A 22-year-old female is admitted very distressed and short of breath
advertisement

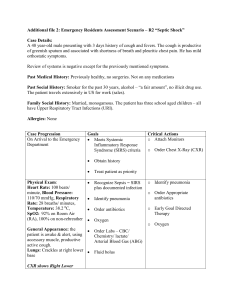
A 22-year-old female is admitted very distressed and short of breath. Examination reveals a respiratory rate of 35/min, a pulse of 120 beats per minute, a blood pressure 110/70 mmHg, oxygen saturations of 90% and a peak expiratory flow rate < 50% predicted. The emergency medical services have administered salbutamol 5 mg (twice) and face mask oxygen. Which of the following is the most appropriate next action in this patient? (Please select 1 option) Arterial blood gas analysis Incorrect answer selected Intensive care referral Oxygen 35% Prednisolone 40 mg Salbutamol 5 mg and ipratroprium bromide 0.5 mg This is the correct answer According to British Thoracic Society guidelines addition of ipratroprium would be the next step in the case of this lady with acute severe asthma. Prednisolone would be administered shortly thereafter. 35% oxygen is inadequate and a maximal concentration should be used. A blood gas is not essential for management particularly with the oxygen saturations of 90% although these will be performed. Intensive care referral may well be appropriate if this lady does not improve. Managment of Acute severe Asthma... A 22-year-old male is admitted wheezing with a respiratory rate of 35/min, a pulse of 120 beats per min, blood pressure 110/70 mmHg, peak expiratory flow rate < 50% predicted. The emergency medical services have administered salbutamol 5 mg (twice), ipratroprium 0.5 mg and face mask oxygen. His arterial blood gas reveals: pH 7.42 (7.36-7.44) PaCO2 5.0 kPa (4.7-6.0) PaO2 22 kPa (11.3-12.6) Base excess -2 mmol/L (+/-2) SpO2 98 Which of the following is the most appropriate action for this man? (Please select 1 option) Chest X-ray Incorrect answer selected Intensive care referral This is the correct answer Ipratroprium Magnesium 1-2 g Oxygen 35 % In this case the patient is showing signs of respiratory decompensation. A normal or raised PaCO2 in an asthmatic is a warning of impending respiratory failure as the patient becomes too tired to ventilate adequately and ITU need to be notified. Administration of magnesium would be the next therapeutic measure. A chest x-ray will be helpful but should not delay in treatment and referral. 35 % oxygen is inadequate. A 72-year-old lady presented after taking an overdose of a sustained-release propranolol preparation. She has a pulse of 40 bpm and a BP of 90/60 mmHg. She was given atropine by the emergency department staff but there has been little response. Which of the following is the most appropriate treatment? (Please select 1 option) Atropine Glucagon Correct Haemodialysis Noradrenaline Salbutamol "For cases of beta-blocker poisoning where symptomatic bradycardia and hypotension are present, high-dose glucagon is considered the first-line antidote." Am J Health Syst Pharm. 2006 Oct 1;63(19):1828-35 A 23-year-old man with known peanut allergy presented to the emergency department with anaphylaxis. He has a swollen face and lips. His BP is 90/60 mmHg, pulse 110 bpm and he is wheezy. Which of the following formulations of adrenaline should be given? (Please select 1 option) 0.5 ml of 1:10000 adrenaline IM 0.5 ml of 1:1000 adrenaline IM Correct 5 ml of 1:1000 adrenaline IM 10 ml of 1:10000 adrenaline IV Nebulised adrenaline "For adults, a dose of 0.5 mL adrenaline 1: 1000 solution (500 micrograms) should be administered intramuscularly, and repeated after about five minutes in the absence of clinical improvement or if deterioration occurs after the initial treatment especially if consciousness becomes - or remains impaired as a result of hypotension. In some cases several doses may be needed, particularly if improvement is transient." Resuscitation Council UK. Adult EpiPen which allergy sufferers can carry with them contains 0.3 mg adrenaline in a 1:1000 dilution for intramuscular (IM) injection. A 45-year-old lady with a history of depression presented to the emergency department drowsy. Her repeat prescription says she is taking diazepam and dosulepin and the ambulance crew say that she has taken an overdose of her medication. Her BP is 140/80 mmHg, pulse 130 bpm, respiratory rate 7 per minute and O2 sats 98% on air. Which of the following is the most appropriate next action? (Please select 1 option) Give flumazenil Incorrect answer selected Give naloxone Obtain an ECG This is the correct answer Refer for urgent haemodialysis Start N-acetylcysteine infusion This is a tricky case and will catch those who go for the first answer they see that is reasonable. The urge is quickly to treat the drowsy patient with respiratory depression with some sort of antidote, but there needs to be a diagnostic step first. Tricyclic antidepressants can cause fatal arrhythmias and seizures which are very difficult to manage. An electrocardiogram (ECG) would immediately indicate if there is a risk of significant tricyclic toxicity by showing a wide QRS complex or abnormal axis deviation. A 17-year-old girl presents following an overdose of paracetamol, her parents having found her with empty packets of paracetamol. She states that she has taken 100 tablets, three hours earlier. Which is the most appropriate step in this patient's management? (Please select 1 option) Administer oral activated charcoal 50g Give N-Acetylcysteine (NAC) intravenously This is the correct answer Measure plasma paracetamol concentration Incorrect answer selected Transfer to young person's psychiatric unit immediately Take no immediate action This patient has taken a huge paracetamol overdose only three hours previously so the paracetamol level would be pointless until after four hours. Also we know that she has taken a huge dose and that she needs urgent treatment. As absorption of paracetamol can be prevented by activated charcoal if given within two hours of ingestion it may be too late to use in this case. But generally algorithms suggest using NAC as early as possible. However, you would usually give activated charcoal as well particularly if she had taken the paracetamol with alcohol which may delay absorption. A 27-year-old lady collapses in the Emergency Department after being admitted with numerous seizures. You obtain information from her husband that she has a past history of seizures, but has not had any for the last two years, and is well controlled on valproate. He also informs you that she has been gaining weight recently and has also had erratic menses which the neurology clinic attribute to the valproate. Pulse 110/min Blood pressure 160/90 mmHg Urinalysis 3+ proteinuria After airway, breathing and circulation, the immediate drug therapy should be: (Please select 1 option) Diazepam 10 mg Lorazepam 2 mg Magnesium 2 grams Correct Nil Phenytoin 1000 mg This lady may well be having an epileptic fit, but why should a young woman have an elevated blood pressure and proteinuria? In a woman of this age with raised blood pressure and proteinuria, a diagnosis of eclampsia has to be considered and the primary treatment of eclampsia is the administration of magnesium A 16-year-old girl presented with fever, headache and photophobia. Investigations revealed: Cerebrospinal fluid examination Opening pressure 260 mm H20 (50-180) Total protein 0.8 g/l (0.15-0.45) Glucose 4.2 mmol/l (3.3-4.4) White cell count 60 per ml (<5) Lymphocytes 90% (60-70) Plasma glucose 6.4 mmol/l (3.0-6.0) What is the most likely diagnosis? (Please select 1 option) Bacterial meningitis Cryptococcal meningitis Incorrect answer selected Tuberculosis meningitis Viral encephalitis Viral meningitis This is the correct answer A normal cerbrospinal fluid (CSF) glucose together with a CSF lymphocytosis an increased opening pressure, and a raised CSF protein are typical of a viral meningitis, which would be high on the list of differentials in patients of this age group (together with bacterial meningitis). Further reading: Cerebrospinal Fluid Analysis American Academy of Family Physicians A 45-year-old man attends the Emergency Department with symptoms suggestive of community acquired pneumonia. On examination he is pyrexial at 38.0°C and has a respiratory rate of 32/min, with a blood pressure of 85/55 mmHg. Which of the following combination of features are not necessarily an indication for urgent hospital admission? (Please select 1 option) BP of 85/55 mmHg and respiratory rate of 32/min BP of 85/55 mmHg and urea of 7.5 mmol/l Confusion and BP of 85/55mmHg Pyrexia of 38.0°C and serum urea of 7.5 mmol/l Correct Respiratory rate of 32 and blood urea of 7.5 mmol/l This patient has community-acquired pneumonia. The CURB score can be used in the assessment of severity using core adverse prognostic features which are two from four of: Confusion abbreviated mental test score <8 Urea >7 mmol/l Respiratory rate >30/min Blood pressure: systolic BP <90 or diastolic BP <60. Clinical judgement must still however be used particularly if only one feature is present or if there is co-morbidity such as age over 50 years or chronic cardiac, respiratory or renal disease A 60-year-old man presents with an episode of memory loss. Three days earlier he had become confused. His wife led him into the house - he apparently sat down at her request, and had a cup of tea. He then wandered around the house, confused, but remained conscious and able to have some conversation with his wife, though continuing to ask similar questions repeatedly. After three hours, he abruptly returned to normal and had no recollection of the events. What is the most likely diagnosis? (Please select 1 option) Alcohol related amnesia Chronic subdural haematoma Complex partial status epilepticus Hysterical fugue state Transient global amnesia Correct This is the typical clinical description of transient global amnesia which represents a transient vascular insufficency of both hippocampi. A 19-year-old female with type 1 diabetes is admitted with diabetic ketoacidosis. Which of the following is most appropriate concerning the use of a bicarbonate infusion? (Please select 1 option) Bicarbonate infusion should be considered at pH less than 7 Correct Commence a bicarbonate infusion with a ketone concentration above 5 mmol/l (NR les than 1) Commence bicarbonate infusion with a potassium concentration above 6 mmol/l Commence a bicarbonate infusion with a standard bicarbonate concentration below 5 mmol/l (NR 22-26) No benefit from using a bicarbonate infusion The use of bicarbonate in DKA is controversial (pdf). However, most authorities agree that a bicarbonate infusion may be used in subjects with a severe metabolic acidosis (pH less than 7). An anxious 22-year-old female with a high respiration rate has the following arterial blood gas results: pH 7.27 (7.36-7.44) PCO2 2.6KPa (4.7-6.0) Base deficit 12 mmol/L What is the interpretation of the acid-base status? (Please select 1 option) Combined metabolic and respiratory acidosis Combined metabolic and respiratory alkalosis Metabolic acidosis with some compensatory respiratory alkalosis Correct Respiratory acidosis with some compensatory metabolic alkalosis Respiratory alkalosis with some compensatory metabolic acidosis This patient has a metabolic acidosis as evidenced by a pH of 7.27 and a base deficit, which is a marker of the extent of acidodis. The low CO2 is a reflection of the physiological respiratory compensation which is attempting to normalise pH by clearing the acidic gas CO2. A 21-year-old man, who has a past history of IV drug abuse, presents 12 hours after taking an overdose of 480 mg of codeine and 30 g of paracetamol. His blood pressure is 100/60 mmHg and he has pin-point pupils. What is the most appropriate management for this patient? (Please select 1 option) 500ml 10% glucose IV over four hours 1 litre normal saline IV over six hours IV naloxone IV flumazenil Incorrect answer selected Start N-acetylcysteine This is the correct answer This patient presents 12 hours after taking a potentially fatally toxic dose of paracetamol. In the circumstances provided in this question where there is an absence of data relating to pulse rate (as he is probably not in shock), respiratory rate (reflecting respiratory depression) or blood glucose, the most appropriate intervention at this 12 hour time-point would be N-acetylcysteine. The urgency of treatment is underlined by the fact that the incidence of hepatotoxicity is worse if treatment is delayed. Trials of N-acetylcysteine suggest that the incidence of hepatotoxicity is 1% in those treated within eight hours versus 46% in those treated after 16 hours. A 16-year-old man is brought to the emergency department with a GCS (Glasgow coma scale) rating of 3/15. Within 10 minutes he regained consciousness with a GCS of 15/15, is sitting up and talking. What is he likely to have taken? (Please select 1 option) Inhaled solvent glue Correct Smoked heroin Smoked marijuana Snorted cocaine Taken ecstacy This patient was markedly comatose on arrival but quickly regains consciousness. This suggests a short acting (probably) inhaled anaesthetic-like agent - glue. Marijuana would not be expected to produce this level of coma and the effects of cocaine would last much longer. The inhaled solvents, due to their lipophilicity, are rapidly absorbed through the lungs and then quickly distributed to the brain and other organs. The effects therefore appear within minutes of inhalation. Typical substances that are inhaled include toluene aromatic hydrocarbons and butane. Which of the following percentages most accurately reflects the mortality associated with the modern management of diabetic ketoacidosis? (Please select 1 option) 0.5% Incorrect answer selected 1% 2-3% This is the correct answer 5-6% 8-10% Despite the advances in the management of diabetes in general and the improvements in intensive care, studies reveal that the mortality associated with diabetic ketoacidosis remains stuubbornly around the 2-5% since the 1970s. Specifically mortality relates to cerebral oedema An 18-year-old woman presents three days after allegedly taking 50 paracetamol tablets (25g). Which of the following tests measured at this time point would be most helpful in determining the outcome? (Please select 1 option) ALT concentration Bilirubin concentration Creatinine concentration Paracetamol concentration Prothrombin time Correct The patient has ingested a seriously toxic dose of paracetamol. The best determinant of this risk at 72 hours would be a prolonged prothrombin time. Paracetamol concentrations would be rather meaningless at this time point and irrespective she should be treated with N-acetylcysteine. There are four phases of paracetamol overdose: * Phase 1 (0-24 hours) o Asymptomatic o Anorexia o Nausea or vomiting o Malaise o Subclinical rise in serum aspartate transaminase (AST) - 12 hours post ingestion. * Phase 2 (18-72 hours) o Right upper quadrant abdominal pain, anorexia, nausea, vomiting o Continued rise in serum transaminases levels (note this is the time slot for our patient with the alanine transaminase [ALT] rises). * Phase 3 (72-96 hours) o Centrilobular hepatic necrosis with continued abdominal pain o Jaundice o Coagulopathy o Hepatic encephalopathy o Nausea and vomiting o Renal failure o Fatality rising international normalised ratio/prothrombin time (INR/PT) from three days. * Phase 4 (Four days to three weeks) o Complete resolution of symptoms o Complete resolution of organ failure A 35-year-old business man presented with anxiety and palpitations after having 'snorted' cocaine. The patient who denies any prior use had also consumed some alcohol. On examination, he was distressed and sweating with a temperature of 38°C, a pulse of 138 bpm (regular) and a blood pressure of 216/110 mmHg. His ECG revealed a sinus tachycardia. Which of the following is the most appropriate initial treatment for this man? (Please select 1 option) Dantrolene Diazepam Correct Lidocaine Propranolol Verapamil Cocaine abuse is quite common and neurological and cardiovascular side effects predominate. Delirium, hyperthermia, dysrhythmias, as well as myocardial and cerebral infarctions are reported. In this patient, the first consideration should be attention to airway, breathing and circulation (ABC) and also to remove any residual cocaine from the nares. Generally, the toxic effects of cocaine are short lived and relate to sympathetic stimulation, in this case with tachycardia, pyrexia and hypertension. The most appropriate treatment would be an intravenous (IV) benzodiazepine such as diazepam, which relieves the sympathetic adrenergic overdrive and would be expected to relieve these features including the hypertension. If further treatment is required, IV nitrates can be used and are particularly useful for associated coronary artery spasm. Beta-blockers should be avoided as they may depress cardiac output, which may exacerbate the depressive effect of cocaine A 16-year-old girl is brought to the Emergency Department after having taking drugs at a rave. Which of the following suggests that she has taken Ecstasy (MDMA)? (Please select 1 option) Hypernatraemia Metabolic acidosis Pin-point pupils Pyrexia Correct Respiratory depression The features of ecstasy overdose include: hyperthermia hypertension hyponatraemia due to polydipsia associated with syndrome of inappropriate antidiuretic hormone (SIADH) and respiratory alkalosis. Pin-point pupils suggest opiates A 16-year-old girl presents with bilateral cervical lymphadenopathy. Her lymph node biopsy reveals a nodular sclerosing Hodgkin's disease (HD). Which one of the following features indicates a poorer prognosis? (Please select 1 option) Fatigue Mediastinal mass of 3 cm Night sweats Correct Pruritis Recent Epstein-Barr virus (EBV) infection Important prognostic features in HD are Stage B symptoms: fever/night sweats and weight loss Mass > 10 cm. Therefore although fatigue and pruritus are common, they have no prognostic significance. EBV infection is commonly associated with HD but has no prognostic significance. A 70-year-old female who has a history of chronic anxiety presents with a three day history of severe left temporal headache radiating from the eye to the scalp. She had also experienced discomfort during eating. Which one of the following drugs should be given to this patient while awaiting the results of diagnostic tests? (Please select 1 option) Acyclovir Carbamazepine Diclofenac Prednisolone Incorrect answer selected This is the correct answer Sumatriptan The history suggests temporal arteritis irrespective of the history of anxiety and in view of the sight-threatening nature of the disease, the patient should be commenced on steroids. Although the differential diagnosis is also trigeminal neuralgia steroids should be used here whilst awaiting diagnostic investigations as temporal arteritis may be sight-threatening if left untreated A 20-year-old student is found in her bedroom by friends drowsy, confused and sweating. She is unable to give a clear history. On examination she has a fever of 38.3°C, pulse 110 bpm, BP 110/60 mmHg and she appears short of breath with a respiratory rate of 30. Her chest sounded clear to auscultation. Arterial blood gas result taken on 15 L/min oxygen shows: pH 7.29 (7.35-7.45) Pa O2 16 kPa (11-14) Pa CO2 2.1 kPa (4.5-6) Which of the following is the most likely diagnosis? (Please select 1 option) Aspirin overdose Correct Cocaine use Legionella pneumonia Meningococcal septicaemia Severe asthma There are a number of clues here that point to aspirin toxicity: fever sweating tachypnoea and acidosis. The presence of confusion suggests a severe overdose. In severe asthma and legionella pneumonia hypoxia would be expected. Meningococcal septicaemia does not explain the tachypnoea. A 24-year-old law student attends with visual loss affecting the right eye. She reports a constant headache for the last 3 months, and absence of menses for 6 months. On examination her visual acuity in the right eye is 6/24, with slight constriction of the temporal field in that eye but she has no other neurological deficit. She is afebrile and haemodynamically stable. What is the diagnosis? (Please select 1 option) Glaucoma Migraine Multiple sclerosis Pituitary tumour Correct Pregnancy This patient has a pituitary lesion; the history of headache and amenorrhoea suggests a prolactinoma or non functioning tumour. This has been complicated by involvement of the visual pathway, which has precipitated her visual loss. She needs urgent assessment of her pituitary function, imaging of the pituitary gland by MRI scanning. One of the most important investigations to perform would be a serum prolactin. The amenorrhoea would argue against this being retrobulbar neuritis associated with MS and similarly the peripheral visual field constriction would be unusual as a central scotoma and fluctuating visual loss would be more typical. A 76-year-old with a recent history of cerebral haemorrhage is admitted with a cough, worsening breathlessness and right pleuritic chest pain. He is also mildly pyrexial. His ventilation-perfusion scan reveals several areas of ventilation/perfusion mismatches in the right lower zone. What is the most appropriate line of management? (Please select 1 option) Aspirin therapy Antibiotics Inferior vena cava (IVC) filter This is the correct answer Low molecular weight heparin treatment Incorrect answer selected Warfarin treatment This patient has a pulmonary embolism (PE) following a recent haemorrhagic stroke. The risk of rebleeding into the stroke area is too high with anticoagulation. The best action would be percutaneous insertion of IVC filter which may be as effective as anticoagulation. It is used in cases where anticoagulation is a contraindicated or in those in whom anticoagulation alone fails An 81-year-old female is admitted following a seizure although her relatives state that prior to this she had been increasingly confused, unsteady and unable to look after herself over the last two to three weeks. On examination she was drowsy and had a temperature of 37.5°C, and a blood pressure of 192/108 mmHg. She had a mixed aphasia, with a mild right hemiparesis. What is the most likely diagnosis? (Please select 1 option) Acute cerebral infarction Acute intracerebral haemorrhage Cerebral abscess Chronic subdural haematoma Correct Glioblastoma The history of variable 'confusion' and unsteadiness for some weeks followed by an acute exacerbation is a typical presentation of a subdural haematoma in the elderly population. Cerebral abscess is unlikely due to the absence of significant fever. Acute infarction or acute intracerebral haemorrhage would not explain the two weeks history of confusion and unsteadiness. Astrocytoma usually causes symptoms over months to years. Mixed aphasia (or transcortical mixed aphasia) is, simply, not a complete 'global aphasia'. In global aphasia there is receptive and expressive dysphasia. Further reading on dysphasias ... Patients can often repeat words but not understand commands, name objects or have intelligible spontaneous speech. 'Mixed aphasia' is not specific for stroke, although it can be caused by it. It may be caused by Alzheimer's disease, bilateral cerebral damage, tumours, thalamic lesions and so on. It is an excellent choice of language defect for a 'best of five' question since it is a good distractor A 75-year-old man was admitted after been found collapsed in a garden shed surrounded by a number of empty containers. On clinical examination the patient had small pupils, a heart rate of 50 beats per minute, and was frothing at the mouth. What is the most likely diagnosis? (Please select 1 option) Creosote poisoning Glyphosate poisoning Organophosphorus poisoning Correct Paraquat poisoning Pyrethroid poisoning The patient has cholinergic features with a relative bradycardia, small pupils and increased salivation. This is highly suggestive of organophosphorus poisoning which is an anti-cholinesterase, thus prolonging the effects of acetylcholine. Paraquat is associated with nauseam vomiting and diarrhoea with ulceration. Creosote is a petroleum based substance and would not have such an effect. Glyphosate herbicides produce nausea, vomiting and diarrhoea with a caustic effect in the mouth. Pyrethroid is an insecticide and poisoning is rare but associated with coma, convulsions and pulmonary oedema A 19-year-old girl presents with an overdose of paracetamol. Which of the following statements is correct? (Please select 1 option) Acetylcystine should routinely be given if the presentation is within the first 12 hours of overdose Because she is over the age of six, she is unlikely to develop significant toxicity Hospitalisation will be needed for at least five days Liver function tests should be monitored Correct The mortality in those with an AST of >350 IU/l is 4% Treatment with N-acetyl cysteine (NAC) is given according to a standard nomogram. NAC may be useful up to 36 hours following ingestion. Children under the age of six are unlikely to develop significant toxicity, but adolescents have a higher incidence of toxic plasma levels following ingestion, and a higher incidence of abnormal aspartate transaminase (AST) >1000 IU/l. Even after serious hepatotoxicity, the mortality rate is under 0.5%. The occasional patient may require liver transplantation. Which of the following would be expected features of a left posterior cerebral artery occlusion? (Please select 1 option) A right homonymous hemianopia Correct Decerebrate state Internuclear ophthalmoplegia Pure aphasia (i.e. without alexia) Wernicke's aphasia Internuclear ophthalmoplegia is typical of multiple sclerosis. Wernicke's aphasia and Pure aphasia (i.e. without alexia) are middle cerebral artery. Decerebrate state is most likely a pontine lesion. Other possible findings in posterior left cerebral artery occlusion are: cortical blindness visual hallucinations thalamic syndrome Claude's and Weber's syndrome Which of the following is correct concerning a precordial thump? (Please select 1 option) Can be delivered up to twice during a cardiac arrest Can be given following an unwitnessed cardiac arrest Delivers approximately 10 joules of energy This is the correct answer Should be administered after a warning has been given to the patient selected Incorrect answer Should be aimed at the position of V4 on the anterior chest wall The precise indication for performing a precordial thump is following a witnessed or monitored cardiac arrest. Warning a patient who has arrested will serve little purpose! Only one thump should be delivered (before the first 200 J defibrillatory shock) over the lower third of the sternum. Approximately 7 to 10 joules of energy are delivered with an appropriately weighted thump (potential energy to mechanical energy to electrical energy). A 40-year-old farmer presented to the casualty department with a 24-hour history of fever and increasing confusion. On examination he was febrile 39.5C. A generalised erythematous rash, covering most of his body, was observed. He also had a paronychial infection of his right index finger, with lymphangitis extending caudally and with axillary lymphadenopathy. His heart rate was measured at 120 beats per minute with a blood pressure of 80/60 mmHg. What is the most likely diagnosis? (Please select 1 option) Hantavirus infection Leptospirosis Orf Staphylococcal toxic shock syndrome Correct Stevens-Johnson syndrome The history is typical of staphylococcal toxic shock syndrome (TSS): - shock - fever - confusion and - rash. The primary source of infection in this case is the paronychia of his right index finger. Hantavirus infections (viral zoonoses transmitted via rodents) typically have two distinct presentations: - either as a haemorrhagic fever with renal failure - or as an acute pulmonary syndrome. The former manifestation is commonest in the Far East and eastern Europe, while the latter is the predominant form in the southwestern United States and South America. Leptospirosis does not typically cause a rash and is often associated with jaundice; leptospirosis would not explain the lesion on his finger. Orf, a zoonotic infection caused by a pox virus, presents with painless ulcerated lesions on the hands of farmers, but does not fully explain this clinical picture. Stevens-Johnson syndrome typically starts with an erythema multiforme-type rash that spreads widely and involves the buccal mucosa and conjunctivae; often caused by antibiotic therapy, but does not fit the clinical picture presented here In adult basic life support the correct ratio of chest compressions to ventilations is: (Please select 1 option) 5 to 1 8 to 1 10 to 1 15 to 2 30 to 2 Correct 15 compressions to two breaths was the recommended ratio regardless of the number of rescuers performing basic life support, but the recent guidelines now suggest 30:2. You have been called to the ward by the senior nurse, to review a repeat calcium result. The repeat result is 3.9 mmol/l (2.2-2.6), the previous result four hours earlier was 3.2. The patient has a disseminated malignancy with an unknown primary. Which of the following statements is most correct when considering the hypercalcaemia of malignancy? (Please select 1 option) A prolonged QT interval is associated with hypercalcaemia Bisphosphonates inhibit osteoblast function thereby lowering calcium Calcitonin is of greater benefit than bisphosphonates in the treatment of hypercalcaemia of malignancy NSAIDs are indicated for bone pain in this patient Incorrect answer selected On neurological examination, hyporeflexia may be exhibited This is the correct answer This is an oncological emergency. Hyporeflexia is a common clinical sign in patients with hypercalcaemia. Non-steroidal anti-inflammatory drugs (NSAIDs) should not be prescribed in patients with hypercalcaemia as they reduce renal blood flow thus inhibiting urinary calcium excretion. Bisphosphonates inhibit bone resorption by osteoclasts, and are the first line pharmacological treatment of hypercalcaemia of malignancy; calcitonin use is limited by its association with anaphylaxis. Electrocardiogram changes in hypercalcaemia include bradycardia, prolonged PR interval, short QT interval, widened T waves and arrhythmias. A 65-year-old male presents with acute severe headache, ataxia and vomiting. Six hours later he became drowsy. On examination he had left horizontal nystagmus, a partial left sixth cranial nerve palsy and extensor plantar responses. His blood pressure was 188/110 mmHg. What is the most likely cause for this deterioration? (Please select 1 option) Brain stem herniation Cerebral oedema Dehydration Malignant hypertension Correct Non-convulsive status epilepticus The most likely explanation of the sudden deterioration will be brain stem herniation. The acute onset of symptoms with headache and vomiting indicating an acute intracranial haemorrhage. Mass effect created the brain stem herniation. Intravenous mannitol, intubation/ventilation, urgent computerised tomography (CT) brain scan and neurosurgical referral are indicated. In most cardiac arrest situations 1mg of adrenaline (epinephrine) is given intravenously every three minutes. What is the correct volume and concentration of the adrenaline? (Please select 1 option) 0.1 ml of 1 in 100 1 ml of 1 in 1000 10 ml of 1 in 1000 1 ml of 1 in 10,000 Incorrect answer selected 10 ml of 1 in 10,000 This is the correct answer A 1 mg dose of adrenaline (epinephrine) would be administered with 0.1 ml of 1 in 100, 1 ml of 1 in 1000 and 10 ml of 1 in 10,000. However, 10 ml of 1 in 10,000 is the recommended dose and concentration and is considered the optimum volume of adrenaline during cardiac arrest, and is recommended by the UK Research Council