Cases and Questions
advertisement

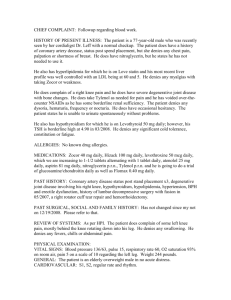
Evaluation of Cardiac Risk Before Noncardiac Surgery CASE 1 AF is a 61 y/o male scheduled for cholecystectomy, for symptomatic gallstones. The surgery is scheduled for 2 weeks from today. The patient has a history of hypertension for the past 16 years. He states that his blood pressure is usually in the 140-150/80-90. One year ago he was admitted to the hospital with chest pain and was diagnosed to have an acute MI. He had a LAD drug eluting stent placed. He was discharged after four days. He denies any chest pain since his MI. He denies dyspnea on exertion, PND, or orthopnea. He is able to walk 4 blocks. He also has a history of hypercholesterolemia. He denies any history of excessive bleeding. His medications are hydrochlorothiazide 25mg qAM, Lipitor 40 mg daily, one aspirin daily, and Plavix. His prior surgery was 35 years ago when he underwent an emergency laparotomy and splenectomy following trauma. Because of his prior laparotomy his present surgeon told him that his cholecystectomy probably cannot be done laparoscopically. He denies any known complications following that surgery. He smoked cigarettes, 3 packs per day for 37 years until quitting when he had his MI one year ago. He denies drinking alcohol. On exam he is in no distress. His blood pressure is 140/90. You repeat his BP and it is 132/82. His pulse is 60 and regular. On HEENT exam, he is PERRLA and EOMI. His neck reveals no JVD and no thyromegaly. His lungs are clear to auscultation and percussion, he has decreased breath sounds bilaterally symmetrically. On cardiac exam S1 and S2 are normal. There is no S3, S4, or murmurs. His abdomen is obese, soft, and nontender, he has a midline scar. His extremities are without clubbing, cyanosis or edema. On neurologic exam cranial nerves 2-12 are intact. His hemoglobin is 16.4. His BMP is normal except for a glucose of 103. His EKG shows NSR with a rate of 60, left axis deviation, and LVH. 1. What are his medical problems? 2. Which if any of these might have a significant effect on the risk of the planned surgical procedure? Why? 1 3. What is the risk of this planned surgery? 4. Should anything be done preoperatively to modify that risk? 5. Is there anything you would recommend perioperatively for this patient? CASE 2 RH is an 82 year old woman scheduled for L total knee replacement. She is referred to your clinic for a preoperative medical evaluation because her blood pressure was elevated on her preadmission screening exam. She states that she had not seen a doctor for 15-20 years until her knee pain started interfering with her walking. She denies a past history of hypertension. She denies a history of chest pain or MI. She is able to walk one block, and then has to stop because of knee pain and fatigue. She denies SOB except when she goes up one flight of stairs. She has slept on two pillows for the past 3 months because that is the only way she is comfortable. Her only medication is advil prn for knee pain. She smoked cigarettes 1 ppd for 40 years until quitting 8 years ago. She does not drink alcohol. She denies prior surgery. On exam she is an elderly female in NAD. Her BP is 160/98 and her pulse is 88. Her RR is 18. On HEENT she is PERRLA and EOMI. Her lungs are clear. Cardiac exam reveals a normal S1 and S2. She has a 2/6 SEM at the apex. Her abdomen is soft and non-tender. Her extremities have 2mm of pitting edema bilaterally. Her EKG shows NSR, Q waves in 2, 3, and AVF, and nonspecific ST segment changes. Her Hb is 13. Her CMP is WNL. 1. What are her medical problems? 2 2 Which if any of these might have a significant effect on the risk of the planned surgical procedure? 3. What is the risk of this planned surgery? 4. What would you recommend to be done at this point? Would you recommend any other tests or treatment? 3