Hypertension in Pregnancy
advertisement
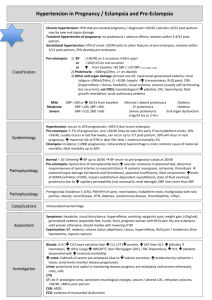
Hypertension in Pregnancy Tony Nicoll Consultant Obstetrician Ninewells Hospital QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Outline • • • • • • • • Objectives Physiology Classification Pre-eclampsia Pathogenesis Management Eclampsia Conclusions QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Objectives • Understand the processes involved in antenatal care, surveillance in pregnancy, and the roles of the professionals involved (Outcomes 1-11) • Demonstrate a knowledge of the common problems encountered in obstetric practice (Outcomes 3,4,5,8) Hypertension in Pregnancy • Hypertension affects 10-15% of all pregnancies • Mild pre-eclampsia affects 10% of primigravid women • Severe pre-eclampsia affects 1% of primigravid women • Eclampsia affects 1/2000 pregnancies • Death from eclampsia = 2% • Pre-eclampsia is the commonest cause of iatrogenic prematurity • Up to 25% of antenatal admissions are due to hypertension Blood Pressure in Pregnancy • Blood pressure (BP) proportional to systemic vascular resistance and cardiac output • Pregnancy Vasodilatation • BP falls in early pregnancy • Nadir reached at 22-24 weeks • Steady rise until Term • BP falls after delivery but subsequently rises and peaks at day 3-4 P/N Hypertension • ≥140/90 mmHg on 2 occasions • DBP >110 mmHg • ACOG - >30/15 mmHg compared to booking BP Hypertension in Pregnancy • Pre-existing hypertension • Pregnancy Induced Hypertension (PIH) • Pre-eclampsia Pre-existing Hypertension • Diagnosis prior to pregnancy • Likely if hypertension in early pregnancy (PET / PIH diseases of second half of pregnancy) • May be retrospective diagnosis if BP has not returned to normal within 3 months of delivery • Consider secondary causes - renal / cardiac, Cushing’s, Conn’s, Phaeochromocytoma • Risks include PET (X2), IUGR and abruption PIH • Second half of pregnancy • Resolves within 6/52 of delivery • No proteinuria or other features of pre-eclampsia • Better outcomes than pre-eclampsia • 15% progression to pre-eclampsia - depends on gestation • Rate of recurrence is high Pre-eclampsia Pre-eclampsia • Hypertension • Proteinuria (≥0.3g/l or ≥0.3g/24h) • Oedema • Absence does not exclude the diagnosis Pre-eclampsia • A pregnancy-specific multi-system disorder with unpredictable, variable and widespread manifestations • May be asymptomatic at time of first presentation • Diffuse vascular endothelial dysfunction widespread circulatory disturbance • Renal / Hepatic / Cardiovascular / Haematology / CNS / Placenta Pathogenesis • Genetic predisposition • Stage 1 - abnormal placental perfusion • Stage 2 - maternal syndrome Pathogenesis • Abnormal placentation and trophoblast invasion failure of normal vascular remodelling • Spiral arteries fail to adapt to become high capacitance, low resistance vessels • Placental ischaemia widespread endothelial damage and dysfunction • Mechanism unclear (??oxidative stress / PGI2 : TXA2 imbalance / NO) • Endothelial Activation • • • • • Capillary Permeability Expression of CAM Prothrombotic Factors Platelet aggregration Vasoconstriction NonPregnant Preeclampsia Normal Placentation A Multi-system Disorder • • • • • • • CNS Renal Hepatic Haematological Pulmonary Cardiovascular Placental CNS Disease • • • • • • Eclampsia Hypertensive encephalopathy Intracranial haemorrhage Cerebral Oedema Cortical Blindness Cranial Nerve Palsy Renal disease • • • • • • GFR Proteinuria serum uric acid (also placental ischaemia) creatinine / potassium / urea Oliguria /anuria Acute renal failure • acute tubular necrosis • renal cortical necrosis Liver Disease • Epigastric/ RUQ pain • Abnormal liver enzymes • Hepatic capsule rupture • HELLP Syndrome Haemolysis, Elevated Liver Enzymes, Low Platelets • high morbidity/ mortality Haematological Disease • • • • • Plasma Volume Haemo-concentration Thrombocytopenia Haemolysis Disseminated Intravascular Coagulation Cardiac / Pulmonary Disease • Pulmonary oedema ARDS • iatrogenic • disorder related • Pulmonary Embolus • High mortality Placental Disease • Intrauterine growth restriction (IUGR) • Placental Abruption • Intrauterine Death Symptoms • • • • • Headache Visual disturbance Epigastric / RUQ pain Nausea / vomiting Rapidly progressive oedema • Considerable variation in timing, progression and order of symptoms Signs • • • • • • • • Hypertension Proteinuria Oedema Abdominal tenderness Disorientation SGA IUD Hyper-reflexia / involuntary movements / clonus Investigations • Urea & Electrolytes • Serum Urate • Liver Function Tests • Full Blood Count • Coagulation Screen • CTG • Ultrasound - biometry, AFI, Doppler Management • Assess risk at booking • Hypertension < 20 weeks - look for secondary cause • Antenatal screening - BP, urine, MUAD • Treat hypertension • Maternal & fetal surveillance • Timing of Delivery • PIH can be managed as O/P in Day Care Unit Risk Factors • Maternal Age (>40 years 2X) • Maternal BMI (>30 2X) • Family History (20-25% if mother affected, up to 40% if sister) • Parity (first pregnancy 2-3X) • Multiple pregnancy (Twins 2X) • Previous PET (7X) • Molar Pregnancy / Triploidy • Multiparous disease women develop more severe Medical Risk Factors • Pre-existing renal disease • Pre-existing hypertension • Diabetes Mellitus • Connective Tissue Disease • Thrombophilias (congenital / acquired) Predicting Pre-eclampsia Normal MUAD Notch Maternal Uterine Artery Doppler 20 - 24 weeks Antenatal Screening • When to refer to AN DCU? BP 140/90 (++) proteinuria oedema symptoms - esp persistent headache • For every 1000 “Low-risk” patients: 100 hypertensive 60 normal - 20 will return 20 DCU follow up - 10 admitted 20 admitted When to admit? 1. BP >170/110 OR >140/90 with (++) proteinuria 2. Significant symptoms - headache / visual disturbance / abdominal pain 3. Abnormal biochemistry 4. Significant proteinuria - >300mg / 24h 5. Need for antihypertensive therapy 6. Signs of fetal compromise Inpatient Assessment • Blood Pressure - 4 hourly • Urinalysis - daily • Input / output fluid balance chart • 24 hour urine collection - if proteinuria on urinalysis • Bloods - FBC, U&Es, Urate, LFTs. Minimum X2 per week Fetal Surveillance • Fetal Movements Normal • CTG - daily AEDF • Ultrasound Biometry Amniotic Fluid Index Umbilical Artery Doppler REDF Treatment of Hypertension • Treat regardless of aetiology • With MAP ≥150 mmHg there is significant risk of cerebral haemorrhage • Most treat if BP ≥150/100 mmHg • BP ≥ 170/110 mmHg requires immediate Rx • Aim for 140-150/90-100 mmHg • Control of blood pressure does not reduce the risk of developing pre-eclampsia Treatment of Hypertension Mode of Action Starting Dose Maximum Dose Contraindications Breast Feeding Methyl Dopa Centrally acting agonist 250mg bd 1 gram tds Depression Yes Labetolol + antagonist 100mg bd 600mg qid Asthma Yes Nifedipine SR Ca channel antagonist 10mg bd 40mg bd Yes Hydralazine Vasodilator 25mg tds 75mg qid Yes (Avoid Diuretics / ACE Inhibitors) When to Deliver? • The only cure for pre-eclampsia is delivery • Mother must be stablised before delivery • Consider expectant management if pre-term • Most women delivered within 2 weeks of diagnosis Indications for Delivery • Term gestation • Inability to control BP • Rapidly deteriorating biochemistry / haematology • Eclampsia • Other Crisis • Fetal Compromise - REDF, abnormal CTG Crises in Pre-eclampsia • • • • • • • • • Eclampsia HELLP syndrome Pulmonary Oedema Placental Abruption Cerebral Haemorrhage Cortical Blindness DIC Acute Renal Failure Hepatic Rupture Steroids • Promote fetal lung surfactant production • ↓ neonatal respiratory distress syndrome (RDS) by up to 50% if administered 24-48h before delivery • Administer up to 36 weeks • Only significant effects up to 34 weeks. Proven benefit up to 1 week • Betamethasone preferred to Dexamethasone • 1 course = 12mg Betamethasone IM X2 injections 24 hours apart Eclampsia Eclampsia • Tonic-clonic (grand mal) seizure occuring with features of pre-eclampsia • >1/3 will have seizure before onset of hypertension / proteinuria • Ante-partum (38%) / Intra-partum (16%) / postpartum (44%) • More common in teenagers • Associated with ischaemia / vasospasm Management of Severe PET / Eclampsia • Control BP • Stop / Prevent Seizures • Fluid Balance • Delivery Antihypertensives • IV Labetolol • IV Hydralazine • Beware hypotension – fetoplacental unit Seizure Treatment / Prophylaxis MAGNESIUM SULPHATE Loading dose: 4g IV over 5 minutes Maintenance dose: IV infusion 1g/h If further seizures administer 2g Mg SO4 If persistent seizures consider diazepam 10mg IV Fluid Balance • Main cause of death = pulmonary oedema (Capillary leak / fluid overload / cardiac failure) • Oliguria in 30%. Does not require intervention • Any doubts about renal function urine osmolality • Fluid challenges are potentially dangerous • Safer to run a patient “dry” - 80 ml/h Labour and Delivery • • • • • • Aim for vaginal delivery if possible Control BP Epidural anaesthesia Continuous electronic fetal monitoring Avoid ergometrine Caution with iv fluids Postpartum Management • • • • • Breast feeding Contraception BP management Counselling Future risk – Depends on other medical factors – Gestation dependent (28/40 - 40%, 32/40 - 30%) • Long term CVD risk Low Dose Aspirin • Aspirin - inhibits cyclo-oxygenase prevents TXA2 synthesis • 75mg Aspirin 15% reduction in PET (NNT=90) • May be more beneficial in preventing severe early onset pre-eclampsia (MRC CLASP Trial) • Safe • Used for high risk women - Renal, DM, APS, Multiple risk factors, previous PET • Commence before 12 weeks NICE Aug 2010 Calcium, Antioxidants & Folic Acid • Calcium supplementation (>1gram / day) may reduce risk of hypertension (30%), PET (52%) and maternal death (20%). Did not affect pre-term birth or stillbirth (Hofmeyr et al Cochrane Database 2006) • Antioxidants not effective (Poston et al. VIP Study, Lancet 2006) • Mid trimester folic acid also appears to be effective in preventing pre-eclampsia (73% reduction) (Wen et al AJOG 2008) Conclusions • Hypertension in pregnancy is common • Pre-eclampsia is a multi-system disorder unpredictable and variable manifestations with • Pathogenesis involves abnormal placentation and widespread endothelial dysfunction • Supportive management requires maternal and fetal surveillance • No cure other than delivery • Maternal risks balanced against risks of prematurity