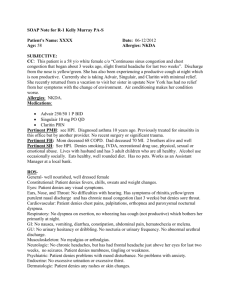
Complete H&P Internal Medicine R4
advertisement

Complete H&P Internal Medicine R4 Elijah Hanna PA-S Lock Haven University PA Program 10/18/12 Name: **** ********* MRN: ######## Race & Gender: Caucasian Female Insurance: Geisinger Gold D.O.B.: 4/05/1925 Date: 10/18/2012 CC: Generalized weakness and cough x’s 3 days HPI: Mrs. ********* is an 87-year-old female that presents to the Lock Haven Hospital ED with a chief complaint of generalized weakness and a cough for the last 3 days. The patient says weakness has been constant over the last three days, and progressively worsened to the point where she is having difficulty with ambulation today. Patient admits to also feeling feverish with the chills, but denies sweats, lightheadedness, focal weakness, or confusion. Patient’s cough has also gotten progressively worse, and patient claims that initially the cough was unproductive but is now productive of green sputum and is quite frequent. Patient also admits to SOB that has progressively gotten worse over the last three days to the point that the patient says she will even get SOB at rest now. Patient denies any nasal congestion/rhinitis, sinus pressure, post nasal drainage, sore throat, swollen nodes, chest pain, palpitations, nausea, vomiting, diarrhea, constipation, black or bloody stools, abdominal pain, dysuria, foul smelling/discolored urine or lower extremity edema/pain. Patient denies taking anything for the weakness, cough, fever, chills or SOB. Patient denies anything that makes these symptoms any worse, and denies ever feeling like this before. Patient’s son presented to the visit and confirms that she is far below her baseline in terms of strength. Patient lives on her own and independent with her ADLs, but can’t ambulate without assistance today. Patient and patient’s son deny any history of weakness, bleeds, cancers, or respiratory conditions. PMH: Paroxysmal Atrial Fibrillation without anticoagulation therapy, which was diagnosed in 2008. Hypertension diagnosed in 1994, which is well controlled with prescription medication. Osteoporosis diagnosed in 2010 supplemented by prescription medication. Patient denies any history of congenital diseases, anemia, CVA, DM, CAD, CHF, cancers, COPD, asthma, pneumonias, TB, GI bleeds or diagnoses, or renal disorders. Immunizations: Up to date. Gets a yearly influenza vaccine (most recent was 9/24/12). Had pneumococcal vaccination done in 2009, and has gotten it every 5 years since turning 65 years old. Injuries: Left femur fracture secondary to osteoporosis in 2010. Left distal radius fracture in the 1980’s. Surgeries: Appendectomy in 1960’s. Total hysterectomy in 1980’s (elective). Hospitalizations: For appendectomy in 1960’s, for hysterectomy in 1980’s, for paroxysmal atrial fibrillation in 2008, and for left femur fracture in 2010. Medications: Actonel 150 mg PO once a month, Amiodarone 200 mg PO QD, Aspirin 81 mg PO QD, Azor 10/40 mg PO QD, Calcium 500 mg PO QD, Coreg 25 mg PO BID, HCTZ 25 mg PO QD, Lisinopril 20 mg PO QD, Nortryptyline 10 mg PO QD, Oxazepam 50 mg PO QID, Vitamin D 1000 U PO 3x’s/week, Vytorin 10/20 mg PO QD, Centrum Multivitamin PO QD, and no other vitamins, herbs, or OTC medications. Allergies: Demerol (hives), Codeine (hives), Ibuprofen (nausea, abdominal pain), Penicillin (hives), Prilosec (nausea, abdominal pain), Sulfa Drugs (hives). Family History: Father, Deceased at 75-years-old from MI Mother, Deceased at 80-years-old from CVA Sister, Alive at 83-years-old, Hx. Of DM 2, TIA, Hyperlipidemia Brother, Deceased at 86-years-old from Alzheimer’s Disease Daughter, Alive & well at 62-years-old Son, Alive & well at 65-years-old Social History: Patient is widowed x’s 10 years and lives by herself at a private residence. Patient is no longer sexually active. Patient is independent with her ADLs and still has an active social life with card night, bingo night, and book club. Patient’s son lives close and often checks on her and helps her with strenuous labor around the house. Patient smoked ~1/2pack/day for 10 years through the early 1950’s in to the 1960’s, but hasn’t smoked or used any form of tobacco since. Patient denies any alcohol or illicit substance consumption or abuse ever. Patient is retired x’s 20 years and was a high-school English teacher for 42 years. Patient is financially stable. Patient eats a well-balanced diet and cooks for herself. Patient hasn’t traveled away from PA since the 1990’s. R.O.S.: General: Patient is positive for weakness, fevers, and chills as noted in HPI. Patient denies any confusion, weight gain/loss, appetite loss, difficulty sleeping or night sweats. Skin: Patient denies any rashes, itching, bruising, dryness, redness or lesions. Patient denies any changes to any hair, skin or nails. HEENT: Patient denies any diplopia, blurred vision, visual disturbances, hearing loss, tinnitus, ear pain/pressure/drainage, sinus pressure/drainage, nasal congestion/drainage, post nasal drip, sore throat or swollen nodes. Respiratory: Patient is positive for a productive cough and SOB at rest as noted in the HPI. Patient denies any hemoptysis, chest tenderness, or history of TB exposure. Cardiac: Patient is positive for DOE for the last three days, and is also SOB at rest as noted in HPI. Patient denies any chest pain, palpitations, orthopnea, PND, murmurs, or history of cardiac abnormalities/complications. Abdominal: Patient denies any abdominal pain, N/V/D/C, black or bloody stools, changes in BM activity or characteristics, or any history of GI bleeds/complications. Genitourinary: Patient denies any dysuria, increased urinary frequency, urinary retention/incontinence, foul smelling or discolored urine. Patient had total hysterectomy in 1980’s. No sexual activity since 2001 before her husband died. Musculoskeletal: Patient is positive for generalized weakness. Patient denies any focal weakness, muscle or joint pain, swelling, redness, or increased warmth. Patient usually walks without assistance, but needs a walker or wheelchair today. Endocrine: Denies any polyuria, polydipsia, polyphagia, heat/cold intolerance, or history of any endocrine disorders including the pituitary, thyroid, parathyroid, thymus, pancreas, or adrenal glands. Patient denies any history of any vitamin or nutrient deficiencies. Neurological: Patient denies any confusion or changes in sensation, perception or alertness. Patient denies any focal weakness or abnormalities. Physical Exam: General: Patient is A&O x’s 3. (+) Slightly labored breathing. (+) Weak/sickly/ emaciated appearance. No acute distress. Ambulatory with assistance. Appears as stated age. Patient is mild mannered, well spoken, and has no difficulty with speech or socializing. Vital Signs: Temperature-99.2 F (TM), RR-20 bpm, HR-84 bpm, BP- 110/66, SpO2%- 90%. Skin: No rashes, lesions, ecchymosis, eruptions, erythema, swelling, or dryness noted. The hair is in appropriate distribution, smooth and well kept. The nails have no clubbing, merckes lines, beaus lines, thickening, pallor or pitting. HEENT: Normocephalic, atruamatic head. Eyes are bilaterally PERRLA, EOM intact, with visual acuity 20/20 with corrective lenses, and no discharge, dryness, or nystagmus. Ear canals are patent with no erythema or cerumen impaction. TMs bilaterally are visualized as intact, without perforation, fluid levels, bubbles, bulging or erythema. Nasal turbinates are patent without discharge. Oral mucosa is (+) dry and pink with no lesion, erythema, tonsillar hypertrophy, or exudates. Neck is negative for carotid bruits and JVD, supple, trachea is midline, and no thyromegaly or masses felt. Chest/Lungs: Inspection reveals no scars, lesions, masses, accessory muscle use or asymmetrical chest wall movement. AP:Lateral ratio is 1:2 with no intercostal retractions. Percussion revels symmetrical respiratory excursion and no dullness. Chest is non-tender to palpation. Tactile fremitus reveals suggested consolidation at bilateral lower lobes. Auscultation reveals (+) slightly diminished breath sounds throughout with bilateral crepitations and expiratory wheezing at both lower lobes. (+) Whispered pectoriloquy and egophony noted at the bases bilaterally. Cardiac: Inspection of precordium reveals no lifts, heaves or visible PMI. Palpation reveals no lifts, heaves, or thrills. Auscultation reveals regular rate and rhythm, S1 and S2, and no gallops, clicks, rubs, or murmurs. Abdomen: Inspection of the abdomen is (+) for scars from appendectomy and hysterectomy with no visible pulsations, striae, ascites, lesions or obvious masses. Auscultation reveals no abdominal aortic, renal, external iliac, or femoral arterial bruits. Bowel sounds are heard in all four quadrants of consistent quality and intensity. Percussion reveals no hepatosplenomegaly, tenderness, or masses. The bladder was unable to be percussed. Palpation reveals no tenderness, masses, hepatosplenomegaly, or enlargement of the abdominal aorta. The kidneys were able to be trapped bilaterally and unsuggestive of any tenderness, hypertrophy, or masses. No CVAT. Rectal: Inspection reveals no obvious masses, lesions or bleeding. Appropriate sphincter tone, minimal soft brown stool in rectal vault, and (-) FOBT. Musculoskeletal: Inspection reveals a thin, elderly lady with equal, bilateral, diffuse muscle atrophy and no fasiculations or cramps visualized. No joint erythema, edema, increased warmth, or decreased active or passive ROM. Patient able to ambulate with assistance of a walker, but not independently. Strength is 4/5 throughout in her upper and lower extremities. No focal weakness observed or felt. Neurological: Sensation is intact with appropriate recognition of sharp v. dull and light touch in bilateral upper and lower extremities. Cranial nerves II-XII intact. (-) Romberg test. Appropriate rapid/alternating movements, heel to shin, and reflexes equal at +2 bilaterally for triceps, patellar, and achilles. Lymphatic: No occipital, post/pre-auricular, submandibular, subtonsillar, submental, posterior cervical, anterior cervical, supra/infra-clavicular, axillary, or inguinal lyhmphadenopathy. Labs/Imaging: Chest X-ray- Bilateral lower lobe infiltrates suggestive of pneumonia. Mild cardiomegaly. WBC Count- 22,000 Neutrophils-94% Na+- 121 K+-4.0 Cl- -100 BUN/Cr- 33.0/1.3 Hgb- 10.4 Hematocrit-36.4 U/A- WNL EKG-NSR Troponin- <.01 BRNP- 206 Assessment: 1. Bilateral Lower Lobe Community Acquired Pneumonia 2. Hyponatremia with hypochloremia, likely secondary to dehydration 3. Acute on Chronic Renal Insufficiency secondary to dehydration 4. Hypertension 5. Hx. Of Paroxysmal Atrial Fibrillation 6. Hx. Of Osteoporosis Plan: Pending Labs: Repeat CBC and CMP every 24 hours. Sputum culture and sensitivity. Blood Cultures x’s 2. Pending Imaging: None Referrals/Consults: Admit to ICU for telemetry. Consult nephrology and Dr. Bermudez for acute on chronic renal insufficiency. Treatment: Nasal cannula O2 to keep SpO2% above 94%. Normal saline 125 cc/hour IV. Levaquin 750mg IV over 90 minutes every 24 hours. Protonix 40 mg IV QD. Continue all previous medications. Patient Education: Patient educated on pneumonia and need for IV antibiotic treatment due to advanced disease progression and patient’s age. Patient educated on hyponatremia and hypochloremia and possible consequences of low levels. Patient given a chance to ask questions, but has none and a good handle on current condition. Provider Notes: Most likely Strep pneumoniae because it is CAP. Will check sputum culture and sensitivity. Make sure not to fluid overload through diluted antibiotics because of renal insufficiency. Admission Orders: Admit To: ICU under Dr. Adroja’s care Diagnosis: Bilateral lower lobe pneumonia, hyponatremia and hypochloremia most likely secondary to dehydration, acute on chronic renal insufficiency, Hx. of paroxysmal atrial fibrillation, hypertension, and osteoporosis. Condition: Fair/Poor Vitals: Taken q3hrs including Temperature, HR, RR, BP and SpO2% Activity: OOB to Chair with assistance Nursing: Strict I/O’s, Daily bottom and back checks, SCDs. Call house officer if T>99.5 F, HR>105, RR>26, SBP>160 or <90, UOP<30mL/hr, or any critical high or low lab values. Diet: Regular diet, low salt after hyponatremia corrected Allergies: Demerol (hives), Codeine (hives), Ibuprofen (nausea, abdominal pain), Penicillin (hives), Prilosec (nausea, abdominal pain), Sulfa Drugs (hives). No known food allergies. Labs: CBC and CMP q 24 hours in the AM. IVF: Normal Saline Solution 125mL/hour Studies: Repeat CXR in 36-48 hours. Meds: Continue all previous medications. Protonix 40 mg IV once daily. Levofloxacin 750 mg IV over 90 minutes once daily. Elijah Hanna PA-S 10/18/12