SOAP Note for R-1 Kelly Murray PA
advertisement
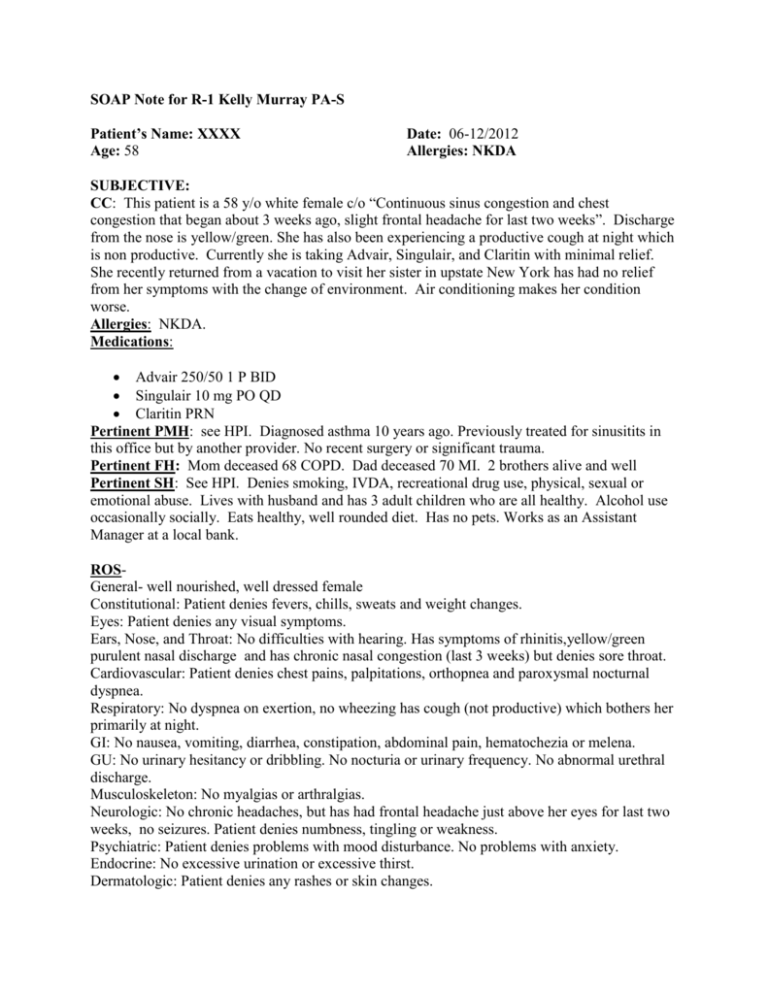
SOAP Note for R-1 Kelly Murray PA-S Patient’s Name: XXXX Age: 58 Date: 06-12/2012 Allergies: NKDA SUBJECTIVE: CC: This patient is a 58 y/o white female c/o “Continuous sinus congestion and chest congestion that began about 3 weeks ago, slight frontal headache for last two weeks”. Discharge from the nose is yellow/green. She has also been experiencing a productive cough at night which is non productive. Currently she is taking Advair, Singulair, and Claritin with minimal relief. She recently returned from a vacation to visit her sister in upstate New York has had no relief from her symptoms with the change of environment. Air conditioning makes her condition worse. Allergies: NKDA. Medications: Advair 250/50 1 P BID Singulair 10 mg PO QD Claritin PRN Pertinent PMH: see HPI. Diagnosed asthma 10 years ago. Previously treated for sinusitits in this office but by another provider. No recent surgery or significant trauma. Pertinent FH: Mom deceased 68 COPD. Dad deceased 70 MI. 2 brothers alive and well Pertinent SH: See HPI. Denies smoking, IVDA, recreational drug use, physical, sexual or emotional abuse. Lives with husband and has 3 adult children who are all healthy. Alcohol use occasionally socially. Eats healthy, well rounded diet. Has no pets. Works as an Assistant Manager at a local bank. ROSGeneral- well nourished, well dressed female Constitutional: Patient denies fevers, chills, sweats and weight changes. Eyes: Patient denies any visual symptoms. Ears, Nose, and Throat: No difficulties with hearing. Has symptoms of rhinitis,yellow/green purulent nasal discharge and has chronic nasal congestion (last 3 weeks) but denies sore throat. Cardiovascular: Patient denies chest pains, palpitations, orthopnea and paroxysmal nocturnal dyspnea. Respiratory: No dyspnea on exertion, no wheezing has cough (not productive) which bothers her primarily at night. GI: No nausea, vomiting, diarrhea, constipation, abdominal pain, hematochezia or melena. GU: No urinary hesitancy or dribbling. No nocturia or urinary frequency. No abnormal urethral discharge. Musculoskeleton: No myalgias or arthralgias. Neurologic: No chronic headaches, but has had frontal headache just above her eyes for last two weeks, no seizures. Patient denies numbness, tingling or weakness. Psychiatric: Patient denies problems with mood disturbance. No problems with anxiety. Endocrine: No excessive urination or excessive thirst. Dermatologic: Patient denies any rashes or skin changes. Reproductive- Menopausal, in monogamous relationship with her husband, no complaints of dyspareunia, vaginal discharge, dryness or irritation. OBJECTIVE: VS: Wt: 147 lbs Hgt: 5’ 7” BP 136/80 P 80 RR 18 Sat 97% Room air General: No acute distress, well nourished. Good attention to hygiene and body habitus. A&O x 3. Eyes: sclera clear, non-injected. Conjunctiva pink. No discharge Ears: No masses, redness, discharge. No tenderness on palpation. Tympanic membrane unobstructed and intact without scarring or bulging. Nose: No tenderness on palpation. Nares patent. Purulent yellow/green nasal congestion visible bilaterally in each nares, skin on nose is irritated form frequent use of tissues. Throat: uvula midline on protrusion, No exudates Sinuses: no tenderness on palpation or percussion. Neck: supple, trachea midline. No bruits, No thyroidmegaly, no lymphadenopathy, no JVD. Cardiac: Inspection: PMI visible at left 5th intercostals space, midclavicular line. no lifts, heaves, rashes, scars Palpation: PMI felt at left 5th intercostals space, midclavicular line. No thrills Auscultation: RRR heard at pulmonic, aortic, mitral, tricuspid and Erb’s point sitting, laying and left lateral decubitus. No murmurs, rubs, clicks, gallops, S3 or S4 Lungs: Inspection: No rashes, lesions, scars, accessory muscle use, labored respirations, 2:1 AP: lateral ratio. Palpation: equal fremitus bilaterally, respiratory excursion equal bilaterally anterior and posterior Percussion: resonant bilaterally anterior and posterior Auscultation: end expiratory wheezing heard BIL anteriorly and posteriorly lower bases. Extremities: No edema, no clubbing of the nails, no discoloration ASSESSMENT: 1. Sinusitis 2. Asthma aggravating Sinusitis PLAN: 1. Keep taking Claritin OTC a. Warned of side effects which include: Headache, abdominal pain, drowsiness, dry mouth fatigue, insomnia, and nervousness. 2. Augmentin 875 mg PO bid for 10 days a. Warned of possible side effects which include diarrhea, rash, mycosis, nausea, vomiting, loose stool, candidiasis, vaginitis, hypersensitivity reactions, anaphylaxis , anemia, thrombocytopenia, leukopenia, agranulocytosis, hepatotoxicity, AST/ALT elevation, pseudomembraneious colitis, serum sickness, abdominal discomfort, cholestatic jaundice, Flatulence) 3.Prednisone 10mg PO qd x 1wk then 5mg PO qd x 1 wk a. Warned of side effects which include: adrenal suppression, psychosis, insomnia, vertigo, pseudotumor cerebri, acne, osteoporosis, myopathy and delayed wound healing, advised patient to drink plenty of fluids and to take with food to advoid stomach upset. If patient still having stomach issues advised to use OTC Prilosec to be able to better tolerate prednisone. 2. Flonase 50mcg/spray, 2 sprays per nostril daily, instructed patient on how to administer. a. Warned of side effects which include: headache, URI, pharyngitis, nasal congestion, nasal discharge, allergic rhinitis, dysphonia, loss of taste. 3. Keep taking Advair, gave sample inhaler of Advair 500/50 1 P BID for two weeks then will back it off to 250/50 1 P BID. a. Warned of side effects which include: palpitations, dizziness, headache, tremor, dermatitis, Hypokalemia, candidiasis, diarrhea, dyspepsia, nausea, vomiting, taste changes, bronchitis, cough, dysphonia, hoarseness, throat irritation, URI, pharyngitis, sinusitis. Patient reminded to rinse mouth after each inhalation to prevent thrush. 4. Albuterol 90mcg inhaler, 2 puffs inhaled PO q 4-6 hours as needed for chest tightness or Wheeze. a. Warned of side effects which include tremor, nausea, fever, bronchospasm, vomiting, headache, dizziness, cough, allergic reactions, otitis media, dry mouth, increase in sweating, increase in appetite, dyspepsia, hyperactivity, lymphadenopathy, ocular pruritus, dysphonia, flu syndrome, nervousness, epistaxis, prolonged QT interval and ST segment depression, tachycardia, sleeplessness, hypokalemia, increased blood glucose levels, hypersensitivity. 5. Come back to office in 3 weeks if not experiencing relief from medications. If you are experiencing new symptoms- such as fever, chills, SOB or hemoptysis call the office immediately. If any adverse reactions occur to drugs, stop the drugs and call the office. If hypersensitivity to drug occurs (anaphylaxis) stop drug and go to the ER immediately. Return to office in 3 months for follow up visit. Kelly L. Murray PA-S 06-12/2012