principles of DM dietotherapy at children. 8. Requirements to insulin therapy of DM at children. 9. Complications of insulin therapy, prevention and treatment. 10. DM comas. 11. Principles of the urgent help at various kinds of comas at children. 12. Principles of dispensary methods of children having DM. THYROID DISORDERS AT CHIDREN 34 1. Theme urgency: For the recent years there is significant increase in the amount of children and adults with thyroid hyperplasia. Any physician should be able to identify thyroid disease and evaluate its function. This issue is urgent because untimelydiagnostics and the beginning of treatment of thyroid disorder can cause severe irreversible processes and can form children disability. 2. Specific purposes: А. Student has to know: 1. Principles of regulation of human endocrine system. 2. Characteristics of endocrine system at children 3. Classification of thyroid disorders at children. 4. Clinical findings consistent with hypothyroidism, hyperthyroidism. 5. Contemporary methods of hypothyroidism, hyperthyroidism diagnostics. 6. Clinical findings consistent with inflammatory processes of thyroid gland. 7. Clinical and laboratory characteristics of autoimmune thyreoiditis. 8. Contemporary principles of preventive measures, prophylaxis and treatment of thyroid disorders. 9.Principles of rendering treatment at urgent states at thyroid diseases. В. Student has to be able to: 1. Identify thyroid disorder 2. Formulate diagnosis at thyroid gland diseases according to contemporary classifications. 3. Conduct treatment of thyroid diseases. 4. Give emergency medical care to children having thyroid disorders. 9. Tasks for students` self-dependent work during preparation for the classes. 3.1. List of main terms, parameters, characteristics, which students has to master preparing for the classes. Term Diffuse nontoxic goiter Diffuse toxic goiter Thyrotoxicosis Hyperthyroidism Hypothyroidism Endemic goiter Definition Diffuse enlargement of thyroid gland without disorder of its function. Disease with increased secretion of thyroid hormones, diffuse enlargement of thyroid gland and ophthalmopathy. Syndrome, causes by prolonged Т4 and Т3 elevation in blood and tissues with typical clinical findings. Increased secretion of thyroid hormones by thyroid gland. Decreased secretion of thyroid hormones by thyroid gland. Enlargement of thyroid gland, which is observed at most of people, who live in geographic areas with insufficient amount of iodine in the environment. 3.2. Theoretical questions for classes: 1. Features of regulation of endocrine system in childhood. 35 2. Functions of thyroid gland hormones. 3. Classification of thyroid disorders. 4. Definition of terms «diffuse toxic goiter, hypothyroidism, autoimmune thyroiditis, endemic goiter». 5. Clinical findings consistent with hypothyroidism 6. Clinical findings consistent with hyperthyroidism. 7. Clinical findings suggesting congenital hypothyroidism. 8. Clinical findings suggesting diffuse toxic goiter 9. Clinical findings consistent with autoimmune thyroiditis. 10. Methods of thyroid disorders diagnostics in childhood. 11. Principles and methods of treatment of thyroid gland diseases. 12. Emergency states at thyroid disorders. Providing medical assistance. 13. Dispensary observation at children having thyroid diseases. Hypothalamic-pituitary and genital glands disorders 1. A theme urgency: During the last years there is considerable increase in the quantity of children having obesity, different clinical forms of growth and sexual glands disturbances. The prevalence of endocrine pubertal disorders of girls and boys is increasing. This is caused by influence of many exogenous and endogenous factors, with adverse ecological conditions. The endogenous causes can be from constitutional to severe endocrine disorders. They negatively affect the condition of almost all organs and systems, markedly reduce quality of life of the child. The urgency of this question is underlined by that untimely (late) diagnostics and an initiation of treatment of diseases can lead to development of severe irreversible processes and formation of children disability. Timely diagnostics and treatment of such pathology warns development of severe complications at adulthood. 2. Specific goals: А. Student should know: 1. Developmental stages of endocrine system at children 2. Mechanisms of regulation of hormone secretion, their biological action, interconnection with other systems. 3. The nomenclature of diseases of hypothalamic-pituitary system at children. 4. Clinical signs suggesting hypothalamic-pituitary disfunction at children. 6. Treatment of hyper- and hypofunction of adenohypophysis at children. 7. The causes of obesity at children. 8. Classification of obesity at children. 9. Diagnostical and differential-diagnostical criteria of obesity. 10. Principles of management and rehabilitation measures at obesity at children 11. Classification and clinical manifectations of syndromes with growth delay at children 12. Methods of diagnostics and treatment of syndromes with growth retardation. 13. Definition of term “pubertal delay”. 14. The causes of different forms of endocrine disorders of the sexual development. 36 15. Clinical signs of disorders of sexual development at children. 16. Treatment, preventive and rehabilitation measures of children with sexual development dysfunction. 17. Dispensary principles and rehabilitation of such children. В. Student should be able: 1. To evaluate physical development of the child. 2. To make the plan of investigation of children, having adenohypophysis and hypothalamicpituitary dysfunction, growth delay and obesity. 3. To diagnose diseases, which are accompanied by adenohypophyseal disfunction. 4. To reveal signs of hypothalamic-pituitary dysfunction. 5. To carry out differential diagnostics of growth delay at children 6. To diagnose diseases, which are accompanied by growth delay 7. To appoint treatment to the child, having growth delay. 8. To render the urgent help to children with hypothalamic-pituitary diseases. 9. To diagnose childhood obesity of different age. 10. To formulate the obesity diagnosis according to contemporary classification. 11. To make the differential diagnosis between different forms of obesity at children. 12. To appoint management of various forms of obesity at children. 13. To carry out obesity proprylaxis at children 14. To diagnose dysfunction of sexual development. 15. To deftermine clinical forms of the delayed puberty. 16. To appoint treatment to the patient with the dysfunction of sexual development.. 17. To appoint rehabilitational measures to a child with the disorder of sexual development. 10. Tasks for students` self-dependent work during preparation for the classes. 3.1. List of main terms, parameters, characteristics, which students has to master preparing for the classes. 1. Term 1. Short stature 2. 3. 4. 5. 2. Subnanism 3. Nanism 4. Dwarfism 5. Pituitary nanism 6. 6. Hypothalamic (cerebral) nanism 7. 7. High stature 8. 9. 10. 8. Subgigantism 9. Gigantism 10. Obesity 11. 11. Hypopituitarism Definition Growth delay on 1-2 standard deviations (SD, δ) for corresponding age and sex (gender). Growth delay on 1-2 SD for corresponding age and sex. Growth delay >3 SD bellow the mean. Growth at men does not exceed 130 sm, at women - 120 sm. Disease which develops owing to primary insufficiency of growth hormone (GH) secretion. Disease which is characterised by growth delay owing to growth hormone (somatotropin) deficiency, caused by decreased secretion of somatotropin-relizing hormone in hypothalamus. Body length above the mean on 1-2 standard deviations (SD, δ) for the given age and sex. Body length above the mean on 2-3 δ for the given age and sex. Body length above the mean >3 δ for the given age and sex. Chronic relapsing disease which is manifested by excessive accumulation of fatty tissue and is a consequence of the disbalance of consumption and an expense of energy at persons with successive susceptibility or at its absence. Endocrine disease caused by partial or entire insufficiency of secretion 37 12. 12. Diabetes insipidus 13. 13. Pubertal delay 14. 14. Precocious puberty 15. 15. True precocious puberty 16. artificial (unreal) precocious puberty 17. Isolated telarche 16. 17. 18. 18. Isolated adrenarche (pubarche) of adenohypophyseal hormones. The disease caused by deficiency of antidiuretic hormone (АDH) vasopressin. Is diagnosed, if occurrence of cardinal signs of puberty in the teenager lags behind from standard for 2 years and more. Occurrence of secondary sexual signs on isosexual type at girls before 7 years, at boys - before 9 years. Premature sexual development which is causes by premature excessive secretion of gonadotropic hormones by pituitary gland. Premature sexual development which is causes by excessive secretion of sexual hormones. Breast enlargement at girls before 7 years without other signs of premature sexual development. Early occurrence of only secondary genital hairiness at girls before 8 years, at boys - before 9 years, without other signs of premature sexual development. 3.2. Theoretical questions for classes:: 1. Developmental stages of endocrine system at children. 2. Mechanisms of regulation of hormone secretion, their biological action, interconnection with other systems. 3. The nomenclature of diseases of hypothalamic-pituitary system, disorders of sexual development and obesity at children. 4. Clinical signs suggesting hypothalamic-pituitary disfunction at children. 5. Treatment of hyper- and hypofunction of adenohypophysis at children. 6 The causes of obesity at children. 7. Classification of obesity at children. 8. Diagnostical and differential-diagnostical criteria of obesity 9. Principles of management and rehabilitation measures at obesity at children . 10. Classification and clinical manifestations of syndromes with growth delay at children 11. Methods of diagnostics and treatment of syndromes with growth retardation. 12. Definition of term “pubertal delay” 13. The causes of different forms of endocrine disorders of the sexual development. 14. Dispensary principles and rehabilitation of such children. Fe, protein, vitamin deficiency anemia in children 1. Actuality of the topic: Anemia is one of the most widespread forms of hematological pathology in children. Over 50% of childish population are suffering Fe deficiency anemia. Starting at early age anemia takes relapsing course and causes formation of heavy complications. Anemia at early age should be considered as a risk factor which influences acute respiratory diseases, pneumonia, rachitic diseases. These diseases occur 3-5 times more often in children with anemia than in healthy children. Correct and timely determination and treatment of anemia prevents development of heavy complications and consequences. These facts explain actuality of the present topic. 38 2. Certain purposes: А. A student should know: 1. Definition of term “anemia” 2. Classification of deficiency anemias in children 3. Etiopathogenetical peculiarities of deficiency anemias at early age 4. Importance of development factors in different forms of anemias 5. Causes of Fe deficiency development in a child’s body 6. Causes of vitamin deficiency (vit.В12) development, folic acid, proteins in a child’s body 7. Pathogenesis of deficiency anemias in children 8. Laboratory signs of Fe, vitamin, protein deficiency anemias 9. Differential diagnosis of various deficiency anemias 10. Principles of therapy of deficiency anemias in children 11. Peculiarities of administration Fe-therapy in children of early age 12. Principles of prophylaxis of deficiency anemias at child’s age 13. Outcomes of different anemias in children В. A student should be able: 1. To develop a scheme of diagnostic search in cases of anemia 2. To take patient’s blood disease anamnesis 3. To carry out patient’s objective study 4. To estimate laboratory data. To choose among analyses those which testify to anemia 5. To determine clinical diagnosis criteria in cases of different anemia forms 6. To represent detailed clinical diagnosis according to the classification 7. To carry out differentiated diagnosis of anemia and other blood diseases in children 8. To administer adequate treatment taking into consideration the form of the disease 9. To carry the disease prophylaxis 10. To use deontological principles while taking anamnesis, objective patient’s check 11.Tasks for self-study work while preparing for the lesson. 3.1. List of basic terms, medicines, characteristics which a student should master while preparing for the lesson: Term Definition Fe deficiency anemia Decrease of hemoglobin levels in circulating blood due to Fe deficiency in the body Anemic syndrome Symptoms: languor, fatiguability, decrease of appetite, asthenia , skin pallor, tachypnea, tachycardia, weakening of heart sounds, abnormal systolic sound, in heavy cases – delay in growth and mental activity Symptoms: dryness, skin pigmentation, hyper-keratosis of knee and cubital areas, dystrophy of hair, nails, caries without particular symptoms, distortion of smell and taste, angular stomatitis, atrophic glossitis, расстройства digestion disorders, blue scleras. mild - Hb 110-91 g/l moderate - Hb 90-71 g/l heavy - Hb 70-51 g/l very heavy - Hb 50 g/l and less Reveals hemoglobin saturation of erythrocyte. Norm 0.85-1.5 Syderopoenic syndrome Degree of severity of IDA Color index Serum Fe Conditionally responses to amount of Fe bound with transferrin. Norm 39 in infants: 5.0-19.0 mkmol/l > 1 month: 10.6-33.6 mkmol/l General Fe-binding serum ability Characterizes general amount of Fe which can be bound with serum transferrin. Norm 40.6-62.5 Transferrin saturation index Specific gravity of serum Fe from all serum Fe-binding ability Norm – not less than 17%. Day dose of elementary Fe for per os administration is (according to WHO): For children – younger than 3 years old - 3-5 mg/kg/day – 4-7 years old - 50-70 mg/day – over 7 years old - 100 mg/day Formula for calculation of elementary Fe course dose in case of per os administration: BW( (78-0.35( Hb), where BW – body weight (kg) Нb – child’s hemoglobin (g/l) Course dose of Fecontaining medicine (CDM): Number of injections throughout the course: CDM = CDF : FCM, where CDF – course dose of Fe (mg); FCM– Fe content (mg) in 1 ml of medicine CDM : DDM, CDM – course does of medicine (ml) DDM – daily dose of medicine (ml) Syderoacrestic anemia Anemia caused by enzyme disorders in hemoglobin synthesis and defects of Fe inclusion in heme at high Fe level in serum Megaloblastic anemia Group of anemias with ineffective erythroporesis characterized by disorders in maturing and morphological changes in erythrocytes Folic-deficiency anemia (FDA) Can be caused by deficiency of folic acid in food В12 – deficiency anemia (В12 –DA) Can be caused by deficiency of vitamin В12 in food 3.2. Theoretical questions to the lesson: 1. Definition of term “anemia” 2. Classification of deficiency anemias in children 3. Etiopathogenetical peculiarities of deficiency anemias at early age 4. Importance of development factors in different forms of anemias: deficiency of Fe and other microelements deficiency in B-group vitamins deficiency of folic acid protein deficiency congenital and genetic factors acute and chronic pathologies 5. Clinical symptoms in various forms of deficiency anemias in children 6. Patient’s check-up for anemia: clarification of complaints 40 revealing typical data from anamnesis objective patient’s check-up 7. Importance of additional check-up methods for diagnosing anemia 8. Principles of anemia therapy in children 9. Medicines with Fe in therapy 10. Prophylaxis of deficiency conditions in children 11. Outcomes of different anemias HEMOBLASTOSES AT CHILDREN 1. Theme urgency: Hemoblastoses and leukemias for instance remain one of the most important problems of contemporary hematology. Childhood hemoblastosis has been diagnosed more often then other malignant diseases. Each tenth person, having hemoblastosis, is a child. Peak of disease incidence is mostly observed at age period of 2-5 years (80%). Prevalenceof hemoblastoses on the average makes 6-8 cases on 100.000 children's population per year. Hemoblastoses are a huge group of blood diseases of malignant origin, which is interpreted as malignant neoplasms of lymphatic and blood tissues. Hemoblastoses are divided into 2 main groups: leukemias and malignant lymphomas depending upon systemic or regional affectionof blood tissue. Acute lymphoblastic leukemia (ALL) is the most prevalent form of childhood hemoblastosis; it is registered with frequency of 3-5 children on 100 000 children's population per year. ALL represents about 30% of all oncology diseases. More often this disease is observed at 35 years of age. ALL morbidity in this age group is 10 times more often registered than morbidity in other age groups. Acute myeloid leukemias are less prevalent childhood malignancies: its prevalence is 0,7 cases per 100.000 children population per year on average. Chronic myeloleukemia – is malignant disease of blood system, which is originated from myeloid sprout of blood production. Granulocytes, predominantly mature forms, are main tumor pathological components. In childhood chronic myeloleukemia is observed at 2-5% cases of leukemia and is the only malignant process, which has precise chromosome disorders. Hodgkin`s disease is malignant neoplastic disease of lymphatic system. Childhood Hodgkin`s disease takes second place in prevalence after acute leukemia among hemoblastosis and first place among malignant lymphomas. In childhood and youth age periods lethality among hemoblastoses achieves 50% of all amount of lethal cases in oncology. So all this statements proves urgency of learning current theme. 2. Specific purposes А. Student has to know: 1. Definition of term «hemoblastosis». 2. Classification of childhood hemoblastosis. 3. Definition of terms “leukemia”, " myeloleukemia ", “ myeloleukemia ” 4. Contemporary classifications of leukemia, myeloleukemia, myeloleukemia at children. 5. Etiopathogenetical features of the development of leukemia, myeloleukemia and Hodgkin`s disease at children. 6. Clinical findings consistent with different variants of hemoblastosis course at children. 7. Cytomorphological forms of hemoblastosis at children - Acute lymphoblastic leukemia - Acute mieloblastic leukemia - Acute monoblastic leukemia. - Acute mielomonoblastic leukemia - Acute erithroleukemia. - Chronic leukemia 41 - Hodgkin`s disease 8. Clinical and laboratory diagnostic criteria of hemoblastosis at children. 9. Principles of management of different forms of childhood hemoblastoses. 10. Outcomes of different forms of hemoblastoses at children. В. Student should be able: 1. To develop the scheme of diagnostic search at blood disease. 2. To take history of patient, having blood disease.. 3. To carry out objective investigation of the patient. 4. To evaluate the laboratory data. To choose from analyses the data, which confirm hemoblastosis. 5. To be able to reveal clinical criteria of the diagnosis at different clinical forms of hemoblastoses. 6. To formulate the developed clinical diagnosis according to classification 7. To make differential diagnostics with other blood diseases at children. 8. To appoint treatment, taking into account the clinical form of disease.. 9. Principles of prophylaxis of disease recurrence. 10. To use deontological principles during collecting of the anamnesis, objective investigation of the sick child. 3. Tasks for students` self-dependent work during preparation for the classes. 3.1. List of main terms, parameters, characteristics, which students has to master preparing for the classes. Term 1. Hemoblastoses 2. Leukemias 3. Malignant lymphomas (hematosarcomas) 4. Acute leukemia 5. Chronic leukemia Definition The big group of blood diseases of tumorous origin, or a neoplasm of lymphatic and hematopoietic tissue. Malignant tumorous diseases of hematopoietic system with primary localisation in a marrow. Group of diseases which belongs to primary localised tumours of lymphatic system. Disease at which there is a tumorous transformation and impetuous growth of young blast cells. Disease at which development of tumorous cells reaches to differentiated mature (or ripened) forms: plasmocytes, red (blood) cells, lymphocytes. Leukemia with tumorous transformation and impetuous growth of young blast cells. Leukemia, with insufficiency of marrowy hematopoiesis caused by replacement of normal hematopoietic cells by malignant cells. Malignant lymphoma which affects not only lymphatic system, but also can affect nonlymphatic organs and tissues. Not specific for lymphogranulomatosis tumorous cells. 6. Acute lymphoblastic leukemia 7. Acute mieloblastic leukemia 8.Lymphogranulomatosis, Hodgkin`s disease 9.Uninuclear Hodgkin`s cells 10.Polynuclear Sternberg- Specific for lymphogranulomatosis tumorous cells. Reeds cells 3.2. Theoretical questions for classes 1. Definition of terms «hemoblastosis», “leukemia”, " myeloleukemia ", “ Hodgkin`s disease” 42 2. Contemporary classifications of hemoblastosis, leukemia, myeloleukemia, Hodgkin`s disease at children. 3. Etiopathogenetical features of the development of leukemia, myeloleukemia and Hodgkin`s disease in childhood. 4. Clinical manifestations of different variants of outcomes of childhood hemoblastoses. 5. Clinical, laboratory and diagnostic criteria of hemoblastosis at children. 6. Principles of management of different forms of hemoblastoses at children. 7. Outcomes of different forms of hemoblastoses at children. 43