DOC - Foundations In Herbal Medicine
advertisement
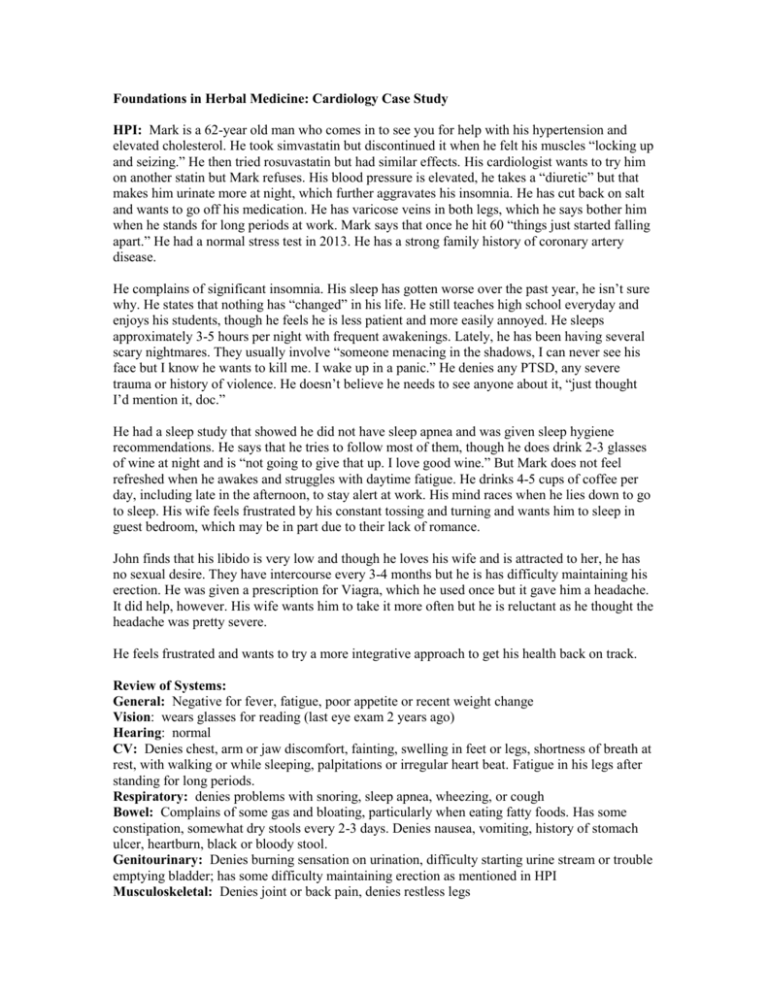
Foundations in Herbal Medicine: Cardiology Case Study HPI: Mark is a 62-year old man who comes in to see you for help with his hypertension and elevated cholesterol. He took simvastatin but discontinued it when he felt his muscles “locking up and seizing.” He then tried rosuvastatin but had similar effects. His cardiologist wants to try him on another statin but Mark refuses. His blood pressure is elevated, he takes a “diuretic” but that makes him urinate more at night, which further aggravates his insomnia. He has cut back on salt and wants to go off his medication. He has varicose veins in both legs, which he says bother him when he stands for long periods at work. Mark says that once he hit 60 “things just started falling apart.” He had a normal stress test in 2013. He has a strong family history of coronary artery disease. He complains of significant insomnia. His sleep has gotten worse over the past year, he isn’t sure why. He states that nothing has “changed” in his life. He still teaches high school everyday and enjoys his students, though he feels he is less patient and more easily annoyed. He sleeps approximately 3-5 hours per night with frequent awakenings. Lately, he has been having several scary nightmares. They usually involve “someone menacing in the shadows, I can never see his face but I know he wants to kill me. I wake up in a panic.” He denies any PTSD, any severe trauma or history of violence. He doesn’t believe he needs to see anyone about it, “just thought I’d mention it, doc.” He had a sleep study that showed he did not have sleep apnea and was given sleep hygiene recommendations. He says that he tries to follow most of them, though he does drink 2-3 glasses of wine at night and is “not going to give that up. I love good wine.” But Mark does not feel refreshed when he awakes and struggles with daytime fatigue. He drinks 4-5 cups of coffee per day, including late in the afternoon, to stay alert at work. His mind races when he lies down to go to sleep. His wife feels frustrated by his constant tossing and turning and wants him to sleep in guest bedroom, which may be in part due to their lack of romance. John finds that his libido is very low and though he loves his wife and is attracted to her, he has no sexual desire. They have intercourse every 3-4 months but he is has difficulty maintaining his erection. He was given a prescription for Viagra, which he used once but it gave him a headache. It did help, however. His wife wants him to take it more often but he is reluctant as he thought the headache was pretty severe. He feels frustrated and wants to try a more integrative approach to get his health back on track. Review of Systems: General: Negative for fever, fatigue, poor appetite or recent weight change Vision: wears glasses for reading (last eye exam 2 years ago) Hearing: normal CV: Denies chest, arm or jaw discomfort, fainting, swelling in feet or legs, shortness of breath at rest, with walking or while sleeping, palpitations or irregular heart beat. Fatigue in his legs after standing for long periods. Respiratory: denies problems with snoring, sleep apnea, wheezing, or cough Bowel: Complains of some gas and bloating, particularly when eating fatty foods. Has some constipation, somewhat dry stools every 2-3 days. Denies nausea, vomiting, history of stomach ulcer, heartburn, black or bloody stool. Genitourinary: Denies burning sensation on urination, difficulty starting urine stream or trouble emptying bladder; has some difficulty maintaining erection as mentioned in HPI Musculoskeletal: Denies joint or back pain, denies restless legs Skin: denies any skin disorders, or new rashes or lesions Neurological: Denies lightheadedness, unsteady gait, frequent or severe headaches (except with Viagra as mentioned in HPI), dizziness, or seizures. Mental Health: Admits he sometimes feels mildly depressed, which he describes as sad and overwhelmed. Only lasts a couple days and then “he pulls himself out of it.” Denies suicide ideation. He is having nightmares (~ four in last 3 months) and feels more tense and less patient at work. Endocrine: Denies excessive intolerance to cold or heat or excessive thirst or frequent urination Bleeding: denies history of blood clots in legs or lungs, or excessive bruising or bleeding Cardiac risk factors: - hypertension, - diabetes mellitus, -tobacco use. He has a strong family history of CAD. + hyperlipidemia +waist circumference 39 inches Allergies: No known allergies Medications: aspirin 325 mg every day, diphenhydramine (Benadryl) 50 mg at night for sleep Family History: Father died at age 64 from heart attack, mother passed away age 69 after stroke. He has 1 sister that is alive. Sister, age 58, has diabetes and coronary artery disease. Social History: Married for 32 years. He has one daughter, age 29 who is married and lives in Chicago. He enjoys his wife’s company. She works as a second grade teacher. He has been a high school math teacher since he graduated college. He enjoys his work, though, he finds the days are long and the kids more unruly. Past Medical History: 1. Hyperlipidemia 2. Hypertension 3. Insomnia Past Surgical History: 1. Tonsillectomy (age 5 for recurrent sore throats) Smoking history: He does not smoke cigarettes. He smoked pack/day from ages 18-46. Caffeine intake: he drinks 4-5 cups of coffee Alcohol intake: 2-3 servings wine 7 nights per week Exercise: does not do any exercise Spirituality: Raised Lutheran. Has no active practice. “Not interested. We’re here, we live, we die. The end.” Relaxation: watches football and other television shows, usually with his wife. Supplements: does not take any supplements Stress level: Rates himself 8 on a scale of 1-10 (10 being considerable stress) Mental health: Rates himself 7 on a scale of 1 to 10 (10 being depressed) Sleep habits: Goes to bed around 9 PM and watches TV until around 11. Falls asleep for 1-2 hours. Wakes up and can’t go back to sleep until around 4 AM. Then falls asleep until around 6 AM when he gets up to get ready to go to work. Takes Benadryl to help with sleep. Has never taken prescription sleep aids. Nutrition He eats 2-3 servings of vegetables in an average day. He eats 0-1 servings of fruit in an average day. He eats fried or "fast" food 5/week times a week. He eats red or processed meat 4-5 times a week. Height: 6 feet 2 inches, weight 255 pounds, BMI 32.81 BP 142/84, HR 68 bpm Appearance: Well dressed man in no apparent distress, looks his age. Speech is clear and appropriate. Affect is somewhat flat. Gait is steady and coordinated. HEENT: Pupils equal, react to light and accommodation. Neck: No JVD appreciated. No carotid bruits bilaterally, no thyromegaly Cardiac: S1S2, regular rate and rhythm, no S3 or S4 appreciated. Pulmonary: Bilaterally clear without wheezes, rales or rhonchi Abdomen: soft, nontender, no masses appreciated, no heptasplenomegaly, bowel sounds present Extremities: No edema, pulses present; 2+ dorsalis pedis and 2+ posterior tibial pulses, varicose veins very pronounced in lower legs bilaterally Skin: No rashes, lesions Neuro: Non- focal, cranial nerves 2-12 intact Labs: LDL: HDL: Triglycerides: hs-CRP: 176 mg/dL 44 mg/dL 266 mg/dL 3.1 CHEM20: normal Thyroid panel: normal Vitamin D: 19 ng/ml