Haem Module 2
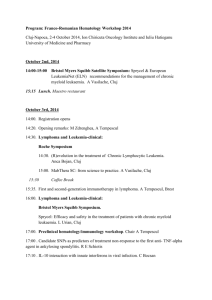
advertisement

2.1 - CHRONIC MYELOID LEUKAEMIA (CML) 1. The clinical features of CML D - CML is a myeloproliferative disease/neoplasm where there is a proliferation of mature myeloid cells in the BM & PB. Although the causative mutations occurs in the pluripotent HSC and hence is present in all cells, the disease primarily manifests as a neutrophilia I A S G A P C - i = 1/100k/year (rare); accounts for 15-20% of all leukaemias - 50-60y - M> F (just) - UNKNOWN; ionising radiation is a known risk factor - [see below] s/s/e 20-40% of patients are asymptomatic (chronic phase of the disease) Increased metabolism = B symptoms (fatigue, weight loss, sweating, normocytic anaemia) Acute leuakaemic symptoms manifest in the blastic phase Hepatosplenomegaly (due to extrameduallry haemopoeises) Investigastions Blood film - mature leucocytosis with blasts <2% of nucleated cells in BM o The majority is neutrophilia; neutrophil may have decrease nuclear lobules and thus appear as band cells o Basophilia may also be present; it is otherwise rare in other causes of leucocytosis Blood count - anaemia. Platelet count may increase as disease progresses (it is very rarely low in the chronic phase) BM aspirate - HYPOCELLULAR o Megakaryocytes can increase in number and appear hypo-lobular o The percentage of erythroid cells falls (increased myeloid:erythroid ratio) o Increased deposition of reticulin fibres o Pesudo Gaucher cells (macrophaged that have phagocytosed other cells) can be present Low Neutrophil ALP used to be another diagnostic tool Diagnosis is based on cytogenetics Management c - monitor white cell count, cytogenetics and molecular genetics. m - imatinib is a useful treatment (interferons used to be used). S - BM transplant is the only cure but it can not be used in all patients P - Imatinib gives a good prognosis on haematological, cytogenetic and molecular grounds 2. CML as a 3 phase disease Phase 1 - Chronic; most patients are in this phase Phase 2 - accelerated o Progression occurs because of additional mutations on top of the background BCR/ABL o Very variable presentation that can take months or years o Suspect progression into accelerated phase if patient: Displays decreased response to treatment % of blasts increases to 10-20% % of basophils increases to 20% Platelet count deranges/ splenomegaly increases Phase 3 - Blastic Phase o Similar to AML, although some develop into a lymphoid leukaemia o % of blasts >20% o Can be fatal 3. The genetic Pathogenesis of CML The hallmark of CML is the Philadelphia chromosome, which is present in 95% of patients. In the remainder, the BCR-ABL fusion gene forms via cryptic translocations involving other chromosomes apart from 9 & 22 The Philadelphia chromosome Translocation of BCR (22q) to ABL (9q) o The result is an elongated tyrosine kinase product which is constiutively expressed 15% of primary ALL patients have the same mutation, but the splice point on the BCR gene is upstream - this produces a smaller gene product BCR/ABL expression in the HSC leads to: o Proliferation & resistance to apoptosis of myeloid lines, particularly neutrophils o Decreased development of lymphoid lineages o Development into accelerated/blastic CML in the context of additional mutations ABL is usually a nuclear protein, but BCR-ABL is cytoplasmic - has the potential to effect a lot of downstream processes directly 2.2 - ACUTE MYELOID LEUKAEMIA (AML) 1. Clinical features of AML D - A clonal expansion of myeloid blasts in the BM or other tissues, where the percentage of blasts reaches >20% of nucleated cells in the BM I A S G A P C - 4/100k/year; accounts for 70% of adult acute leaukaemias - adults; median 60years - M>F (just) - Known risk factors include ionising radiation, benzene, smoking, chemotherapy and possibly viruses s/s/e Features relating to BM failure/ replacement of normal cells in BM by leaukaemic clones o Normocytic Anaemia (fatigue etc) o Neutropenia (infections, mostly bacterial, watch out for sepsis) o Thrombocytopenia (spontaneous bleeds from mucous membranes) BM expansion/ bone impinging on other tissues - Bone pain Features relating to infiltrates of leukaemic clones into other tissues o Organomegaly, gyum hypertrophy, sarcoma Symptoms due to increased metabolism - B symptoms Symptoms relating to electrolyte imbalance following release of intraceullar contents after cell death o Hyperuricaemia, hyperkalaemia o Hypocalcaemia Investigations [see below] Management C - supportive treatments; antibiotics (infections), blood transfusions (Hb), platelet transfusions (bleeding), resuscitate, rehydrate, allopurinol M - Chemotherapyto induce remission, differentiating agents (eg ATRA, arsenic trioxide) can be used in M3 S - BMT P - depends on classification but ‘normal’ prognosis AML is roughly 42% 5 year survival 2. Investigations and classifications in AML 4 main methods in investigation of AML Morphology (blood film) Immunophenotyping (flow cytometry) Cytogenetic analysis (FISH) Molecular genetics WHO classification of AML AML with recurrent genetic abnormalities (translocations; 35% of cases) AML with multi-lineage dysplasia (i.e. following MDS/MPD); worse prognosis Therapy-related AML (secondary to chemo); o alkylating agents - develops 5-10years after drug use after an MDS o topoisomerase II inhibitors - develops 1-5 years after drug use without an MDS AML not otherwise categorized - this has been revised in most recent classification - get it 3. Morphological classification in AML - the FAB system is not enough Classification M0 M1 M2 M3 M4 M5 M6 M7 Description No maturation; immunophneotyping needed to diagnose Minimal maturation Mature cells with upto 90% non-erythroid; Acute promyelocytic leukaemia; t15,17; DIC; good prognosis if treated early Myelomonocytic Monocytic/monoblastic; gum/organ ilfiltrates; hypokalaemia Erythroid; bad prognosis Megakaryoblastic; immunophenotyping needed to diagnose; bad prognosis 4. Immunophenotyping in AML Is needed for the diagnosis of M0/M7 AML o Picks up CD41 and CD61 in M7 Has a role in all laeukaemias as a general point because it can pick up CD33/ CD13/ other myeloid markers Useful in ruling out lymphoid leukaemia if it is negative for CD19 as an example 5. Genetic basis of AML There are 4 main translocations in AML; these account for 35% of the cases Good Prognosis o T8,21 [AML1/ETO] M2 morphology Accounts for 5-12% of cases Presence of auer rods is sufficient to diagnose it on blood film o Inv16 or inter 16 translocation [CBFb/MYH11] M4 morphology Accounts for 10-12% of cases Associated with abnormal marrow eosinophils and large basophil granules o T15,17 [PML/RARa] M3 morphology (promyelocytic leuakaemia) Accounts for 5-8% of cases Bad Prognosis o 11q23 [MLL] mutation Accounts for 5-6% of cases The majority of AML cases are caused by genetic mutations These can occur with or without translocations o FLT3 mutation FLT3 is a gene that is involved in HSC differentiation/proliferation Accounts for 20-40% of cases ITD mutation has worse prognosis than TKD mutation o KIT mutation [poor prognosis] o Nucleophosmin mutation Accounts for 1/3 of cases Mutation leads to nucelophosmin, which usually binds RNA in the nucleus, being expressed in the cytoplasm Better prognosis 2.3 – LAB DIAGNOSIS OF ACUTE LEUKAEMIA: MORPHOLOGY & CYTOCHEMISTRY 1. The initial suspicion of leukaemia comes from signs/symptoms AML o Anaemia, neutropenia, thrombocytopenia o hepatosplenomegaly o Gum hypertrophy, skin infiltrates (M4) o gum haemorrhage, DIC (M3) o Hypopyon (leukaemic cells in anterior chamber of eye) o Recurrent priapism in men ALL o Anaemia, neutropenia, thrombocytopenia o hepatosplenomegaly o lymphadenopathy o thymic enlargement o involvement of testes in men o involvement of CNS 2. Blood film, count and bone marrow aspirate are important in Acute leukaemia is diagnosis Things to look for on blood count: o anaemia +/- MCV (usually normocytic, but anaemia can cause rouleaux = high mcv) o leucocytosis (sometimes leucopenia) o neutropenia & thrombocytopenia things to look for on blood film: o anaemia + aniso- & polikilocytosis o leucocytosis (sometimes leucopenia) o presence of leukaemic cells (blasts, auer rods) o neutropenia +/- dysplastic neutrophils dysplastic neutrophil are more characteristic in myeloid leukaemia dysplastic neutrophils are more diffuse and have ?pseudo-pelvis nuclear shape in MDS the appearance of (white) nucleoli may suggest leukaemia o thrombocytopenia bone marrow aspirate o helps to count percentage of blasts in bone marrow (>20% of nucleated cells = acute leukaemia) o appearance of onky one type of cell (as opposed to all cells in a lineage development) are indicative of clonal expansion and hence acute leukaemia o gains material for cytogenetic analysis 3. The role of cytochemistry in diagnosis of acute leukaemia is dying out because immunophenotyping is more specific There are 4 types of stain used in cytochemistry Myeloperoxidase – stains myeloblasts o only identifies M1/2/3 AML o helps to differentiate M0 & M7 AML from ALL (ALL will not stain +ve) Sudan Black B – same as myeloperoxidase Chloroacetate esterase – stains myeloblasts o useful in variant M3 non-specific esterase – stains monoblasts and megakaryocytes 4. the role of morphology in diagnosis of acute leukaemia (FAB) Morphology lineage notes M0 minimally differentiated need immunophenotyping for CD34, CD33, CD117 to diagnose M1 slightly mature M2 mature smaller cells, more cytoplasm, nucleus a bit more condensed M3 APML DIC following degrnaulation of leukaemics variant M3 has a cleaved nucleus apperance M4 myelomonocytic M5 monocytic/monoblastic M6 erythroid M7 megakaryoblastic need immunophenotyping to diagnose clinical suspicion bone marrow aspirate blood film & count cytochemistry on blood film or aspirate 2.4 – CYTOGENETICS IN HAEMATOLOGICAL NEOPLASMS 1. NOT all cytogenetic abnormalities are causative for leukaemia can show random abnormalities which need to be distinguished from abnormalities that are causative for leukaemia International nomenclature accepts a leukaemic clone to be present when: o 2 cells show the same structural change or additional chromosomes o 3 cells show the same missing chromosome 2. Translocations: Inversions & deletions Reciprocal translocations involve exchange. Non-receiprocal translocations involve one way transfer Balanced translocations involve no change in amount of DNA. unblanaced translocations give a gain/ loss of DNA o International nomenclature lists chromosomes in numerical order. if the chromosome is unbalanced, that which has had DNA inserted into it, is listed first Pericentric inversions involve the centromere o this involves one chromosome and means one chromosome has 2 fusion genes paracentric inversions do not involve the centromere o this involves both chromosomes and means both chromosomes have 1 fusion gene terminal deletions involve loss of the telomere Interstitial deletions keep the telomere but intervening material between the centromere and the telomere is lost 3. Two of the main Cytogenetic techniques are karyoptyping and FISH Karyotyping arrests cells in metaphase and uses a Giemsa/fluoresecent stain to induce a banding pattern on each chromosome so they can be visualised Single probe single colour FISH Types of probes that can be used in FISH – centromeric, arm or ‘whole chromosome’ Single colour FISH labels a DNA sequence on a pair of chromosomes with one colour o hence 3 signals = trisomy o signals of different sizes = translocation o 1 signal = partial deletion/ monosomy – not sensitive to this Double colour FISH Labels targeted sequences of DNA with a particular colour o possible to label centromere one colour and label an arm a different colour. o hence loss of a chromosome gives loss of both signals whereas a partial deletion gives loss of one fusion probes target DNA sequences at breakpoints and hence give a colour change when two targeted sequences come into proximity following translocation breakapart probes target DNA sequences that span across the breakpoint, hence giving a colour loss following a translocation Advantages of FISH can give information about an amplified signal (oncogene) as well as a decreased signal (tumour suppresso gene) can be used with cells in metaphase or interphase – useful for slowly dividing cells (CLL) Whole paint FISH/ multi colour FISH is useful when the translocation is complex Summary: FISH Type of FISH (normal) FISH Definition labels DNA sequences with fluorgenic probe M-FISH (multicolour) labels chromsooems with 5 fluogenic probes similar to M-FISH but cominbations of colours are recognised by spectral signature SKY (spectral karyotyping) Applications detects numerical abnormalities, translocations, presence of fusion genes, amplifications/loss of gene sequences can help to make complex karyotopes a bit clearer 4. PCR can be adopted if karyoptyping is complex/ cytogenetic analysis has failed Type of PCR (normal) PCR definition Amplifies DNA in vitro Applications detection of gene rearrangement and hence leukaemia classification; more senstitive than southern blotting analysis of genes that are too long for standard PCR RT-PCR (reverse transcriptase) Multiplex PCR RQ-PCR (realtime quantitative) uses RT to generate and subsequently amplify cDNA simultaneous identification of a number of mutations fluorogenic probe is broken quantification of DNA = quantification of disease down over course of burden AND monitoring of minimal residual disease reaction 3. WHO classification of AML Therapy-related AML has a worse prognosis which is why it is classified separately. alkylating agents cause worse AML – they are associated with abnormalities in c7, c5, inv(3), t (3;3), (6;9) and (8;16) topoisomerase inhibitors cause balanced translocations and account for ~10% of APML. this is on the up as treatment of other cancers is improving so that survival is long enough to experience an AML. importantly, mutations caused by therapy have a worse prognosis than if the same mutation occurred de novo. The next step in the WHO classification is classifying recurrent genetic abnormalities seen in AML, because they correlate closely to prognosis The important ones are: t(8;21) (q22;q22) [RUNX/RUNX1T1] o good prognosis APML - t(15;17) (q22; q21) [PML/RARA] o variant M3 is very (but not 100%) similar to true M3 on a genetic and clinical basis. it is ‘variant’ because of morphological differences – granules cannot be seen on LM but they can on EM o the diagnosis between classic and variant M3 lies with using a fluorescent Ab against PML, which appears microparticulate in variant M3 o survival rates plummet initially because of DIC o RARA is involved in a number of leukaemias inv (16) (p13.1q22) or t(16;16) (p13;q22) [CBFB/MYH11] o eosinophilia and increased basophil granules o good prognosis Some others are: t(9;11) (p22;q23) [MLLT3/MLL] – bad prognosis t(6;9) (p23;q23) [DEK/NUP214] inv (3) (q21q26.2) or t(3;3) (q21;q26.2) [RPN1/EVI1] t (1;22) (p13;q13) [RBM15-MKL1] NPM1/ CEBPA mutations, these tend to have a good prognosis. There are many subtypes of AML that can not be classified on a genetic basis some of these can be classified morphologically by the FAB system M0-M7 the others can not: o transient myeloproliferative disorder in Downs Syndrome o Acute basophilic leukaemia o acute panmyelosis with myelofibrosis o myeloid sarcoma Summary – roles of cytogenetics in haematological neoplasms 1. Prognostic roles a. Demonstrates monoclonality of leukaemia b. Shows which lineages are involved in the neoplasm c. Provides evidence of mechanisms in leukaemia (over-expressed oncogene/ suppressed tumour suppressor gene) 2. Diagnostic roles a. Provides evidence of aetiology of leukaemia (because certain aetiological agents cause distinctive genetic changes; finding these changes can reveal the cause) b. Very specific at identifying subtypes of AML (eg M3/APML) c. Distinguishes therapy-related and recurrent AML d. Can provide evidence for underlying/predisposing disease to a leukaemia 3. Monitoring roles a. Can provide evidence of regression in response to treatment b. Can provide evidence for engraftment in response to BMT 2.5 – IMMUNOPHENOTYPING IN ACUTE LEUKAEMIA 1. When do we need immunophenotyping? In EVERY case of acute leukaemia that is not obviously myeloid Particularly in M0 & M7 AML o lymphoblasts cannot be distinguished from M0 myelobasts because M0 do not have granules (so myeloperoxidase staining will fail) and do not have auer rods (so morphological tests will fail) 2. Principles of Immunophenotyping the process identifies CSM antigens, and, if the cell can be permeabilised, cytoplasmic and nuclear antigens too Most immunophenotyping is achieved by use of a flow cytometer o forward light scatter can count and size cells in a stream o sideways light scatter can characterize cells based on granularity/ complexity o gating (to increase expression and hence scatter) of a particular antigen can increase specificity in flow cytometric analyses gating fails with some blast cells, particularly monoblasts and M3 AML blasts the principle is using a flurosecent monoclonal antibody against the antigen. o monoclonal antibodies are stable and specific o coexpression of different antigens can be measures if >1 Ab is used o Monoclonal antibodies are expensive and it would not be practical to check for every surface antigen instead, panels of antibodies that are appropriate for subtypes of leukaemia are used to make a diagnosis supplementary panels are used to identify markers that correlate with stages of cell maturation and hence is of prognostic value rarely, antibopdies are labeleed to an enzyme which releases a colour when it catalyses a reaction. enzyme-labelled antibodies require the sample to be on a fixed medium 3. Applications of Immunophenotyping in haematological malignancy differentiation AML from ALL and determining the subtype of AML/ ALL distinguish acute leukaemia from a lymphoproliferative disorder/ other tumour revealing the abnormal phenotype which is useful in monitoring minimal residual disease after remission is achieved identify antigens for therapeutic targets o you rarely need immunophenotyping to diagnose CML because usually blood film/ count/ cytochemistry will give you the diagnosis accurately 4. Common CD markers Diagnostic use Both AML & ALL Common ALL B Cell ALL (strong association) B Non hodgkins lymphoma CD CD34 TdT CD45 CD10 CD19 CD79A CD22 SmIg Distribution of CD HSCs, immature cells ALL blasts and 10-20% of AML blasts express it too Common leucocyte antigen more closely associated with B cell > Tcell B cells & B blasts B cells & B blasts (sometimes T blasts) B cells & in cytoplasms of B blasts Mature B cells T Cell ALL (strong association) CD3 TCR ab TCR gd T Cell ALL (weak association) CD1a CD2 CD4 CD5 CD7 CD8 CD13 CD117 anti-MPO CD33 CD41, 42a/b, 61 antierythroid glycophorin AML AML (M7) AML (M6) T cells, thymoblcytes & in cytoplasms of T blasts Majority of T cells Some T cells and T blasts (strong monoclonal expansion of this TCR is suspicious) 20% T blasts & thymocytes T cells, T blasts, thymocytes & NK cells Thymocytes [with CD8] & CD4 T cells T cells, T blasts & thymocytes T cells, T blasts, thymocytes, NK cells AND 2-15% of AML Thymocytes [with CD4] & CD8 T cells all myeloid blasts most myeloid blasts in cytoplasm of myeloid cells myeloid blasts and some mature myeloid cells platelets, megakaryocytes & blasts Panels used in immunophenotyping: Malignancy B cell T cell myeloid not-lineage restricted Primary panel CD19, 22, 79a, 10 CD3, CD2 Cd13, 117, anti-MPO Tdt supplementary panel SmIg, CD138 CD7 CD33, 41, 42, 61, glycophorin CD45 Supplementary Panel outcomes in B-cell ALL Type of B-ALL Pro-B or early B Common Pre-B Mature B (non Hodgkin lymphoma) Markers CD34+, TDT+, CD10-, SmIgCD34+, TDT+, CD10+ SMIgCD34+, TDT-, mu Ig (cytoplasmic only) CD34-, TDT-, kappa/lamda Ig (cytoplasmic or surface) 3. Minimal Residual Disease MRD can not be detected morphologically and cytogenetic analysis is also too insensitive Immunophenotyping is useful in monitoring minimal residual disease after remission is achieved But PCR is the best method of monitoring MRD Another method is multiparameter flow cytometric immunophenotyping – this uses a number of antibodies simultaneously to try and detect leukaemic characteristics. such characteristics include: o aberrant antigen expression loss/weak expression of a (tumour suppressor) antigen over expression of a (oncogenic) antigen simultaneous expression of markers of immature cells (CD34, tdt) 2.6 – MANAGEMENT OF CML 1. Recap of the CML disease process Without Treatment, CML patients undergo the following process: 5-6years in the chronic phase (anaemia, B symptoms, early satiety and abdominal discomfort because of splenomegaly) ~1year in the accelerated phase 3-6months in a blastic crisis – followed by death 2. The genetic pathophysiology of CML is the key to treatment design 22q- is the Philadelphia chromosome This is because BCR is upstream of ABL in 22 whereas it is downstream of ABL in 9q+ The breakpoint in 9 is anywhere before the 2nd exon of ABL The breakpoint on 33 is at either exon 13 or 14 of BCR o Hence the breakpoint region in 9 is much larger than in 22 The role of BCR/ABL Normally, a tyrosine kinase domain on ABL, called SH1, keeps it regulated BCR ‘unlocks’ and hence activates SH1, and thus ABL o Since BCR is a housekeeping gene, it is always on and unregulated. o Hence the fusion gene leads to constitutive activation of SH1 The active BCR-ABL gene product uses ATP to phosphorylate side chains on tyrosine residues o Cytoskeletal protein phosphorlyation = increased cell migrations and decreased adherence to BM matrix o Nuclear protein phosphorylation = induction of c-myc = proliferation o Mitochondrial protein phosphorylation = escape from apaoptosis RT-PCR in disease monitoring Because the breakpoint region in 9 is large – traditional PCR cannot detect the gene sequences involved at the BCR/ABL border following translocation o Hence, RT-PCR has to be used to replicate the mRNA transcript and analyse cDNA At diagnosis, you usually have 10e13 leukaemic cells. PCR is only sensitive to the point that where it doesn’t pick up anymore BCR/ABL transcript, you probably have less than 10e7 leukaemic cells o It is thought that the host immune system can manage this leukaemic burden 3. Imatinib and other monoclonal antibodies can ‘cure’ CML Imatinib is a tyrosine kinase inhibitor The mechanism of action is that the drug mimics ATP so BCR-ABL uptakes it instead of ATP, and thus cannot start phosphorylation cascades 1/3 of patients fail to responf to Imatinib. The reasons for this are: o Lack of compliance o Drug interactions and CYP3A4 polymorphisms giving reduced drug titre in plasma o Plasma binding (AGP) to give reduced drug titre o Resistance 15 mutations account for 90% of cases of resistance to Imatinib o One of these is a point mutation in BCR/ABL [t315i] which means Imatinib can not bind the gene product Newer agents dasatanib and nilotinib give a response in 40% of resistant patients o Subsequently, they have been show to be more powerful and have a decreased risk of developing blastic crises compared to imatinib, when given to patients in the chronic phase With treatment, about 85-90% of CML patients now have a normal life expectancy The main issue is that Imatinib costs about £500million/yr; newer agents are about 1/3 more expensive Measuring the response to Imatinib [clinical endpoints from the IRIS study] Haematological response o WCC <10e9 o Plt <450 x10e9 o <5% myelo- & metamyelocytes o No blasts, promyelocytes, no extramedullar haemopoeisis Cytogenetic response in marrow cells o No Philadelphia chromosome in metaphase arrested cells Molecular response o PCR to measure ‘log reduction’ of ratio of BCR/ABL:BCR transcripts 2.7 – ACUTE LYMPHOBLASTIC LEUKAEMIA (ALL) 1. Clinical features of ALL D - haematological neoplasm characterized by clonal expansion of lymphoblasts in BM and PB. I - commonest childhood malignancy; 35% of all childhood cancers A - peak incidence 2-5 years S - M>F G - White > Black A - Unknown P - [see classification] C - s.s.e Bone marrow failure = anaemia, neutropenia (chest infections in kids), thrombocytopenia Organ infiltration = tender bones (limping children) organomegaly and lymphadenopathy meningeal syndrome (rare) o confusion, hemiplegia testicular swelling in boys, mediastinal compression in T-ALL P cure rate in children ~90%; worse in adults (~50%) 5 year disease free survival is now about 90% in kids who get ALL aged 2-5 2. Differential diagnosis of ALL AML Aplastic anaemia, neuroblastoma, rhabdomyosarcoma Infectious disease o Pertussis – look for ‘clefted lymphocyte’ on morphology – more indicative of reactive lymphocytosis o EBV – look for scalloping (cupping) of RBCs by lymphctic cytoplasm Diagnosis of ALL depends on immunophenotyping Tdt is the most important antigen – present on lymphoblasts and lost on mature cells B/T markers can subsequently diagnose the sub-type o 75% of adult ALL is B-ALL o 85% of childhood ALL is B-ALL 3. Classification of ALL The old FAB classification was based on morphology L1 – uniform, small blast cells L2 – large blast cells with prominent nucleoli and more cytoplasm L3 – blasts with perinuclear and cytoplasmic vacuoles o L3 is now known as Burkitt’s lymphoma (which is associated with HIV) Blasts – increased nuclear: cytoplasmic ratio Agranular cytoplasm Visible nucleoli Large cells The new classification given by WHO is based on cytogenetic & molecular subtypes of ALL ALL o B- cell Good prognosis T(12;21) (p12,q22) [TEL/AML1] – this is the commonest genetic abnormality in B-ALL T(1;19) (q23;p13) [PBX/E2A] Hyperdiploidy – trisomy 4,10,17 have decent prognoses Bad prognosis T(9;22)(q34;q11) [BCR/ABL] T(11q23) [MLL] – AL diagnosed in babies <1yr old usually have this hypodiploidy o T-cell Burkitt’s lymphoma Biphenotypic acute leukaemia ALL not otherwise classified o Aplastic variant of ALL o Down syndrome ALL o Secondary ALL 4. Pathways affected by mutations in B-ALL Block in B-cell maturation o PAX5 is common mutation; IKZF1 and EBF1 mutations are others Downregulation of tumour suppressor genes = dysregulated cell cycle Abnormal lymphoid signaling Activation of transcription factors Modification of epigenomes and histone proteins 5. Prognostic factors in ALL At diagnosis o Age – unless <1yr old (MLL) having ALL young is better prognostically then getting it old o WCC – higher WCC = worse prognosis (T-ALL tends to present with high WCC than B) o Cytogenetics [see above] o Immunophenotype – not of importance in prognosis of B-ALL. T-ALL which is CD1a+ has a favourable prognosis At Induction of treatment o Remission/MRD = <5% blasts o To avoid relapse, you aim for no blasts/100k cells o MRD+ve = worse prognosis Long-term effects of ALL Chemotherapy related – infertility Radiotherapy related o Skin cancer (SCC/BCC) o Meningioma o endocrinopathies 6. Management of ALL depends on chemotherapy Step 1- Induction Phase – 2x28days o Aim is to induce remission o Common drugs are vincristine, dexamethasone, daunorubicin, asparaginase Asparaginase can cause thrombosis/bleeding, pancreatitis, hepatoxicity Step 2 – intensification o Aim is to offer prohylaxis against CNS malignancy o Methotrexate and radiotherapy Step 3 – either HSC transplant in bad prognosis groups or consolidation in good prognosis groups o Indication of transplant include MLL, Ph+, MRD+/relapsing disease o Stem cells can be obtained from sibling, Anthony Nolan register or unbilical cord transplant Step 4 –(post consolidation) – maintenance phase; can take years o Methotrexate and mercaptopurine Supportive measures in management Hickman line (central venous access) Blood/platelet transfusions and antibiotics to prevent infections Antiemetics Allopurinol to prevent tumour lysis syndrome Ph+ ALL needs Imatinib New options in management – the BITE trial used anti-CD19 in B-ALL; it stimulates host T cells to kill B-blasts; great! 2.8 – ONCOGENES AND TUMOUR SUPPRESSOR GENES IN ACUTE LEUKAEMIA; M2 & M3 AML 1. It is thought that most cases of leukaemia are caused by the 2 hit hypothesis of genetic mutation Acute leukaemias are clonal expansions of abnormal cells, commonly as a result of a somatic mutation in a proto-oncogene, resulting in oncogenesis o Mutations in oncogenes often affect transcription factors Mutations in acute leukaemia often demonstrate the dominant negative effect o The mutant inhibits the gene-product of the normally functioning allele, as well as making a dysfunctional gene product itself One mutation is rarely enough – you need one affecting survival and one affecting differentiation ALL follows the 2 hit hypothesis o You get one mutation in utero (eg t12;21) o Another mutation after birth triggers ALL 2. The nature of mutations in oncogenesis (5) Point mutations Interstitial deletions, bringing proto-oncogenes into contact with the wrong gene promoters Internal tandem duplication (MLL, FLT3) Amplification of an oncogene (rare) Translocations, which, again, bring a proto-oncogene into contact with a wrong promoter Insertional oncogenesis occurs after gene therapy, where the gene is inserted into the wrong place Inherited genetic abnormalities in oncogenesis can be the first hit Haploinsufficiency (loss of 1 allele) of a gene that is critical for normal differentiation o Eg loss of 1 copy of RUNX1 in familial thrombocytopenia can predispose to AML Loss of function of tumour suppressor genes o Neuroblastomas (NF1), retinoblastomas (RB1) Chromosomal fragility syndromes increase likelihood of somatic mutations occurring o Fanconi anaemia Abnormalities of genes that repair DNA mean that random errors are not corrected Abnormalities of genes that degrade mutagens can lead to environmental mutagenesis 3. Abnormalities in tumour suppressor genes can cause a variety of leukaemias Whole/partial chromosome deletion as well as small mutations can affect normal tumour suppressor function Tumour suppressor loss can contribute to: o Familial leukaemias o Therapy-related leukaemia o AML in elderly o Transformation of chronic leukaemia to an acute/blastic phase 4. The genetic basis of M3 AML; APML Normal action of RARa and RA RARa uses Zinc to bind to the retinoid X receptor [RXR]; this dimer can bind to retinoic acid response elements [RARE] on target genes This complex recruits NCoR/HDAC and Sin3; this is a repressor complex. It also interacts with another repressor; SMRT o Hence normally, RARa supresses transcription – tumour suppressor gene In the presence of physiological levels of retinoic acid: o the repressor complex cannot assemble o RARa binds to transcriptional coactivators eg CBP o Histone acetylase is recruited; forming an activator complex Hence, normally, retinoic acid activates transcription – proto-oncogene Normal functions of PML [tumour suppressor] PML has 2 isoforms: Normal nuclear PML makes the outer shell of nuclear bodies (NBs) o NBs contain other proteins eg pRb, p53 and BLM hence normally functioning NBs play key roles in apoptosis, senescence, growth suppression and genome stability Cytoplasmic isoform enhances TGFb – this also achieves tumour suppressor activity Overall actions of PML-RARa fusion gene Since all patients express PML-RARa but only 70% express the reciprocal (?relevance), the former is likely to be the causative fusion gene Resistance to retinoic acid = decreased transcription = block in differentiation at the promyelocyte stage Continued proliferation Failure of apoptosis Mechanism of PML-RARa; suppression of transcription leads to block of differentation Oncogenic - Dominant negative inhibition of the normal PML allele [both isoforms] and the normal RARa allele o Abnormal PML = microparticualte distribution of proteins usually encased within Nbs o Cytoplasmic isoform is sequestered = decreased TGFb Suppressive - PML-RARa dimerizes with RXR and binds to RARE as normal, BUT oligomerization leads to binding of nuclear PML o Nuclear PML and RXR are subsequently sequestered o The resulting complex binds the repressor complex more strongly o The resulting complex has resistance to retinoic acid Suppressive – PML-RARa can bind to RARE without the need for RXR – this has a stronger repressive activity as there are more binding sites for repressor complex proteins Suppressive – PML-RARa recruits DNA methyltransferase; methylation of DNA leads to decreased transcription 5. The genetic basis of variant APML Not all acute leukaemias involving the RARa gene also involve PML. These variants may or may not respond to ATRA/Arsenic trioxide – and knowing the molecular basis of disease helps us to make new therapies. Some examples are: T(11;17)(q23;q21) PLZF/RARa o ATRA can not disrupt binding of some repressor molecules to PLZF; adding HDACi may help T(11;17)(q13;q21) NUMA1/RARa T(5;17)(q35;q21) NPM1/RARa T(5;17)(q25;q21) NPM1/RARa o All of these variants have oligomerizaton domains, meaning they can bind to repressor complexes more strongly. They also all display the dominant negative effect. 6. The molecular basis of the management of classic APML (and some variants) Actions of ATRA Induces terminal differentiation Facilitates apoptosis of neutrophils Leads to loss of leukaemic clone and replacement by normal cells Mechanisms of ATRA Degrades PML-RARa o Caspase mediated cleavage The degradation releases RXR to bind with normal RARa The degradation also redistributes nuclear PML back into nuclear bodies The net result is return to normal transcription ATRA doesn’t cure, you will get relapse. Arsenic trioxide and HDAC inhibitors (which interferes with the repressor complex), in synergy with ATRA, may cure APML without the need for chemotherapy. Actions of Arsenic trioxide: Degrades PML-RARa without degrading RARa – this induces partial differentiation which may be the key o It Activates caspases and induces apoptosis Nuclear bodies are reformed Unlike ATRA, it also effects leukaemia-initiating cells. These cells are quiescent but have the potential to cause relapse; this is why arsenic trioxide has lower relapse rates in APML. 7. The genetic basis of M2 AML Normal RUNX1 function Usually encodes a transcription factor CBFa in myeloid cells o CBFa usually activates p14ARF CBFa binds to CBFb via its ‘runt’ domain; this complex allows another protion of the runt domain to bind DNA o In the complex, CBFb protects CBFa from ubiquitization After binding to DNA, CBFb recruits histone-acetyl-transferase – this leads to transcription of many genes including G-CSF, GM-CSF, M-CSF, CD13, IL3, IL5 and MPO o CBFb also leads to repressed transcription of other genes by interacting with TLE Normal RUNX1T1 is a tumour repressor that is usually expressed in the brain Actions of the RUNX1/RUNX1T1 fusion gene Dominant negative inhibition of normal RUNX1 o Hence p14ARF is suppressed The fusion product binds CBFb with greater affinity so DNA binding is enhanced Similar to PML-RARa, there is oligomerization of domains in the RUNX1t1 protion of the gene product o Oligomerization leads to binding of the repressor complex (NCoR, HDAC, Sin3) o Repression of DNA repair genes increases likelihood of further mutation The fusion gene also inhibits PLZF; which leads to excessive proliferation of myeloid cells Its inhibits the TGFb pathway and this also leads to proliferation T(16;21)(q24;q22) involves a different translocation (CBFA2T3 instead of RUNX1T1) but mechanism of action is similar because oligomerization domains are similar 8. Other mutations in RUNX1 (apart from translocations) can also give AML Familial thrombocytopenia predisposes to AML A mutation in the runt domain leads to failure of recruitment of histone-acetyl-transferase This leads to the inability to activate transcription(haplo-insufficiency of the mutated allele) – which is necessary but not sufficient (other mutations needed) for the development of AML Sometimes, this mutation also displays a dominant negative effect A similar mutation is seen in acquired cases of M0 AML and MDS 9. The genetic basis of M4 AML Action of CBFb/MYH11 fusion gene MYH11 forms multimers and this leads to sequestration of RUNX1/CBFa from the CBFa/CBFb complex MYH11 recruits co-repressors o Hence, all leukaemias involving CBF genes tend to involve oligomerization of the fusion product leading to sequestration of CBFa/RUNx1 10. Genetic basis of AML without evident translocations This still tends to follow a two hit hypothesis First hit: o NPM1 mutations are common in adults o CEBPA mutations are implicated in familial leukaemias Second hit: o FLT3 (ITD) mutation o Others Key summary points for M2/M3 leukaemias: Both involve excessive transcriptional repression due to oligomerization Both involve fusion genes with dominant negative effects To reverse the leukaemic phenotype, you need to: o Inhibit HDAC o Recruit HAT o Recruit transcriptional activators 2.9 - MYELODYSPLASTIC SYNDROMES (MDS) 1. Clinical features of MDS D - A group of clonal haematopoetic stem cell diseases characterised by abnormalities in one or more myelod cell lines and manifested by: Cytopenia - particularly manifesting as anaemia The cycle between hyperactive, ineffective haemopoeiss which aims to compensate for abnormal cells, but fails to because all the BM can make is more abnormal cells Increased risk of transforming into AML I - 3-5/100k A - elderly; median 70years S - M>F G A - UNKNOWN - environemtnal exposure to benzene, cigarette smoking may be relevant Secondary to Prior chemo/radiotherapy accounts for 15% of cases o Cyclophosphamide (used in breast and prostate ca) o Cisplatin (used in breast, testicular and ovarian ca) In the differential diagnosis, you must rule out other causes of acquired dysplasis eg infectious (EBV), drugs (azathioprine, cyclosporine) and B12 deficiency P C - [see classification] - s/s/e Cytopenia - anaemia [commonest finding], neutropenia, thrombocytopenia Management C - supportive treatment (transfusions, antibiotics). Especially for people who are old and have comorbities M - EPO may help with anaemia; lenalidomide improves cytopenia [watch major SFX is VTE]. Danozol can help in those with severe thrombocytopenia and pyrimidine analogues (azacytidine, decitabine) can be used in people with evident chromosomal abnormalites S - BMT for young patients only P - The international prognostic scoring system is adopted [see below]. Age and underlying disease also affects prognosis Score % BM blasts Karyotype Cytopenia 0 <5% good 0.1 0.5 5-10% intermediate 2-3 Characteristics of cytopenia: Neutrophils <1.8e9; 1 1.5 11-19% Poor plt <100e9; Low risk = 0 = good prognosis o Morphology - RARS o Cytogenetics - normal, del 5q, del20q, del Y Intermediate risk = 0.5-2 o Morphology = RAEB1, RCMD o Cytogenetics - all that do not fall into good/bad risk High risk = >2 = poor prognosis o Morphology - RAEB2 o Cytogenetics - monsomy 7/ del7q, complex karyotypes Hb<10g/dl 2 >20% (AML) 2. WHO classification of MDS Disease Refractory unilineage cytopenia (anaemia/neutropenia or thrombocytopenia) Refractory anaemia with RS (RARS) Refractory cytopenia with multilineage dysplasia (RCMD) PB No blasts Refractory anaemia with excess of blasts-1 (RAEB1) Refractory anaemia with excess of blasts-2 (RAEB2) MDS associated with del (5q) [5q syndrome] Unclassified MDS <5% blasts, no auer rods No blasts No blasts 5-19% blasts with auer rods <5% blasts, macrocytosis No blasts BM unilineage dysplasia <5% blasts <15% Ring sideroblasts (RS) <5% blasts >15% RS Dysplasia >10% in two or more lineages <5% blasts Uni/mulit-lineage dysplasia 5-9% blasts, no auer rods Uni/multi-lineage dysplasia 10-19% blasts with auer rods Hypolobulated megakaryocytes <5% blasts, no auer rods Dysplasia; 5% blasts 3. Morphological appearances of dysplastic lineages Granulocyte lineage: o Hypolobualted nuclei (pseudo-pelger/dumbbell shaped nuclei) o Hypo/agranular blue cytoplasms o >1 nucleus per cell o Auer rods may or may not be present in MDS Erythroid lineage: o Cytoplasm Poor Hb, vacuole appearances Heavy perinuuclear siderotic granules (ring sideroblasts) Cytoplasmic bridge formation PAS positivity o Nuclear Incomplete division, budding, fragmentation >1 nucleus per cell with Internuclear bridges o Megakaryoblast lineage: Smaller cells with hypolobulated nuclei [normal megakaryocyte nucleus looks like a bunch of grapes] >1 nucleys per cell 4. Cytogenetic changes in MDS Only 50% of MDS have a cytogenetic abnormality evident. Cytogenetic changes are more common in t-MDS The majority of t-MDS are monosomies of 5/7 or deletions of 5q/7q o Two other translocations found in t-MDS are balanced - t (11;16) and t(3;21) Some other cytogenetic changes in de novo MDS are: o Unbalanced translocations - trisomy 8, monsomy 5/7, del 20q, del y, abnormal 17 Del 5q (5q syndrome) is more common in women and presents with a good prognosis; it has a low AML transformation rate can some patients respond to lanalidomide 5. Clinical features of mixed MDS/MPD D - Clonal haematopoetic neoplasms that at the time of presentation, have findings that support both MDS and MPD including: Hypercellular BM with <20% blasts Proliferation in one cell lineage and dysplasia (without proliferation) in another Hepatosplenomegaly is common I/A - 3/100k >age 60; develops in 5% of people with MDS 6. Sub- Classification of MDS/MPD Chronic myelomonocytic leukaemia (CMML) o This is a persistent monocytosis in the absence of other causes including infection, BCR/ABL, PDGFRA rearrangement o Presents with B symptoms, splenomegaly and infiltrates into other organs/skin o Median survival is <3years and 15-30% progress to AML o CMML1 has <5% PB blasts and <10% BM blasts o CMML2 has 5-19% PB blasts and 10-19% BM blasts o Cytogenetic abnormalities only seen in 20-40% of cases; about 40% have a RAS mutation; n-ras mutations are relatively frequent in MDS/MPD Atypical CML (BCR-ABL negative) o Presents very similarly to CML but fusion gene is absent on PCR and/or Px is not responding to imatinib o Multilineage dysplasia is what differentiates it from CML o Cytogenetic abnormalities are seen in 80% of cases o Upto 40% progress to AML Juvenile myelomonocytic leukaemia (JMML) o Diagnosis includes high HbF, hypersensitive to Gm-CSF in vitro o Usually present in boys younger than 14 with thrombocytopenia and neutropenia, hepatosplenomegaly is almost always there o Associated with neurofibromatosis and monosomy 7 is seen in 40% of cases Unclassifiable MDS/MPD ?RARS with thrombocytosis 2.10 - CASE PRESENTATION/TUTORIAL - MDS/AML/BMT TRANSPLANTS MDS/AML Key points in the history of someone presenting with ‘B symptoms’ o Things that could mean it is not a haematological disease - recent drugs, quick onset, alcohol/IVDU o Thigns that could mean it is a haematological disease - Hx of cancer and chemo/radio, HIV (causes MDS) Key points in investigations: o Hb on ABG is not reliable o 1 set of abnormal results always need to be redone o Blasts & dysplastic cells in the BM occur in MDS and AML Girls given chemo are probably going to be infertile, boys should be sperm-banked 50% AML patients relapse after induction chemo Autologous BMT transplants The principle with autologoug transplants is to wipe out the clone (or monoclonal antibody in AI disease) with high dose chemotyherapy and then re-itnroduce the normal host stem cells Uses in malignancy: o Haem - Lymphoma, myeloma, some ALL o Solid - Testicular, placental, ovarian o Other - neuroblastoma Uses in AI disease - MS/ RA/ scleroderma Allogenic BMT transplants Sibling/ matched allogenic - of use in all tumours? Unrelated/ unmatched allogenic o Can be used in AML/ ALL Problems with BMT transplantation Infection o High dose chemo knocks out fast dividing cells - including gut cells Gut is full of G-ve bacteria that can then enter bloodstream to cause sepsis BAD o Hickman lines are often needed to deliver chemo - source of infection o Immunosuppresion leads to susceptibility to all sorts of oppurtunisitics including: CMV - retinitis, pneumonitis, gastroenteritis Aspergillus in the lungs Hepatic/ renal failure o Both of these are sensitive to damage by chemotherapy. o The kidney is sensitive to antiviral drugs that are used to treat CMV GVHD o Usually occurs 2 weeks after chemotherapy; lymphocytes are the 1st cell lineage to recover o ‘foreign’ lymphocytes proceed to attack, in particular, the skin, gut and liver. But they also attack the leukaemic clone o Steroids need to be given to supress the response - the problem here is reintroduction of infection and relapse of leukaemia Transplant mortality is roughly 15%. You need to nurse patients through the 2 week barrier and hope for a sub-clinical level of GVHD. 2.11 - CHRONIC LYMPHOCYTIC LEUKAEMIA (CLL) 1. Clinical Features of CLL D - proliferation of mature (B) lymphocytes I - accounts for ~20% of all haematological malignancies; incidence 3/100k A - increase incidence with age; median age between 65-70years S - male>female 2:1 G - Commonest leukaemia in western world (20x more than eastern) A - Unknown; deletions of microRNA may have a role P - [See below] C - s/s/e disease course is very variable. It tends to be a slow, indolent progression of mature B cells; the time from diagnosis by which symptoms of BM overcrowding is seen is variable 70% diagnosed incidentally o Family hx (you can find monoclonal B cells in relatives of CLL patients) o comorbididites o Infections (bacterial/ fungal) o anaemia o Peripheral lymphadenopathy - syymetrical enlargement of superficial odes o Hepatosplenomegaly Progressive phase/other symptoms relating to management AI diseases in CLL o Haem - AIHA, AI thrombocytopenia, neutropenia, pure red cell aplasia AIHA is stimulated by treatment (chlorambucil) o Non-haem - nephrotic syndrome, angio-oedema, paraneoplastic pemphigus Progression o Richter syndrome - transformation toa high grade lymphoma that effects 3% of patients, associated with fludarabine usage Investigations Blood count/film o Count - Lymphocytosis between 5-300e9, Normochromic anaemia, thrombocytopenia o Film - Smear cells (artefact cause by spreading blood on film) Immunophenotyping o The main thing with mature CLL B cells is that they express CD5, which is usually exclusively espressed on T cells - normal mature B cells do not express it The CLL score gives 1 point to CD5+. CD23+, FMC7- and weak expression of Cd22 and SmIg. A score of 5/5 = CLL likely Other tests include antigolubulin test (coombs test), reticulocyte count, serum Ig, bone marrow aspirate/ LN biopsy o Serum Ig - redyuced concentrations/ immuneparesis o BM aspirate - lymphocytic replacement of normal cells Differential diagnosis Mantle cell lymphoma - non hodkins lymphoma associated with t(11;14) (q13;q32) where cyclin D1 is overexpressed - very aggressive cancer. o Cannot differentiate on immunophenotyping because they also co-express CD5 2. Prognostic factors in CLL Clinical Stage Binet Staging score: Stage A B C Stage 0 1 2 3 4 Rai staging score: Prognosis Good Intermediate bad Features <3 lymphoproliferative areas >3 lymphoproliferative areas B + Hb<10g/dl + Plt < 100e9 Features Lymphocytosis lymphadenopathy Hepatosplenomegaly +/- [stage1] 2+ Hb <11g/dl 2+ Plt <100e9 Prevalence (%) 60 30 10 Prevalence (%) 30 25 25 10 10 CD38/ZAP70 Lower ZAP70 expression is a good prognosis Ig gene mutation status CLL with Mutated Ig heavy chain genes has a better survival than non-mutated. The principle behind this is that Ig somatic hyper-mutation is a normal process by which Ig’s transform to bind antigens better. Lack of mutation = worsenes B cell function Cytogenetics - Karyotpyping is impossible in CLL because cells are too slow diving - you need FISH Good prognosis - normal karyotype, del(13q), trisomy 12 Worse prognosis - del 11q, del 17p o Del 17p confers p53 loss on one allele and mutation of the other = genomic instability, accumulation of mutations and clonal expansion/ resistance to chemo (p53 usually coordinates responses to DNA damage) Anti CD52 is first line treatment for del (17p) CLL - watch out for reduced t cell response, increased risk of fever and CMV infections o Del 11q gives an ATM mutation which also leads to p53 dysfunction o P53 deletions have a very bad prognosis 3. Management of CLL Watch and wait for all patients until they show an indication for intervention: o Progressive BM failure o Massive/progressive lymphadenopathy o Progressive lymphocytosis defined as 50% increase of 2months and/or a doubling time less than 6 months o >10% weight loss in 6months, fever >38 for >2weeks, fatigue, night sweats o Autoimmune cytopenias If an intervention is indicated - the following treatment strategies are adopted: o First line treatments - steroids, alkylating agent, purine analogues, anti CD20 o Second line - purine analogues, anthracyclines, allogeneic BMT o Treatment of patients who are refractory - high dose steroids, anti-CD52 Young patients may be cured by allogeneic SCT Supportive management for people who would not benefit from intensive chemo 2.12 Prophylaxis/treatment of infections (infections account for 50% CLL deaths) 2.12- MANAGEMENT OF AML New points Early infections in AMl are largely from commensal bacteria - watch for G-ve sepsis AML has decreased associated with lymphadenopathy but increased association with leukostasis as compared to lymphoid leukaemias. Choice of treatment is influenced by o Type of aml o Age o Curative versus palliative treatment Pricniples of treatment o Induction of remission 1 cycle of Combination chemo with cytarabine and daunorubicin 60-80% achieve remission after induction therapy o Consolidation 3 cycles of the same Chemo Autologous/allogeneic SCT o At all times - supportive care, psychosocial support Well established prognostic factors in AML: o Patient performance (can they handle chemo? Did they achieve induction-remission?) o Age o Primary/secondary AML o Cytogenetic features Recap of old points: Clonal proliferation of precursor cells AND maturation arrest Biphenotypic leukaemias (HSC mutations) are treates as AML Commonest leukaemia in adults, median age 63 Main differentials are MPN/MDS and aplastic anaemia De novo AML occurs due to risk factors eg o Genetic disorders (downs, NFM, kilnefelters, fanconi anaemia) o Mutagen exposure (benzene, cigarettes) Secondary AML occurs because of o Progression of previous MDS/MPN o Previous chemo/radiation therapy Symtoms occur due to marrow failure (anaemia, neutropenia, thrombocytopenia) and tissue infiltration (hepatospleno- & lymphadenopathy, gum infiltration[m4/5], granulocytic sarcoma in skin, bone pain) Can usualy diagnose with cirscropy (>20% in BM, auer rods), cytochemsitry, cytogenetics and immunophenotypic is needed for M0/M7 subtypes 2.13- CONSTITUTIONAL SYNDROMES PREDISPOSING TO ACUTE LEUKAEMIA 1. Pathways in leukaemogenesis Common oncogenesis involves changes in gene expression implicated in networks/ circuits including o Cellular motility circuits o Proliferation o Differentiation o Viability In leukamogenesis there are 3 main groups of chnges in gene expression o Upregulated oncogenes = excessive proliferation o Down regulated tumour suppressor genes = evasion of apoptosis o Aberrant DNA repair = defective differentiation; oncogene stimulation and tumour repressor gene inhibition 2. Genetic defects predisposing to leukaemia Tumour suppressor genes o Li fraumeni syndrome (p53) o Neurofibromatosis (NF1) DNA repair genes o Fanconi anaemia o Ataxia-telangiectasia syndrome (ATM) o Also bloom syndrome and Nijmegen breakage syndrome Ribosomopathies o Blackfan-diamond anaemia (rps19/24) o Schwachmann-diamond syndrome (Sdo1) o Dyskeratosis congentia (cbf5) In utero mutations o TEL-RUNX1 Aneuploidy o Down syndrome 3. Fanconi Anaemia is a bone marrow failure syndrome associated with defective recombinational DNA repair Normally there are three main pathways in response to DNA damage: o Repair Single strand breaks fixed by base excision repair Adducts fixed by nucleotide excision repair Double strand breaks fixed by recombinational repair or end-joining Mistahces/inertions/deletions fixed by mismatch repair o Transcriptional respsonse o Apoptosis Fanconi anaemia is an AR disease associated with congenital malformations and progressive BM failure with propensity to suffer malignancy, leukaemia and MDS o FANCA is the commonest of 13 associated mutations o Underlying mechanism is defective homologous recombination DNA repair and hence increased sensitivity to DNA damage by cross linking agents o Most patients present with sympttoms of pancytopenia at 7years of age o 50% develop MDs/AML by age 40 4. Ribosomopathies Blakcfan diamond anaemia is associated with increased activity of RBC adenosine deaminase (ADA) giving red cell aplasia in early infancy (sometimes aplastic anaemia), growth failure with an increased risk of developing AML and osteosarcomas o Pathogenesis is defective ribosome 40S synthesis which is toxic to RBCs o The undlerying mutation commonly involves ribosomal proteins (rps) 19 & 24 and there seems to be a block in differentiation of red cells o ?treat with steroids o Some patients spontaneously enter remission Schwachman diamond syndrome is an AD disease with SBDS mutations presenting with: o BM failure (neutropenia is common) o Exocrine pancreatic insufficiency (improves with age) o Increased risk od developing aplastic anaemia, MDs, AML o Proposed mehcnaism is decreased levels of mature 80S ribosomes [defective binding of 40S/60S subunits] 5. Dyskeratosis congenital is a mixed ribosomopathy/ Telomeropathy Normally, telomeres have repeated TTAGGG sequences which stabilize the chromosome by preventing loss of genetic information and end-to-end fusions. Repeats are lost with each cell divison The telomerase complex replaces thje repeats. It is comprised of Dyskerin, TERC, shelterin, TERT, NOP10, NHP2, GAR1 and probably more proteins o The telomerase complex is also involved in pseudouridylation of rRNA - which is necessary for normal ribosome synthesis Dyskeratosis congentia commonly presents with a mucocutaneous triad (skin pigmentation, nail dystrophy, mucosal leukoplakia) and bone marrow failure o DC is due to mutations in any of the proteins in the telomerase complex - commonly Dyskerin which is inherited in an X-linked fashion. This leads to a mixed ribosome and telomerase-related disease o DC demonstrates the idea of anticipation in genetics - this is the idea that a disease has a worse phenotype and earlier onset in successive geenrations. DC correlates because telomere length seems to shorten with generations. 6. In utero mutations T12;21 in childhood B-ALL has a TEL-RUNX1 fusion gene that forms in utero in 1% of sufferers o There is hyperdiploidy and production of a pre-leukaemic clone, which is selected for following ?an infection after birth to produce ALL 2.14- STEM CELL TRANSPLANTATION 1. Introduction to transplants Autologous transplants Give GCSF 5-16microg/kg every day for 4days; 3 hours in total 4 days later, Collect HSCs (CD34+ve) from PB & freeze Thaw HSCs and reinfuse back into host after high dose chemo Allogeneic transplants Give cancer sufferer high dose chemo +/- radio Transplant BM cells from a different donor Donor stem cells can be obtained from BM/ PB or umbilical cord o BM - procedure is done under GA and involves taking a lot of BM samples (can only take 5ml at a time and you need about a litre) o PB - like autologous, needs GCSF prior to HSC extraction o Umbilical cord - can only get a little sample - not useful for adults because you need roughly 2mill CD34+ cells/kg body weight Donor is ideally matched for HLA-type aka sibling/identical twin o Increasing the specificity requirement of matching decreases the chance that a donor will be available Mortality rate is upto 50% and it costs roughly £150k per transplant done 2. Indications for transplant Autologous transplants Indicated for any patient where there is no allogeneic match and if the patient is too old to survive (aggressive) allogeneic therapy Useful in the management of diseases that are not based in the bone marrow o Mianly for acute leukaemias, lymphomas and solid tumours o Can also be used for myeloma and CLL Allogeneic transplants All leukaemia, myeloma, other causes of Bm failure and congenital immune deficiencies Can also be used for lymphoma 3. Outcomes/ complications or transplants Standard parameters Overall survival Disease-free survival Transplant related mortality Relapse incidence Factors that affect transplant outcome in allogeneic transplants Factor Age Disease phase Genders of receipient/donor Time from diagnosis to BMT Donor matching 0 <20 Early <1yr sibling 1 20-40 Intermediate Female male* >1yr unmatched 2 >40 late *female to male is a worse outcome because of ?lack of Y chromosome; outcome is even worse if she is pregnant with a male child and has formed antibodies against him? Higher score = worse prognosis Complications of BMT Graft failure o Prevented by suppressing the host immune response with chemotherapy o Host-versus graft disease may manifest as an engraftment syndrome WCC, neutrophils and platelets all go up Infections o Post-transplant (chemo) pancytopenia can last for upto 1 month o Contributing factors to infection are neutropenia, loss of barrier function, suppressed cellular and antibody-mediate immunity o In the first few weeks of allogeneic BMT you are aplastic - bacterial infections because of loss of innate immunity Weeks 3 - 6 months you are at risk for GVHD - viral and fungal infections because of impaired adaptive immunity Beyond 6 months is the late phase - latent infections? o Aspergillosis occurs in 6% of BMTs and has a mortality rate of 92% o CMV is also a common problem This is primarily because at any given time, 20% of a person’s T-cell reserve is dedicated to controlling CMV - when you are T-cell depleted, shit hits the fan Risk factors for CMV = negative patients/donors serological stuaus, type of donor, type of transplant and total viral load Graft versus host disease o The cut off between acute and chronic forms is 100days. Chornic GvHD presents like scleroderma o Donors T cells and receipient t cells attack each other You can prevent this by depleting the donor T cells using monoclonal antibodies - but this leads to relapse This suggests that donor T cells are playing a key role in attacking the host leukaemic cells Hence in relapse, you can reinfuse donor t cells to control it o Donor t cells attack host skin, liver, bowel o Treated with steroid and cyclosporine amongst other drugs o Prophylaxis regimens include steroids, cyclosporine and methotrexate Relapse of original disease 2.15- DESIGNED DRUGS 1. The ideal drug target in leukaemia is… Crucial to the malignant phenotype and definably correlated with clinical outcome Not expressed significantly in vital organs or tissues Reproducibly measured in readily available clinical samples When interrupted, interfered with, or inhibited a clinical response is yielded in a significant proportion of patients For antibodies: once bound to the surface the antibody is internalised or endocytosed Minimal response in patients whose tumours do not express the target 2. There are 4 categories of drug targets in leukaemia 1. CSM markers/ receptors and secreted proteins a. Normally a reaction usually leads to dimerization & signal transuction b. Eg FLT3 (intercellular communication), CD markers, VEGF 2. Intracellular kinases a. Normally phosphorylate amino acid residues and tyrosine kinases (BCR/ABL) or serine/threonine kinases (aurora) b. Can be receptor bound (FLT3) or intracellular (BCR/ABL) 3. Gene fusion products a. Confer dysregulated gene function which is usually unique to the tumour cell b. Ege BCR/ABL; PML/RARa 4. Other targets eg proteasome a. The 26S proteasome is involved in intracellular protein degradation via ubiquitination b. It has 3 subunits (1x20S, 2x19S) 3. There are 3 categories of targeted therapy in leukaemia 1. Antibody therapies - specificity and high affinity a. Naked - confer cell mediated cytotoxicity (via attraction of macrophages and NK cells) and complement activation i. Eg Rituximab (anti-CD20 [IgG]) in B-cell leukaemia and NHL (also used in RA and management of graft rejection post-transplant ii. Eg alemtuzumab (anti-CD-52) in CLL and t-cell lymphoma in patients who failed treatment with alkylating agents b. Conjugated - focussed delivery radiation/ cellular toxin i. Eg gemtuzumab ozogamicin (anti-Cd33 tagged with a cytotoxin) used for elderly relapsed AML. The toxin is released following intraceullar lysosomal cleavage loss of specificity makes is undesirable as it has a wide range of side effects eg hepatotoxicity ii. Eg yttrium90-anti-CD66 - beta emitter used in mice studies for multiple myeloma 2. Anti-secreted protein antibodies a. Eg bevacizumab (anti-VEGF) inhibits angiogenesis and hence tumour growth in colorectal, breast and lung ca 3. Small molecule inhibitors a. TK inhibitors i. Imatinib - blocks proliferation, induces apoptosis and low toxicity. Mimics ATP binding site for BCR-ABL in CML (t9;22) 1. T315I (cytosine to thymine at 944) makes isoleucine instead of threonine and is the most clinically relevant of 50+ point mutations in BCR-ABL that confer imatinib resistance 2. Others - 2nd gen = nilotinib, dasatinib, bosutinib are useful in all resistant patients except for T315I 3. 3rd gen agents eg ponatinib show some effect in T315I resistant patients ii. [under development] tandutinib, lestaurtinib, midostaurin target FLT3 ITD in AML. The ITD mutations makes the FLT3 ligand independent and is associated with a more aggressive disease b. Differentation agents i. ATRA - targets retinoic acid receptor in APML (t15;17; PML-RARa) c. Proteasome inhibitors i. Bortezomib inhibits 26S proteasome and thus blocks degradation of IkB = less NfkB activation = antiprolioferative and pro-apoptotic in multiple myeloma and ?MCL 1. It appears myeloma cells more sensitive to the drug, but it can effect other cells to so bortezomib does have side effects Bortezomib inhibits proteasome 26S Proteasome usually degrades IkB IkB usually inhibits Nfkb Nfkb usually promotes proliferation & anti-apoptotic pathways hence the net result of the drug is anti-proliferative & pro-apoptotic 2.16 - ACUTE PROMYELOCYTIC LEUKAEMIA (APML) 1. Clinical features of Acute Promyelocytic Leukaemia Patients usually present with haemorrhage resulting from DIC o Bleeding from venupuncture sitre o Mucosal bleeding o Low platelet count (platelets used up) The mean age of onset is about 40years old, DIC occurs within the first few weeks and can be fatal o Watch out for ganagrene, pulmonary and cerebral haemorrhages o The pathophysiology is due to increased TF rexpression/release by the promyelocytes and increased fibrinolysis (because of annexin 2) Patient may present with a low white cell count, and a higher white cell count is a bad prognostic marker 2. There is no role for immunophenotyping in the diagnosis of APML Morphology - Blood film/ bone marrow aspirate o M3 FAB AML - granular blasts where you can’t really see the nucleus o Faggott cells may appear - they have an abundance of auer rods o M3 variant has less granular/darkly staining cytoplasms - the nucleus may also appear clefted Cytogenetics - FISH o Karyotyping takes about a week - FISH is better because DIC might kill them before this o Looking for characteristic t(15;17)(q22;q21) - PML-RARa Anti-PML antibody? 3. The roles of PML-RARa and outlines of treatment for APML Usually retinoic acid binds to RARa to unwind chromatin and activate transcription PML-RARa binds strongly to the repressor-complex and is resistant to physiological levels of RA. o Less transcription = Block in differentiation at promyelocyte stage o Continued prolioferation and failure of apoptosis ATRA is essentially a super-charged RA dose o It induces differentiation into neutrophils Blast PM M metaM band cell neutrophil o It facilitates apoptosis o The leukaemic clone is replaces by normal cells ATRA is usually used in combination with one cycle of anthracycline-based-chemotherapy. This reduces DIC and thus haemorrhage-related-early-mortality Arsenic is emerging as another treatment o it releases caspase III from mitochondria to facilitate apoptosis o it degrades PMl-RARa without degrading normal RARa o it may be of use in ATRA-resistant patients 4. the ATRA (/differentiation) syndrome is a side effect of ATRA treatment clinical features - SOB, oedema, weight gain, pulmonary infilitrates and hypoBP o (can also occur with arsenic treatment) Believed to be related to rising numbers of differentiating myeloid cells Treat by temporarily stopping ATRA and administering dexamethasone 2.17- PATHOBIOLOGY OF MULTIPLE MYELOMA 1. Origin and phenotype of the myeloma cell and the cellular compartment where oncogenesis develops Functional Ig rearrangement (VDJ), somatic hypermutation and Ig heavy-chain class (from IgM to IgG/A) switching following antigen exposure converts B cells into plasma cells, which reside in the marrow o All these three processes involves double strand breaks = propensity to mutate o Somatic hypermutation and class switching occurs in germinal centres of LNs Plasma cells are dependent on interactions with Bm stroma for survival and proliferation hence it is not normally found in the peripheral blood o They have a low labelling index and make Ig inefficiently o Plasma cell leukaemia is a progression where plasma cells become independent of stroma and hence begin to appear in peripheral blood 2 compartments of dividing cells in myeloma o End stage cell (plasma cell) o Feeder cell (plasmablast) Immunophenotype of myeloma cells o Plasma cells are marked by CD38 & CD138 (syndican1) Myleomatous plasma cells lack CD19 and 50% lose CD27; loss continues with disease progression o Expression of CD56; this is absent in normal plasma cels and in plasma-cell leukaemia o ?CD28 expression in relapse patients o Under-expression of CD45 and over-expression of Cd221 are associated with a worse prognosis 2. Genetic events that lead to myeloma Karyotyping is difficult because cells have slow turnover - you need FISH Hyperdiploidy seen in 60%; pseudo/hypodiploidy seen in 15-20% o Monsomy 13/del (13q) common; upto 50% patients with MM -aasspcoted with worse prognosis o Trisomy 3,5,7,9,11,15,19 common Diploid cytogenetic commonly involve IgH gene locus (14q23) o Primary MM present early with B-cell specific mutations involving switch of J region of the IgH locus (also present in MGUS). o Secondary MM presents late with more complex abnormalities o Juxtaposition of IgH with a gene promoter is found in 48% MGUS, 73% of all MM and 84% PCL 4 categories : t(11;14)(q13;q32) 15-20% Bcl -1 Cyclin D1 NB a different breakpoint in the same 14q32 locus gives mantle cell lymphoma t(4;14)(p16.3;q32) 12% FGFR-1 and MMSET worst prognosis t(14;16)(q32;q23) 5-10% c-maf t(6;14)(p21;q32) 5% Cyclin D3 o Other translocations involving the IgH locus include 8q24 (c-myc), 18q21 (BCL2), 11q23 (MLL1) 20q12 (MAFB). These are rarer Secondary genetic events become commoner with advanced disease. These include further mutatuons in IgH as well as mutations in lamda light chain, del (Rb), P18/ras mutations o Ras mutations accumulate and correlate with disease stage. Mutant ras has less dependence on stroma (IL6) for activation 3. Emerging role of cyclin D activation Cyclins are usually not expressed in lymphoid cells D cyclins (1,2,3) are important or cell cycle progression from G0 G1 o They interact with CDK4 = release of E2F from Rb = transcription & progression T(11;14)(q13;q32) involved with overexpression of cyclin D1 - seen predominantly in light chain myeloma. Associated with a good prognosis T(6,14)(p21;q32) involved with overexpression of cyclin d3 Maf/MAFb mutations may increase levels of Cyclin D2 and trisomy 11 may contribute to increase in cyclin D1 4. Role of stroma cytokines and adhesion molecules in myeloma Normal plasma cell development depends of stroma via interactions through adhesion molecules, receptors and cytokines These interaction regulate proliferation , differentiation and apoptosis of plasma cells Growth/pro-proliferative/anti-apoptosis factors: o IL6, IGF1, VEGF, SDF1a o BM stroma produces IL6. Myeloma cells may also make it when in contact with stroma Inhibitory factors: o IFN-a,b,g, TGF-1b,a 2.18- TREATMENT OF MULTIPLE MYELOMA 1. Spectrum of disease caused by myeloma Proliferation of plasma cells within BM o Symptoms of BM overcrowding/failure; anaemia, neutropenia, thrombocytopenia Cytokine production by plasma cells o Bone resorption = pain. Fractures, hypercalcaemia Paraprotein production by plasma cells can lead to Hyperviscous blood Excess light chain production may lead to amyloidosis RENAL FAILURE caused by recurrent infections (neutropenia), hypercalcaemia, paraprotein and light chain deposits 2. The choice of treatment depends on the ‘stage’ of the disease MGUS may precede active myeloma directly, an intervening period of ‘indolent’ myeloma may also occur There is no treatment benefit by starting early in MGUS/ indolent patients - watch and wait unless there is signs of active /progression of disease: o Presence of M component in serum (as kappa or lamda light chains) and/or urine (as bence jones proteins) Note, M proteins correlate weakly with disease progress o Intact Ig, BJP o Presence of plasma cells in BM o Raised serum light chains in abscence of >10% plasma cells in BM o Ca>2.65, bone disease o Creatinine >177 o Hb <10 Active MM is incurable so aims of treatment are to prolong life/ reduce symptoms o Give Bisphosponates because they reverse bone disease and block mevalonic acid pathway which may trigger an anti-myeloma response Ultimately, the only treatment for active myeloma patients is autologous BM transplant o If patients are not candidates for autografts - melphalan Lastly, if patients relapse after chemo/ auto-SCT - new drugs eg Bortezomib may be used 3. The choice of chemotherapy regimen for autologous stem-cell transplant Standard therapy - Melphalan +/- prednisolone o Low CR [complete response] rate but oral therapy and produces response in 50-60% Px High dose therapy - Cyclophosphamide, thalidomide and dexamethasone has now replaced VAD as high dose regimen in the UK o VAD - vincristine, Adriamycin, dexamethasone + autologous SCT High response rate 65%, CR achieved in 10% Bm suppression, high dose steroids, hickman line and unsustainability of response are weaknesses (median survival is about the same) o Other regimens with similar survival outcomes - COP, CVAMP, VBMCP, VMCP, BVAP Median survival between either regimen is roughly similar at about 4-5 years , relapses also seem to continue at a constant rate between either Allogeneic SCT only applicable to a minority of patients [because most people get myeloma when they are old]. Does offer a cure but has a high relapse rate and high treatment-relatedmortality o Should be considered for anyone <age 55 with matched sibiling 4. Treatment options in relapsed myeloma/ refractory myeloma THALIDOMIDE o Low renal excretion; particularly useful in MM because renal failure is a problem o Supresses TNfa and angiogenesis Morphology of advanced disease shows microvessels - hence anti-angiogenesis may be its most important mechanism o Stimulates IL10, Tcells, B cells (cell mediated immunity) o Teratogenicity, constipation, somnolence, peripheral neuropathy, and thromboembolism are side effects Lenalidomide is more potent than thalidomide in enhancing Nk cell activity, has less incidence of side effects but may produce cytopenias. It is also very expensive. Bortezomib - proteasome inhibitor that leads to decreased activity of NfKB o Proteasomes degrades proteins that are ‘polubiquinated’ [tagged in many sites by ubiquitin] o Tumour cells are highly dependent on proteasome activity because they are high turnover cells o Proteasome inhibiton leads to growth retardation and apoptosis of tumour cells Inhibition of NfKB = decreased proliferation, adhesion molecule and IL6 production, and increased spoptosis through ?caspase mediated pathways o Bortezomib is potent, reversible and selective; it binds to proteasomes with a high affinity and a low turnover rate 2.19 - MOLECULAR TECHNIQUES IN HAEMATOLOGY 1. Descriptions of some molecular techniques in haematology The first step is ALWAYS PCR You have to extract DNA/RNa from cellular (usually WCC) suspensions Then you do PCR - you can use upto 70 cycles if you are looking for a rare molecular target Primer design is important o 18-30bp long o Avoid repeats & complimentary sequences to prevent self-annealing o Limit C/G because they require more heat to denature (4degs as opposed to 2degs with A/T) Then you analyse your product Agarose gel analysis/ Qiaxel segregate fragments within the product according to size/molecular weight - qualitative information only o Qiaxel is preferred because it avoids the need for the bromide (carcinogen) and is much quicker Gene scanning is more sensitive/ specific/qualitative o It can determine sequences and hence is useful in segregating fragments that vary by only a few bases, which would otherwise have a similar weight and be missed on agarose gel/Qiaxel Heteroduplex gel analysis is useful when one allele is mutated and the other is not o It uses slow re-annealing which can generate mismatches in such cases o However this is laborious and you need a lot of sample material Real time PCR uses 2 primers and 1 probe o The probe is degraded by TAQ-polymerase after about 15 cycles, and then produces light o Concentration of your molecular target at the beginning of the reaction effects the number of cycles needed to produce light (cycle threshold) o Hence you can use RQ-PCR to tell how much of your target was in a particular sample o All samples reach the same plateau, but after a different number of cycles Sanger Sequencing is similar to heteroduplex but it will tell you what nucleotides are mutated, hence it is quantitivate, whereas heteroduplex can only tell you if a mutation is present or not (qualitative) 2. Clinical applications of some molecular techniques in haematology Establish clonality in T/B cell proliferations o Sanger sequencing is used to sequence immunoglobulin genes in B cell leukamias o Recap: you have 125V, 3D and 4J segments, any of which can combine for the antigen cinding component of an antibody, then nucleotides are added at V/D and D/J interfaces to get more variety No 2 individuals will ever develop the same sequence on the Ig gene in leukaemia - if you see this, your sample is contaminated Demonstrate chimerism/ monitor treatment post BM transplant o After a transplant, You use PCR with primers designed to flank short tandem repeats and then use gene scanning to see whether the pre-transplant genotype of the host returns - this would indicate relapsed disease/ failure of treatment o Real time PCR can identify very small events - so this is also useful in monitoring treatment response PCr detection of chromosomal abnormalities/ fusion genes o Eg in BCR-ABL, cooperation of primers would suggest the translocation Lastly - microarray analysis is a useful research tool by matching disease to gene expression - but you need a lot of patient samples for it. 2.20 - CYTOGENETICS IN LEUKAEMIA - PRACTICAL OVERVIEW The average gene is about 10-50kb in size, the average chromosome 50-100Mb in size o Cytogenetic is low resolution - usally only to 5mb Acquried cytogenetics looks at mutations in individual cells and is what is used in leukaemia Constitutional cytogenetics looks for mutations in meiosis; inherited diseases like CF, downs Karyotping The first step is preparing metaphase cells for analysis o Colchicine arrests mitosis by inhibiting spindle formation o BrdU/U? Then you stain with giemsa and analyse band formation under a microscope/ using a computer o Dark bands are gene poor and light bands are gene rich o Single cell abnormalities may be artefacts - you need to analyse several metaphases o You need to clone 2 or more cells to prove a translocation/chromosome gain o You need to clone 3 or more cells to prove a chromosome loss o Red herrings are loss/gain of X/Y The genome is usually in equilibrium between tumour suppressor genes and proto-oncogenes o Cytogenetic analyses can pick up monosomies/ trisomies/ trnasloactions which obsiously upset this balance o This provides diagnostic, prognostic and treat-reponse information In nomenclature - for trnaslocations - the involved chromosome that contributed the centromere is termed a derivative It is fast, cheap, screens the whole genome but is low resolution FISH FISH involves labelling targets within the genome with a fluorescent probe o It is rapid, requires less analytical skill, detects sub-micrscopic abnormalities and is useful for slowly dividing cells o Traditional karyotyping is less narrow - this is the major disadvantage of FISH Chronic eosinophilic leukaemia is characterised by CHIC2 (non terminal) deletion which brings PDGFRA into proximity with FIP1L1, creating a fusion gene on chromosome 4 aCGH Array comparative genomic hybridisation involves co-hybridising the sample to a genomic array and using a computer to analyse it. Its major problems are: o Require relatively large quantities of purified disease cells o Expense o Data analysis is complicated by germline copy number variation o Difficult technique to master, prone to unreliable results o More clinical correlations required o Unable to detect balanced rearrangements 2.21 - TECHNIQUES USED IN MONITORING MINIMAL RESIDUAL DISEASE (MRD) 1. Definition of MRD and requirements of monitoring techniques MRD is the lowest level of disease detectable in patients in complete cytogenetic remission by the methods available, hence these methods need to be: o Specific (to demonsrate malignant from normal cells) o Sensitive (because you want to pick up the few malignant cells left) o Reproducible o Quantitative The ideas behind monitoring MRD is that if you can’t completely eliminate the leukaemic clone, you can live with a small number of laukaemic cells because your immune system can keep them under check. Monitoring is needed to make sure the clone does not re-proliferate, so treatment strategies preventing relapse can be employed. 2. Advantages and disadvantages of main techniques used Morphology o Advantage - easy access to source (PB/BM) and rapid test o Disadvantage - poor sensitivity, high false negative rate (especially post-chemo) Immunophenotyping o Ads - rapid, cost effective o Disads - only applicable for about 60% of cases, requires a lot of analytical expertise, and can have low sensitivity Cytogenetics (structural changes, deletions, numerical changes) o Reproducible, cost effective o Poor sensitivity and requires cell division for karyotyping - you would have to wait 6months-1year post chemotherapy for cell division to reach ‘normal’ - therefore cytogenetics is of limited use in monitoring MRD It is useful in diagnostics, prognoses and telling us epidemiology of certain translocations eg young >old Molecular techniques o You can look for (clonal) genes Ig genes for B cells - the ?complimentary dependent region 3 (CDR3) is a locus of added nucleotides that joins [V to D] and [D to J] and is typical of leukaemia primers are designed against this region TCR genes for T cells - primers built against gamma/delta chains (immature) o You can look for fusion genes generated by translocations Fusion genes are specific to leukaemia. Ig/TCR gene rearrangement are done in a polyclonal fashion by normal cells as well, but no normal cell will have a fusion gene You need PCR to monitor patients who have a number of leukaemic cells that is too low for micrscopes to detect. It can also help to identify the very start of a relapse, which can inform clinical decision making Eg. BCR/ABL, PML/RARa 3. Strengths, weaknesses of molecular techniques Ads - reproducible, applicable to 90% of cases, sensitive, becoming more cost effective Disads - requires molecular expertise, can be laborious 2.22 - LYMPHOMA - DLBCL & MCL (this lecture was not actually given) Not sure if this lecture was given or not 1. Pathogenesis in lymphoma Mutations that confer survival advantage/clonal proliferation early in the lymphoid ontogeny leads to: o ALL o Precursor B/T cell lymphoma Mutations that occur later in the ontogeny leads to: o CLL o Mature B/T cell lymphoma 85% of lymphoma is nonhodgkins, i.e. reed-sternberg cells are absent 2. Structure of a lymph node The outer layer (PARACORTICAL) contains T cells The inner layer in the lymphoid follicle: o the germinal centre is where B cells bind antigen and become activated o the surrounding mantle zone still contains naïve, unstimulated, virgin b cells 3. Clinical features of lymphoma Presentation o proliferation of lymphocytes in tissues = lymphadenopathy (+/- local compression/ obstruction) hepatosplenomegaly High WCC Leukostasis o Proliferation of (immature) blasts in BM = Anaemia, neutropenia, thrombocytopenia o B symptoms Diagnosis/staging - BM/ LN biopsy, PET scan 4. Diffuse large B cell lymphoma DLBCL Aggressive Mature b cell (non-hodgkin) lymphoma; accounts for 30% of all NHL Occurs in the elderly Morphology - sheets of large B cells seen in (34%) or after germinal centre (49%) o Within germinal centre is a better prognostic phenotype - associated with ongoing Ig mutations, bcl2 and c-rel amplification o Post-germinal centre has no ongoing Ig mutations and associated with NfKB activation Moleculr - p53 mutation is a worse prognosis Prognosis determined by IPI [international prognostic index] o 1 point each for Age >60, raised LDH, ‘performance status’ 2-4, stage III/IV and >1 extranodal site o 5 year survival is 73% for score 0/1; 26% for score 4/5 Treated with 6-8 cycles of rituximab + CHOP (cyclophos, Adriamycin, vincristine, prednisolone) 50% are cured, consider Autologous SCT for people who relapse - can save 25% of them 5. Mantle cell lymphoma Aggressive Mature B cell (non-hodgkin) lymphoma Affects adult males more (6:1), is disseminated at presentation (multiple large nodes) median survival is 3-5years is worst of all B cell lymphomas - frequently relapses Morphology - low rate of somatic hypermutation of V genes in small pre-germinal centre B cells Immunophenotyping - - aberrant cd5, cd19, cd20, cd22, delta chain, sIgM/D (cd10 and cd23 negative) Molecular - 50-75% associated with t(11;14)(q13;q32) and cyclin d1 overexpression o BCL1/IgH fusion gene = upregulated BCL1 = increased cyclin D1 Cyclin d1 not normally expressed in lymphocytes = unchecked progression into S phase o The same translocation can be found in large cell lymphoma, CLL and MM o additional cytogenetic abnormalities occur in 50% (+12, 13q-(BCMS), 17p- (p53), 11q(ATM), 9p- (p14,15,16) Treat with 3 cycles of R-CHOP, 3 cycles of R-DHAP (platinum-based) and auto-SCT 6. Other non-hodgkins lymphomas Burkitts Aggressive Mature b cell (non-hodgkin) lymphoma Jaw/abdominal sweeling secondary to lymphadenopathy seen in young people Associated with EBV Morphology - proliferation within germinal centre; ‘starry sky appearance’ Cytogenetic/molecular - t(8;14), t(2;8), t(8;22) - all involving c-myc Follicular lymphoma Mature b cell (non Hodgkin) lymphoma - accounts for 22% of NHL Affects elderly as an indolent disease that can transform into an aggressive lymphoma Morphology - arises in germinal centre in a follicular pattern Immunophenotyping - cd10 & bcl6 +ve Molecular - associated with t(14;18) and bcl-2 translocation 7. Outlook in Non hodgkins lymphoma Phenotype Aggressive ~ Indolent Survival Weeks without treatment Months without treatment Years (upto 15) without treatment/ transformation Curability Curable - leukaemia protocols ~ R-CHOP +/- A-SCT Incurable; wait and watch or RCOP 2.23 - CYTOGENETICS AND MOLECULAR GENETICS OF ALL 1. The roles of cytogenetics in ALL Determines prognosis, informs treatment decisions and is useful for MRD monitoring o Vary rarely needed for diagnosis in ALL Cand distinguish and recognise relapses, leukaemogenic mutations and molecular mechanisms in leukaemogenesis 2. Important cytogenetic features of childhood and adult B-ALL Cytogenetic and molecular abnormalities between B & T-ALL differ greatly Children tend to have better prognoses in ALL because ‘good prognosis’ cytogenetic abnormalities are more common, and they are more resilient and hence can survive more aggressive treatment regimens o High Hyperdiploidy (25% children; 8% adults) o T(12;21) (10-30% children; 3% adults) o T (1;19) (5% children; 3% adults) Bad prognosis t (9;22) is occurs in 25% of adult ALL (2% children) Age, gender (lymphoblasts are protected from chemo in CNS & testes) and country where you are treated also influence survival from ALL 3. Genetic features of B-ALL 2 hit model Initial mutation (eg a translocation) in childhood ALL may occur in utero The second hit leads to emergence of the leukaemic clone o Exposure to an environmental agent/ pathogen? - a concordant time gap in between ‘hits’ might suggest this o Deletion of the normal allele in a person where the other copy is already mutated (eg ETV6) o Other cytogenetic abnormalities Child - High Hyperdiploidy 10,17,21 are often triplicated You need centromeric probes in FISH to pick it up The same hyperdiplouid karyotype is odten seen in identical twins Morphologically, it is associated with Common B ALL Child - T(12;21) (p13;q22) Leads to formation of the ETV6-RUNX1 fusion gene o RUNX1 codes for CBFa, which binds CBFb and HAT. HAT allows it to bind to DNA and activate transciprtion for a number of genes including tyrosine kinases o The fusion gene leads to a product which: cannot bind HAT, but remains tethered to DNA binds co-repressor molecules like sin3a, ncor, HDAC heterodimerises via ETV6 to give further transcriptional inhibition Although associated with a good prognosis (95% 7yr EFS), ‘relapses’ can occur - these are thought to be emergence of a sub-clone The translocation is cryptic; the derivatives look similar to the originals - SO YOU ALWAYS FISH Morphologically, it is associated with Common B ALL Child - T(1;19)(q23;p13) Leads to formation of the TCF3-PBX1 fusion gene Unbalanced translocations are common, and involve loss of the derivative of 1 and subsequent duplication on the c1 that was not involved in the translocation Morphologically, it is associated with Pre-B ALL (mu positive) Infant - t(4;11)(q21; q23) Leads to the MLL-MLLT2 fusion gene o This leads to activation of transcription of genes like HOX Morphologically, it is associated with Pro-B ALL; mutations occur in early precursors or the pluripotent stem cell - this can lead to a biphenotypic leukaemia Has the worst prognosis despite more intensive treatment Adult - T(9;22)(q34;q11.2) Leads to the BCR-ABL1 fusion gene o Involves a different breakpoint from that seen in CML Not all cases have abnormal cytogenetics - you need FISH & PCR Presents in middle age and is largely responsible for the ‘second peak’ of ALL incidence with age Poor prognosis, often relapses Another rare cytogenetic abnormality in B-ALL is dic(9;12) where, following translocation, the result is one chromosome with centromeres from both the participants. A Marker chromosome is an abnormal chromosome that marks the leukaemic clone 4. Overview of genetic & cytogenetic features in T-ALL Important loci are 14q32 and 14q11 as these code for the TCR The most frequent cytogenetic abnormality is an interstitial deletion that leads to the STIL-TAL fusion gene (33%) o TAL is Not usually expressed in T cells o The deletion is cyrtpic - you need RT-PCR T(5;14)(q35;q32)is seen in about 20% of T-ALL o Translocation is Cryptic - FISH for it o Leads to HOX11L2 dysregulation T(10;14)(q24;q11) is the third most common cytogenetic abnormality in T-ALL o Leads to HOX11 dysregulation 5 - RECAP - mutations affecting oncogenes in leukaemia Point mutations (eg RAS) Small deletions (STIL-TAL) Internal tandem duplications (FLT3) Translocations that produce fusion genes (many) either by promoter exchange or bringing an oncogene under influence of another promoter Direct gene amplification Insertional mutagenesis following gene therapy 2.24 - IMMUNOPHENTYPING PRACTICAL Morphology- when in doubt, just say you can not tell o M0/M7 AML needs immunophenotyping o Monoblasts may be non-specific esterase +ve Immunophenotyping o Common white cell antigen - CD45 o Myeloid markers - CD117, 13, 33, 15 o 1 immature marker (CD34 or Tdt) is enough Monoblasts can be CD34 negative o CD56 marks Nk cells but is aberrantly expressed on myeloid and myeloma cells o HLA-DR negative is ALWAYS APML MDS - 5q syndrome progresses to AML more readily because of proneness to further mutations, lenalidomide to treat APML - watch for headaches, treat DIC with platelets, plasma and ATRA straight away tAML - t(9;11) [MLL rearrangement] secondary to doxorubicin 2.25 - MULTIPLE MYELOMA (CLINICAL) 1. Epidemiology of Multiple Myeloma D - clonal proliferation of bone marrow plasma cells, characterised by production of one/both of monoclonal antibodies (termed paraproteins) and free Ig light chains (BJP). I - incidence is 3.5k in UK A -OLD; median age 70 S - M>F (just) G - Blacks > white A - UNKNOWN 2. Pathophysiology of disease in Multiple Myeloma 3 main mechanisms of disease Proliferation of plasma cells o Anaemia (common presenting symptom) o Neutropenia (recurrent infections +/- sepsis) o Thrombocytopenia Cytokine production o TNFa & IL1b stimulate osteoclasts = bone damage, lytic lesions, hypercalcaemia Osteoclasts make IL6 which stimulates plasma cells, reduces albumin and raises CRP o Bind to osteoblasts/ BM stromal cells to further stimulate osteoclasts via RANK/RANKl pathway Monoclonal antibody and/or light chain production o Most commonly IgG / IgA are produced, there raise ESR and lead to rouleaux formation o Free light chains circulate as BJP and can contribute to renal failure o BJPs can bind to plasma protein to lead to amyloidosis o 25% of patients have BJP only (no paraprotein) - hence these may have normal ESR Pathophysiology of renal failure - Hyeprcalcaemia, recurrent infections, antibody and/or light chain deposits Pathophysiology of bone disease = lytic lesions, BM growth due to plasma cell proliferation, osteopenia 3. Clinical features of multiple myeloma Symptoms/signs/examination o Symptomatic patients present with symptoms of anaemia, hypercalcaemia, bone disease and renal disease o Patients can be aymptomatic in MGUS and early active MM Investigations o Bloods - Raised ESR (in paraprotein +ve MM), CRP, calcium, low albumin o Film - rouleaux in blood film, clonal plasma cells >10% in BM (presence in BM = PCL) o Immunophenotyping - CD56, CD138, clonal expression of either kappa/lamda light chain o Cytochemistry - immunoperoxidase staining for CDs, cyclin D1 and light chains o Serum protein electrophoresis - dominant M band o Beta2macroglobulin = marker of tumour load and renal function ISS staging system (2005): Stage 1 2 3 B2 macroglobulin <3.5 Between 3.5 and 5.5 >5.5 Albumin >35 <35 4. Treatment options in multiple myeloma Symptomatic management Hypercalcaemia - fluids, steroids bisphosphonates (IV zoledronic acid) o Bisphosphonates improve bone symptoms and reduce need for radiotherapy to ease bone pain etc Conventional chemotherapy regimens & high dose chemotherapy + AutoSCT have similar OS Conventional: o Cyclophosphamide, Thalidomide and Dexamethasone for most patients o Melphalan and prednisolone for the elderly High dose chemotherapy + AutoSCT o Attal et al 1996 - as compared to conventuional therapy, high-dose therapy achieves greater CR but has similar OS Hence AutoSCT is the treatment of choice o Child et al 2003 (Myeloma VII) confirmed these findings AlloSCT is the only cure but is only applicable to the minority of patients Only applicable for a small group of patients: age <50 and with a matched sibling Transplant related mortality is high Curative in about 20% of patients Females, early disease stage, being in CR are good prognostic factors How to improve survival in MM? [median survival now is about 6 years] Use different chemo regimens Tandem (>1) transplants - IFM94 study says it improves OS CD34 selection and starting SCT early seem to have no effect 5. New agents in Multiple Myeloma Thalidomide o Immunomodulatory - anti adhesive, anti TNfa and anti IL10; stimulates host lymphocytes o anti-angiogenic; anti FGF and anti VEGF o Effective in about 60% of patients, oral admin and CHEAP o SFX = constipation, somnolence, peripheral neuropathy, VTE Bortezomib o Reversibly inhibits chymotryptic active site of proteasome beta subunit = NfkB inactivation = less transcription of IL4, VEGF, adhesion molecules o Key study was APEx; Richardson et al 2005 o Effective in 40% of patients, fast responses o Main SFX = thrombocytopenia, neutropenia, anaemia, peripheral neuropathy. Very expensive and requires IV admin Lenalidomide o Advantages - oral admin, appears to be more potent than thalidomide o Diadvantages - very expensive, VTE. neutropenia 2.26 - COMPLICATIONS OF LEUKAEMIA THERAPY 1. Types of leukaemia and their therapy CML - TKIs ALL - combination chemo (FCR; fludarabine, cyclophosphamide, rituximab) Acute leukaemias - combination chemo SCT is an option for all leukaemias 2. Principles in chemotherapy Chemotherapy is aimed at dividing cells. Tumour cells are more proliferative and they divide inefficiently and hence spend a longer total time undergoing division = proness to chemo Types of chemo: Antimetabolites Mitosis inhibitors Enzyme inhibitors Alkylating agents Anthracylines Other - TKIs, monoclonal antibodies 3. Systemic effects of chemotherapy Nausea/Vomiting o Melphalan and anthracycline are bad o Prophylactic ally/therapeutically give anti-emetics, particularly 5HT3 inhibitors eg ondansteron Alopecia o Can recover but may be patchy. Offer wig Dose-dependent bone marrow suppression o Alkylating agents are the worst o Treat anaemia with transfusions/ EPO o Treat thrombocytipenioa with platelets o Be careful of neutropenia; <0.2e9 is high risk of infection; <0.1 is high risk of sepsis from gut commensals Drug extravasation (local inflammation, necrosis etc) o Rarely a problem because most people are on central lines rather than cannulas TUMOUR LYSIS SYNDROME o Particularly pertinent in acute leukaemias with a high WCC and Burkitts lymphoma o = Hyperuricaemia, kalaemia, phosphataemia and hypocalcaemia = dehydration, metabolic acidosis, ARF, death o Prevent with allopurinol or rasburicase for the above two diseases 4. Organ-specific effects of chemotherapy renal Antimetabolites Mitosis inhibitors Alkylating agents Anthracyclines bladder cardio liver GI √ √ √ √ √ √ √ √ neuro √ √ √ Repro √ Long term effects: Cerebellar ataxia with antimetabolites (cytosine arabinoside) Sterility with most (freeze sperm/ eggs/ embryos to prevent) T-AML, Bladder Ca and Pulmonary fibrosis with alkylators 5. Side effects of stem cell transplant Acute/chronic toxicity of chemo = problems seen with the table above Acute neutropenia = infections (bacterial and fungal) Effects of immunosuppression = o Chronic/late infections (pneumococcus, PCP, CMV) o Acute GvHD (skin, gut liver) Prevent/treat with immunosuppressive (cyclosporine, tacrolimus, rapamicin, MMF, CAMPATH) and corticosteroids o Chronic GvHD (presents like scleroderma; skin, gut, liver lungs) Prevent/treat with immunosuppressive (cyclosporine, tacrolimus, rapamicin, MMF, CAMPATH) and corticosteroids Long term complications o Endocrinopathy (thyroid, adrenals, growth retardation) o Infertility o Cataracts o Pulmonary dysfunction o T-AML 2.27 - LEUKAEMIA - PAST,PRESENT & FUTURE Cml 1882 - Arthur conan doyle found arsenic to have an effect on CML like syndrome 1950s - nitrogen mustards and bisulphan used to treat 1973- 9,22 translocation established 1980 - BCR/ABL1 fusion gene established 1980s - alpha interferon used to treat IRIS trial 2003 - imatinib Now we can use PCR to monitor MRD with people on imatinib therapy Used to be universally fatal 1930s - folic acid found to make it worse o Idea emerged that antifolate (aminopterin) can induce remission 1950s - 6mercaptopurine used but associated with CNS relapse Now combo chemotherapy mean >90% ALL can be cured We can use cytogenetics to monitor MRD ALL Hodgkin lymphoma Hodgkin recognised the syndrome in 1832 following post mortem analyses Reed and Sternberg characterised the characteristic multinucleate cell between 1898-1902 o Both postulated TB to be associated with it 1940s - role of brucella in aetiology? 1960 - cytogenetics demonstrated aneuploidy and clonal derivation Staging from the 50s onwards has progressed from lymphograms open surgery CT PET-CT (this is what is now used) Combination radiotherapy (ABVD) and radiotherapy is now used to treat 2.28 - APML - A PARADIGM FOR MOLECULARLY TARGETED THERAPY 1. Recap of genetic basis of APML APML is all about repressed transcription giving a halt in matuaration at the promyelocyte stage. Mutations in these committed cells gives them the capacity to self renew - which is a property of stem cells Disruptuon of PML nuclear bodies by PML-RARa may be a key effect o Normal PML makes the outer shell of nuclear bodies o NBs contain other proteins eg pRb, p53 and BLM hence normally functioning NBs play key roles in apoptosis, senescence, growth suppression and genome stability o Abnormal PML leads to microparticualte distribution of proteins usually encased within Nbs 2. Mechanisms in t-APML can inform us of ‘weaknesses’ in the genome In t-APML, there is clustering of breakpoint s within intron 6 of PML and RARa following prior exposure to mitoxantrone o mitoxantrone is used for breast cancer and MS 4 breakpoints are clustered within 8 base pairs on PML o The fact that 1 in 400 MS sufferers treated with mitoxantrone develop t-APML, and experience the same breakpoints, suggests that this area of the genome is a favoured topoisomerase-II cleavage site and thus is prone to sustained damage but topoisomerase-Ii poisons such as mitoxantrone 3. The future of APML management may see the abolishment of chemotherapy ATRA achieves the following by binding to the ligand-binding domain of RARA: o Degradation of PML-RARa o Replaces co-repressor molecules bound to PML-RARa with activators o Reformation of PML in nuclear bodies o Terminal differentiation, upregulation of TRAIL and induction of apoptosis Arsenic achieves the following by binding to PML: o also induces degradation of PML-RARa and thus achieves differentation o inhibits angiogenesis o induces apoptosis by multiple mechanisms you can use molecular monitoring (PCR for PML-RARa) to: o tailor treatment regimes o intervene early and monitor continually - this reduces relapse rate o allow admin and monitoring of low dose chemo (which confers reduced toxicity) studies suggest low dose regimes have better survival current evidence suggests completely withdrawing chemo does not affect survival - win! o Molecular monitoring is probably cost effective in badly diseased patients other potentials for molecularly targeted therapy: anti-CD33 + chemo for AML that has core-binding-factor rearrangements (eg t8/21, inv(16)) molecular monitoring may also be useful to predict relapse in NPM1 mutated AML patients 2.29 - LYMPHOMA AETIOLOGY AND BURKITTS LYMPHOMA 1. Overview of aetiology of lymphoma Multifactorial disease aetiology Inherited predisposition may relate to immunodeficiency: o Abberant immune response to infections (certain HLA groups are prone, SCID) o Defective DNA repair (ataxia telangiectasia/ Nijmegen breakage syndrome) o Polymorphisms in DNA repair genes o Polymorphisms in genes encopding complement] Acquired immunodeficiency o Induced by HIV o Iatrogenic - particulary following heart/lung transplant or methotrexate use Environmental exposure to mutagens (pesticides, herbicides, fertilizers in follilcular lymphoma) INFECTIONS o Bacteria, viruses, malaria Auto immune diseases (cioeliac, hashimotos thyroiditis, sjogrens, RA) Blood transfusion? NHL 2. Role of bacterial agents, namely H.pylori, in lymphoma aetiology Types of bacteria involved in lymphoma H Pylori (T cell gastric MALT lymphoma) Campylobacter - (immunoproliferative small intestinal disease; IPSID) TB - pyothorax associated lymphoma Maybe borrelia and chlamydia too H.Pylori in gastric MALT lymphoma Proof of aetiology o 90-95% of g-MALT lymphoma patients are infected o Incidence of gastric MAL lymphoma is increased 6 fold in infected people o elimination of the infection (antibiotics) leads to remission The bacteria stimulates T cells, the T cells lead to chronic stimulation of B cells The disease becomes autonomous from infective stimulation (and thus refractory to antibiotics treatment) following other genetic events o T(11;18) BIRC3-MALT1 fusion gene = BCL10 dysregulation o T(1;14)= BCL10 dysregulation o T (14;18) = BCL2 dysregulation because a MALT1 fusion gene is formed o Associations with autoimmune diseases and fas mutations can also lead to refractory gMALT Borrelia may play a similar role in the aetiology of cutaneous MALT lymphoma Infection = stimulated CD4 T cells polyclonal B cell expansion, dependent on bacterial antigens random translocation etc monoclonal B cell expansion; independent of bacterial antigens 3. Role of viral agents, namely EBV, in lymphoma aetiology Types of viruses involved in lymphoma HIV o Both HL & NHL (intracerebral DLFBL, Burkitts) HIV surpresses T cell function in burkitts and EBV/oppurtunistics stimulate B cells o May be in part related to EBV co-infection (1/3 patients have this) Herpes viruses o EBV - endemic Burkitts, many classical HL o HHV8 - primary effusion lymphoma (EBV may be a cofactor); CD30+ CD138+ HTLV1 - TALL HCV - salivary gland MALT lymphoma Lymphoma mechanisms in viral infection Expression of viral oncogenes Transactivation of host ptoro-oncogenes Insertional mutagenesis Induction of chronic B cell stimulation Supressed T cell function EBV in endemic Burkitt Lymphoma Endemic Burkitts is an aggressive lymphoma that causes jaw tumour in children, spread across the malarial belt o Sub aharan Africa, south America, papua new guinea o Geographical areas within these countries that confer pro-malaria conditions have higher sub-incidences EBV and malaria act as a team in the aetiology of endemic burkitts o EBV causes chronic B cell stimulation o Malaria does the same but it also surpresses t cell function It is also associated with splenic marginal zone lyphoma o A random mutation (eg dysregulation of myc or p53) is what ultimately leads to monoclonal expansion of (usually) IgM B cells Diagnosis of Burkitts o Cytogenetics - 3 trasnlocations associated with emergence of endemic Burkitts A breakapart probe in FISH is useful because they all involve myc so it can pick up any of the three o Morphology - vacuolated basophilic cytoplasms; appearance of macrophages that have ingested apoptotic material o Immunophneotype - CD34-, Tdt-, SmIG+, B markers and BCL6 [mature B] CD10+ (but this is also seen is normal follicle cells) Translocation Fusion product Frequency T(8;14)(q24;q32) MYC-Ig heavy chain 90& T (2;8) Myc-kappa light chain 5% T (8;22) Myc-lamda light chain 5% Other roles of EBV in lymhpoma: o Can cause classical hodkin lymphoma incidence increases 2-3y after glandular fever is present in neoplastic cells encodes for oncogenic proteins latent membrane protein 1 [LMP1] induces BCL2 LMP2 downregulates development genes and upregulates proliferation genes o Can cause DLBCL (latent membrane protein 1 may be important) o implicated in post-transplant lymphoprliferative diseases o Richters syndrome in CLL (where B cells that are clonally related to CLL invade tissues) o Lymphoma in people who are immunodefiencent follwoinf drug therapy (infliximab, methotrexate) Sporadic (non-endemic) Burkitts The same translocations are seen but the exact breakpoints are different from what is seen in endemic burkitts o EBV might be the key difference in mediating this Soradic is only associated with EBv in 10% of caes Affects abdominal organs (ovaries, caecum0 and breasts HCV in lymphoma The importance of HCV in lymphoma seems to vary by country It causes monoclonal cryoglobulinaemia which leads to tissue necrosis o Associated with SLVL, MALt lymphoma of salviares, DLBCL Patients with splenic marginal zone lymphoma appear to regress when HCV infection is treated 4. Role of auto-immune and other non-infective diseases in lymphoma etiology Principle is the same with inefctions - antigenic stimulation of host lymphocytes = chronic proliferation Autoimmune diseases seem to give an increased incidence of Hodgkin lymphoma o Sjogrens increases risk 6 fold (marginal zone, DLBCL, FL) o SLE increases risk of DLBCL and Marginal Zone Lymphoma 3 fold o Psoriasis and coeliac assoacited with T cell lymphoma Coeliac gives a high grade lymphoma of T mucosal lymphocytes o i.e. the lymphoma arises in a T cell subset which is different to that which mediates the autoimmune disease o Incidence is increased 80x in people are left undiagnosed/untreated The autoimmune lymphoproliferative syndrome (ALPS)is a chronic polyclonal disorder resulting from mutations that lead to failure of apoptosis o Increased incidence of B NHL & HL as well as autoimmune diseases 2.30 - HTLV1 AND ATLL 1. Spectrum of disease caused by HTLV1 infection is somewhat dependent of proviral-load Brief Epidemiology of HTLV1 The infection is almost as prevalent as HIV worldwide Particularly common in sub Saharan Africa, peru, japan and amongst aboriginals Disease of the elderly Proviral load and disease spectrum Importantly, the proviral load does not vary over an individuals’ disease course, but there is varability between different infectees Low proviral load correlates to asymptomatic disease features o Recurrent shingles o TB o Helminth infections e.g. strongyloides (watch for G-ve sepsis following bowel inflammation) o Infective dermatitis (chronic infection in children) Higher proviral loads correlate with symptomatic disease features after a long latent period o Presentation is at ago 60+ usually o Adult T cell leukaemia/lymphoma (4 subtypes) o HTLV1-associated- myopathy Weak & stiff legs, lumbar pain, leg pain, bladder dysfunction, erectile dysfunction, constipation Strongly resembles MS The presence of CSF HTLV1 antibodies distinguishes it from MS o Chronic multisystem inflammatory diseases (alveolitis, uveitis, polymyositis) The STLV1 virus produces a similar disease phenotype hence the immune response to the pathogen, rather than the pathogen itself, might be key. 2. Features of adult T cell leukaemia/lymphoma Type indolent Smouldering (5%) Chronic Leuk (15%) Aggressive Lymphoma (20%) Acute Leuk (60%) Lymphoc Abnormal ytes T cells <4e9 >5% Ca LDH Other Survival Normal <1.5x 24mon >4e9 >5% Normal <2x <4e9 <1% >4e9 >5% Can be high Can be high Can be high Can be high Skin/lung lesions Liver,spleen, skin, lung LNs Tumour lesions 6mon 24mon 10mon Signs/symptoms o Bm failure (anaemia, thrombocytopenia) o Hypercalcaemia (mehcnaisms similar to what is seen in myeloma) o Generalised lymphadenopathy - watch for SVC obstruction o Hepatosplenomegaly o Skin lesions - always biopsy - skin lesion appearance varies gretly between patients. Nodular lesions are the ‘classic’ appearance o Lytic bone lesions Investigations o Bloods - Bm failure, high WCC, high Ca, high LDH (marker of cell turnover) o Film - flower cells (large cells with indented/lobulated nuclei) o Cytogenetics - no classic hallmark o Immunophenotpye - CD4+ CD25+ o Always do an Lp because, like burkitt lymphoma, it commonly spreads to CNS and crytpoccal meningitis is also common in ATLL so rule this out too Management o Aggressive T-ALL - ½ cycles of CHOP + AZT/IFN but we don’t know when to start AZT o Indolent t-ALL - AZT/IFN o Relapsed t-all - DHAP/ new drugs (anti CD25, HDACi’s, bortexomib, ATO)/ alloSCT Difficulty with alloSCT is that most sbilings are infected too so you have to look for unmatched donors 3. Virology in T-ALL HTLV1 is essential to cause T-ALL Vertical transmission is via breastmilk Horizontal transmission is similar to that of other blood borne viruses Mechanism of infection It is a retrovirus - its uses reverse transcriptase before incorporating into host T-cells In early stages of disease - cell-cell contact is how it spreads between cells o This is why you can’t find anything in the plasma From then on, the virus replicates by conferring the clonal expansion of the infected cells How does HTLV1 cause cancer? Two ways in which the provirus affects host genome o Acute - Transcription of an oncogene that happens to have existed within the provirus o Chronic - the provirus acts as a gene promoter itself and leads to transcription of protooncogenes within the host genome e.g. myc Important proteins o TAX - expressed in 40% of T-ALL Involved in a lot of cellular pathways but generally it immortalises the CD4 cell, drives tumour formation and is immunodominant Tax activates NfKb, AP1, SRF, NFAT, CREB/ATF It downregulates beta-polymerase Cell cycle progression (expression of cyclin G2) Inactivation of p53 (ATLL with wild type p53 responds to zidovudine) Induction of apoptosis (through Fas/FasL and IL-1b converting enzyme (ICE)). Inhibition of apoptosis (Tax inhibits anti-APO-1 induced T-cell death, represses transcription of Bax gene and up regulates BCL2). Decreased Genomic Stability Telomerase o HBZ - its mRNA in seen in all cases of TALL and it seems to drive tumour formation o These proteins are not oncogenes - only 5% of HTLV1 infected people actually get TALL The basic leuice zipper domain promotes t cell proliferation and represses tax o This suggests a complex regulatory mechanism of viral load etc 2.31 - LYMPHOPROLIFERATIVE DISEASES 1. MALT lymphoma Epidemiology o Defined as extranodal marginal zone lymphoma of MALT o Comprises 8% of all NHL o Presents at 55-60years old o Commonly arises in stomach, but also in many other organs Disease course o Indolent in most patients; 5yr survival 80-95% o Nodes usually only involved after local spread; <15% involve BM o A minority transform to aggressive DLBCL Diagnosis o Cytogenetics - t (11;18)(q21;q21) o Immunophenotype - CD20+ CD10- CD5o Molecular - BIRC3-MALT1 Aetiology - H pylori Treatment - 2 weeks triple therapy (PPI, amoxicillin, clari/metro) works in 85% of cases o 50% of those who don’t respond/relapse after MRD, respond to chlorambucil o Rituximab may also be useful 2. Primary CNS Lymphoma Epidemiology o Comprises <2% of all NHL o Presents at median 61 years old o Incidence of upto 10% in AIDS patients Disease course o >95% are B cell tumours o 2/3 present as solitary CNS lesions o Median overall surviala about 5 years following combination therapy; radiation is bad? Outlook for PCNSL has improved significantly due to intensified chemotherapy Removing DXT from therapy of patients may reduce toxicity without compromising outcome Some patients with refractory/relapsed disease may be salvaged by HDT 3. Lymphoma in Pregnancy Epidemiology o Occurs in 1/3k pregnancies, usually as a HL o No evidence that HL influences outcome of pregnancy or vice versa o If NHL – particularly bad prognsosis if it presents aggressively (90% of px) Difficulties: o Accurate staging is difficult because you can’t use CT in pregnancy - dangerous for baby o Is it safe to do chemo? Treatment o Do nothing - probably safe for HL o Terminate pregnancy? Probably only for aggressive NHL presenting early in pregnancy o Avoid radio o ABV/ABVD in second half of pregnancy for HL; CHOP for aggressive NHL o vinblastine until pregnancy is completed and then revert back to ABV/ABVD 2.32 - INFECTION & LYMPHOMA 1. How infectious agents contribute to lymphoma Direct infection & neoplastic transformation of lymphocytes o EBV - germinal centre/post germinal centre B lymphomas and almost all extranodal NK/T cell lymphomas o HHV8 - primary effusion lymphoma (with EBV as a cofactor) & LBCL arising from multicentric castleman disease o HTLV1 - ATLL o HIV - primary CNS DLBCL, DLBCL and Burkitts Immune suppression leading to increased risk of lymphoma o HIV o EBV - causes >2/3 of B cell related post-transplant lymphoprolfierative disorders (within 5 years of transplant) o Immunosuppressive medication, increasing age, SCID Chronic (antigen-mediated) stimulation of the immune system o i.e. the lymphoma cell is not infected itself o H pylori (gMALT) and other bacterial infections; tend to be associated with low grade, indolent, usually marginal zone lymphomas 2. Methods of detecting infectious agents in lymphoma Detection of EBV o FISH for EBER1 o Cytochemistry using anti- EBNA1, anti-EBNA2 or anti LPM1 Detection of HHV8 o Cytochemistry using anti-LANA1 or anti-vIL6 Detection of HTLV1 o Serology 3. Role of EBV in molecular pathogenesis of Burkitt & classical Hodgkin lymphoma Classical HL - EBV confers autonomous signalling pathways EBV infects >90% of cHL patients, and these patients have a higher EBV Ab titre The rise in EBV Ab development precedes the lymphoma There is an increased risk of developing cHL following glandular fever There appears to be a need for CD4 cells for EBV to mediate disease - incidence increases as you start treatment for HIV in co-infected patients Molecular roles of EBV o EBV rescues B cells with crippling IgH mutations from apoptosis before they leave the germinal centre o LMP1 induces B cell activation markers, adhesion molecules and upregulates antiapoptosis genes o LMP1 also activates JAK/STAT NfKb pathways so they become ligand independent o LMP2A allows B cells to survive without signalling from Ig Endemic Burkitt lymphoma - EBV generally cofners an escape from apoptosis Malaria infects RBCs and presents the molecule PfEMP1 on their CSMs. A region on this molecule, called C1DR1a can bind to and activate B cells In Burkitt lymphoma each follicle expands roughly 10x The translocations in Burkitt lymphoma involve upregulation of myc o Subsequent p53 mutations are seen in 1/3 patients - aberrant apoptosis o Mutant myc fails to upregulate BIM1, which is usually essential for apoptosis o Upregulated PIM1 further counteracts p53 Molecular roles of EBV o EBNA3A & -3C hypermethylate BIM1 = downregulation = less apoptosis o EBNA1 is also anti-apoptotic o EBER1 promotes proliferation and secretion of the b cell growth factor IL10 4. Molecular roles of HHV8 in primary effusion lymphoma LANA1 inhibits p53 and thus impairs apoptosis Viral cyclins resemble host cyclins so this leads to continuous proliferation FLICE protein blocks caspase activation and apoptosis mediated by Nfkb Viral IL6 stimulates B cells 2.33 - FOLLICULAR LYMPHOMA 1. Introduction to lymphoma Lymphoma is a clonal expansion of lymphocytes, usually B lineage, into tissues of the body Lymphomas can be classified based on the characteristics of the B cell they arise from, particularly the stage of maturity in reference to lymph node anatomy: o Naïve/pre germinal - CLL/SLL o Pre-germinal/manle zone - MCL o Germinal - Burkitt, Follicular o Post-germinal - MZL/ extranodal MALT lymphomas o Plasma cell myeloma 2. Clinical features of follicular lymphoma D - low grade germinal centre, non Hodgkin, lymphoma I - accouints for 22% of all lymphomas; second most common after DLBCL A - adults S - F>M G - western world/industrialised countries A - almost nothing is known; folate deficiency may be a risk factor P - growth of LN follicles; lack of macrophages from follicles helps differentiate it from reactive hyperplasia; (which requires macrophages as it is an antigen driven process) C - usually spreads slowly so that it is a disseminated disease at presentation - LNpathy, splenomegaly and BM invasion my occur. Can transform to a high grade DLBCL or Burkitts. When it relpases, the time intervals between relapses progressively decline. 3. Grading/ Staging of follicular lymphoma Grade Grade 1 & 2 are low grade. 3 a can also behave indolently Grade 3b behaves more like a high grade lymphoma Stage 4. Determined by examination, bloods, biopsies, CXR, CT and PET (radioactively labelled glucose - picks up high metabolism tissues inc. heart, liver, bowel) 1 - single LN/ structure affected 2 - >2 structures on same side of diaphragm 3 - involvement of both sides of diaphragm 4 - invasion of non lymphoid tissues o All - A/B depending on whether ‘B’ symptoms are present or not Morphology of follicular lymphoma Nuclear cleft presence is indicative of germinal cell lymphomas Chromatin is evenly condensed - this helps differentiate it from CLL, where chromatin is patchy Trephine biopsy shows paratrabecular infiltration 5. Immunophenotype of follicular lymphoma Flow: o CD10+ (germinal cell), CD19, 20,22 + (B), CD 45+ (WCC) o CD5 - (identifies it from CLL), CD3-, CD15,30- (these are HL markers), CD34, Tdt(lymphoma cells are mature) NB CLL will also display CD23 o One of kappa or lamda light chain Immunohisto: o BCL2+ - this is key to diagnosis 6. Cytogenetics & molecular features of follicular lymphoma T (14;18)(q32;q21) is the hallmark - brings BCL2 under the influence of IgH@ enhancer o There are 4 cluster regions of breakpoints on IgH - 2 major & 2 minor; each major is nearer the 3’ end of the gene locus o BCL2 is juxtraposed against the J region of IgH. It normally prevents efflux of cytochrome C from the mitochondria and thus confers apoptosis o Normally, unstimulated B cells die - this control is lost T(2;18)(p12;q21) kappa and t(18;22)(q21;q11) are also possibilities Hence follicular lymphoma could be an error of normal class switching You can detect this with FISH & PCR o Use a breakapart probe for 14q32 and this will detect any of the 3 translocations RQ-PCR is useful for MRD monitoring 7. Treatment of follicular lymphoma Most options are aimed at palliation. AlloSCT + local radio offers the only hope for cure but very few patients can survive the treatment Involved field radiotherapy - stages 1 & 2 Chemo-immunotherapy is now considered the optimum treatment for symptomatic stages 3/4 o CVP + rituximab We still don’t know what to do for advanced stage, asymptomatic patients - the rationale for delaying treatment until the patient experiences symptoms is to avoid drug resistance 2.34 - IMMUNOPHENOTYPING IN LYMPHOMA 1. The roles of immunophenotyping in lymphoma Distinguiosh lymphoma from reactive conditions Distinguish lymphoma from CLL/ALL Help make a diagnosis Helps to reveal specific aetiologies Helps to give prognostic information Can allow monitoring or MRD 2. Techniques of immunophenotyping Immunocytochemistry Immunohistochemistry Flow Cytometry All of the methods can detect CSM antigens, cytoplasmic antigens and nuclear antigens. However, flow cytometry needs cells to be permealised to detect the latter two. 3. Distinguishing reactive lymphocytosis from lymphoma by immunophenotyping In reactive conditions, about 2/3 of lympohcytes display kappa whereas 1/3 display lamda In neoplasms, all cells express one or the other For t cells, uniform expression of CD4/CD8 points to lymphoma o Also look out for abnormal expression on T-antigens for example a reduced expression of TCR a/b as compared to g/d [normally, it is the other way around] 4. Distinguishing lymphoma for ALL/CLL B-lymphoma o ALL will usually express TdT, maybe CD34 and are usually SmIg and FMC7 negative T-lymphoma o ALL will usually present TdT and maybe CD34 o Thymic t cells make CD1 o Early T cells have cytoplasmic CD3, whereas mature lymphomatous cells will express surface CD3 o Early t cells co-express CD4/CD8 before they are selected for 5. Panels for diagnosing lymphomas Diagnosing B cell lymphoma o Exclude T cell lymphoma - CD2 negative o Confirm B cell lymphoma - CD19, 22, 23, 79b kappa/lamda positive Diagnosing T cell lymphoma o CD3, CD7, CD4/8, CD25 6. Classic immunophenotypes lymphoma B-cell lymphomas CLL - CD5+, CD23+, CD19+ weak SmIg, 22, 79b FMC7 o [CLL score >4 is very likely; CD23 is not included in this scoring system] o ZAP70 and CD38 in CLL confer a worse prognosis NHL – opposite to CLL - CD5-ve (except MCL), CD23-ve, SmIG+ve, CD22,79b, FMC7 +ve o Mantle cell - cyclin D1+, CD5+, CD19+ o Follicular CD10+ve o Hairy cell - CD11c, CD103, CD25+22, CD123 [Most patients have atleast 3 of these four markers] Myeloma - CD19-ve CD56+ve, CD138+, CD38+ve, cytIg, CD79a [normal plasma cells are CD19+ve, CD56-ve i.e. the opposite to myeloma cells] T-cell lymphomas Large granular lymphocyte leukaemia - CD11b, CD16, CD56, CD57, TIA1 o NB this can be T or NK lineage ATLL - CD4+, CD25+ve, HLADR, CD38 and CD71 +ve o increased sideways scatter because of flower nucleus (more complex = more scatter) NK lymphoma - CD5-ve, CD79a-ve 7. Monitoring lymphoma MRD Needs multi-parameter flow cytometry o This allows different cell populations to be identified o It uses more antibodies to detect subtle changes i.e. strength of antigen expression, clonality/ emergence of a sub-clone/ aberrant antigen expression 2.35 - PATHOLOGY OF NON-HODGKIN LYMPHOMAS 1. WHO classification of lymphoma Low Grade High grade B NHL SLL (small lymphocytic lymphoma) MCL Follicular MALT DLBCL Burkitts Lymphoblastic lymphoma T NHL Mycosis fungoides Anaplastic ATLL enteropathic 2. Clinical features of NHL (largely a repetition from previous Barbara bain lecture) D - a lymphoma without the presence of reed-sternberg cells I -on the up due to increasing AIDS & more frequent SCTs (immunosupression) A - mean = 42 S - M>F G A - Immunodeficiency (AIDS, SCT) AI disease (RA, SLE) Chromosomal abnormalities T14/18 = follicular T11/14 = mantle T8/14 = burkitts Infections (EBV, HIV, HTLV1, H.Pylori) Chemicals (AAs, radiation) Inherited factors/ familial and racial trends P -excised lymph nodes usually display diffuse whiteness and increased size C - insidious (especially with low grade) lymphadenopathy with or without B symptoms - tumour bulk can impact local structures - lymphomas can invade BM (anaemia, neutropenia, thrombocytopenia) - you can get autoimmune disease with some lymphomas Diagnosis - FNA cytology can be useful in those that have spread to blood, but otherwise you need LN excision biopsy under GA P - depends on age, LDH, staging, extranodal involvement(s). some molecular and histological markers can also determine prognosis 3. Low grade lymphoma vs high grade lymphoma LOW GRADE Indolent/ slow progression Presents late, disseminated Difficult to treat; impossible to cure Occurs in adults HIGH GRADE Aggressive/rapid progression Presents early May be curable with chemotherapy (40-50%) Can occur at any age 4. B cell NHL CLL/SLL Accounts for 5% of NHL; presents in elderly (60years) Indolent lymphoma that is usually disseminated at presentation, maybe with BM involvement Chemo can not cure it - median survival is still 10years (indolent) 3% cases can transform to DLBCL Pathology o Small round lymphocytes with little cytoplasm o Cant see follicles in LNs o Lymphocytes may invade nearby adipose tissue o Immunophenotype - CD5+, CD23+ MCL Indolent lymphoma that presents in the elderly but disseminates early and thus only has median survival of 3-4years Pathology - cells appear similar to CLL/SLL Immunophenotype - nuclear cyclin D1, CD5+, CD23Cytogenetics - t11/14 = upregulated cyclin D1 Follicular Indolent lymphoma that presents in the elderly of developed countries Pathology - follicles expand and extened into LN medulla Immunophenotype - CD10+ve, Bcl2+vem CD10+ve Cytogenetics - most have T14/18 = dysregulated BCL2 = dysregualted apoptosis MALT An extranodal marginal zone lymphoma associated with autoimmune disease (sjogrens in salivary gland lymphoma) and infection (h pylori, campylobacter) One of the only haematological malignancies that is more common in women (AI Dx) Pathology - lymphatic destruction of glands Immuniphenotype is of no use in gastric MALT - you need an endoscopy Lymphoplasmacytic lymphoma/ Waldenstroms Can progress to Waldenstroms macroglobinaemia if IgM expression is large enough: o Hyperviscous blood, high ESR (small thrombosis can = visual problems, VTE) 50% have t9/14 which leads to PAX-mediated p53 dysregulation IgM (surface and cytoplasmic) is what you look for in immunophenotyping DLBCL Aggressive disease that invades extranodal sites in 60% of cases De novo cases arise in follicles, transformations of MCL/SLL/follicular arise in other areas Pathology - cells have more cytoplasm, more nucleoli and more apoptotic bodies Immunophenotype and cytogenetics are varied because the disease is so heterogeneous Burkitts Endemic/ sporadic disease that responds well to chemo EBV immortalises cells and malaria stiomultes their proliferation in endemic forms. The subsequent 8/14 trasnlocation leads to emergence of the clone Pathology - starry sky (macrophages) Immunophenotype - CD10+, mib1/ki67+ve 5. T cell NHL Mycosis fungoides Cutaneous disease with nodular infiltration of skin May be limited to skin for years before dissemination Pathology - ‘pouches’ that contain malignant cells underneath the surface of the skin Anaplastic LCL Heterogenous group of nodal T lymphomas with a good prognosis Pathology - expansion of paracortex. Large cells Immunophenotype - CD30+ve, alk1+ve, EMA+ve Cytogenetics - t2/5 = NPM;Alk fusion product = altered growth receptor function ATLL Aggressive disease secondary to HTLV1 infection, presenting with LNpathy, skin rashes, organ dissemination and hypercalcaemia Virus activataes IL2 and CD25 via TAX as well as other genes involves in apoptosis (p16) CD25+ is the immunological hallmark 2.36 - FLOW CYTOMETRY (AGAIN!) Advantages of Flow cytometry Can identify and quantify a cell sample (qualitive and qwuantitaive) Multi-paramteric Can analyse a large number of cells (10e6) Principles of Flow Uses flourochrome conjugated monoclonal antibodies against known cellular markers o Usually CSM, but can be internal if cells are permalised A stream of cells is passed through a laser Cells sctter the light so that fluorochromes are excited to different energy levels; this change in energy is emitted as a light photon when it returns to its original energy level, and this can be measured by a light detector Detectors for different wavelengths of light match the light emitted to the antoibody it was matched to and hence the antigen presence Forward light scatter is an indicator of how large a cell is Sideways light scatter is an indicator of how granular the cell is/ how complex the nucleus is Applications of Flow Diagnosis of leukaemia, lymphoma, PNH, immunodeficiency, platelet disorders Monitoring MRD Measurement of absolute cell numbers (CD4 in HIV, CD34 after SCTs) Important markers Important Diagnostic Hallmarks APL - CD34-; HLADR -ve B-ALL - CD34+, CD10+, B markers + HCL - Cd11c +ve, CD103+ve SLVL - CD103-ve, CD123-ve MCL - cyclin D1 Myeloma - CD19-ve, CD56+ve, CD138 +ve, CD38+ve PNH- CD59 is lost (as with other GPi anchored CD markers) 2.37 - MOLECULAR GENETICS OF LYMPHOMAS 1. General features of lymphoma (think this covers both HL and NHL) EPIDEMIOLOGY : o Disease of men, the elderly, can be predisposed to by infections, genetics, enivormental mutagens, autoimmune diseases SYMPTOMS: o 1st symptoms may, but not always, emerge at the lymph nodes involved o Indolent lymphomas may present with b symptoms without overt/evident LN size change DIAGNOSIS: o LN biopsy, bloods, BM aspirate (to exclude metastases), XR, CT, PET o Staging depends on invovlement either side of the diaphragm and presence/absence of B symptoms CLASSIFICATION: o Hl/NHL depends of the presence of reed Sternberg cells o Diffuse NHLs are associated with complete loss of LN architecture, whereas follicular ones concur follicular expansion into other, still defined, areas o HLs are generally easier to treat 2. Ig rearrangement in lymphomas 85-90% of translocations underlying B lymphoma involve Ig genes: o 14q32 (IgH@) o 2p11 (Igk) o 22q11 (Iglamda) Ig genes are very active transcriptionally in B cells because they are key to function, hence genes brought under their influence following translocation become constitutively expressed o The partner gene doesn’t have to be downstream either, because a promoter region on IgH@ (switch mew?) can transcribe in both directions Ig genes give rise to lymphoma because of rearrangement AND somatic mutations Translocations lead to one of two outcomes: o Transcriptional dysregulation 8/14 burkitt = cmyc activation = proliferation, growth 14/18 follicular = bcl2 activation = anti-apoptosis Other cases involve BCL6 - this is implicated in lymphoma after it is subjected to a number of somatic mutations 11/18 MCL = cyclin d1 activation = unchecked proliferation o Fusion gene production T cell lymphomas involve TCR loci translocations HENCE most are diagnosed with FISH, PCR, karyoptying. New techniqwues include microarrays and array competitce genomic hydribisation (CGH) 3. Other mutations in lymphomas BCL10 - MALT (under influence of 14q32) MALT1 - MALT (under influence of 14q32) - believed to be due to nfkb activation PAX5 - waldenstroms (under influence of 14q32) Point/somatic mutations in c-myc and bcl6 C-myb translocations; ink mutations Tp53 deletions after 17q- or monosomy 17; often an acquired event in lymphoma; bad prognosis Epigenetic changes - methylation = gene inactivation 2.38 - THERAPY OF NHL 1. Prognostic factors in NHL; the Internation Prognostic Index Cure rate varies from 25-75% depending on these factors: Age >60 LDH>normal Performance status 2-4 Disease stage 3/4 more than one extranodal site IPI score 0-1 2 3 4-5 5 year survival 73% 51% 43% 26% 2. Therapeutic options in NHL Indolent b lymphomas usually have small cells. o The most common is follicular lymphoma. o Median survival is about 8 years. o 80-85% present with stage ¾ disease. o Watchful waiting is best until they present with progressive disease/transformation, watch for B symptoms or BM failure symptoms o Give them CHOP (cyclophos, doxo, vincristine, pred) o Those who relapse may need high dose chemo (LACE; lomustine, cytarabine, cyclo, etop) + autoSCT o Randomised data is needed to assess the efficancy of rituximab Aggressive lymphomas usually have large cells o the most common is DLBCL o CHOP +R is first line 2.39 - MANAGEMENT OF MDS (includes overview of whole disease because lecturer was good) 1. Clinical features of MDS D - heterogenous group of clonal disorders characterised by progressive cytopenia and qualitative abnormalities in myeloid cells, leading to ineffective haematopoiesis. It is now recognised as a cancer. 50% die because of cytopenia, 30% progress to AML. I - 5/100k in UK A - median = 67 S - M>F G A - unknown P Bone Marrow features: hypercellular bone marrow and peripheral (pan)cytopenia abnormal microenvironment due to ineffective erythropoiesis, increased TNFa production = apoptosis and an angiogenic response, CD4 lymphopenia and emergence of auto-reactive T cells Cellular features: o nuclear:cytoplasmic size asynchrony o disorganised chromatin and cytoplasm o loss of lobules in neutrophils and agranular cytoplasms C - anaemia may be the only presenting symptom 2. Prognosis of MDS + the IPSS 0 Blast % <5 Karyotype good Cytopenia 0-1 0.5 5-10 intermediate 2-3 1.0 1.5 11-20 2.0 >20 [AML] Poor Karyotypes: Good - normal, del5q, del 20q Intermediate - anything that isn’t good or bad Bad - complex or c7 abnoramlities Cytopenia; 1 point each for: Hb<10 Neutrophils <1.5e9 Plt <100e9 Prognostic risk Low Int-1 Int-2 High Score 0 0.5-1 1.5-2 >2.5 Prevalence 31% 39% 22% 8% Median survival 5.7y 3.5y 1.2y 0.4y Years AML 9.4 3.3 1.1 0.2 3. WHO Classification of MDS RA RARS - with only erythroid dysplasia o RA & RARS are the most indolent forms of MDS and account for the majority of paitents; very few MDS [patients present with worst prognostic subtypes o Mean survival is about 4-5 years RCMD - refractory cytopenia with multilineage dysplasia RCMD + ring sideroblasts RAEB 1 (5-9% blasts) & RAEB 2 (10-19% blasts) MDS-U (unclassified) 5q syndrome 5q syndrome Interstitial deletion between q31 and q33 = macrocytic anaemia (MCV usually normal is other cases of MDS) = thrombocytosis + increase in mononuclear megakaryocytes o Those with high Plt counts may have the JAK2 V617F mutation, which is also seen in other myeloproliferative diseases Presents is women, splenomegaly may be present Accounts for only 15% of patients with MDS 4. The use of EPO+GCSF in MDS Supportive care is employed in many patients because MDS is a disease of the elderly and its heterogenous nature makes it difficult to cure 80% of patients MDS patients are anaemia, 40% are trabnsufsion dependent Endogenous EPO varies greatly within patients and does not correlate to disease sub-type of transfusion dependence o Other factors such as ring sideroblasts, transfusion dependence, cytogenetics, seem to predict response EPO+GCSF seems to only prvoke a response in those who are less transfusion dependent o RA, RARS and RAEB1 o The response wears off after 2 years though, so it isn’t completely effective o Additionally, GCSF may contribute to progression to AML as a SFX o Current recommendations are giving a 6 week trial of EPO+GCSF in Ra/RAEB patients with low transfusion reqyuirement and a basal EPO of <200 5. The use of targeted therapy in MDS Farnesyl transferase inhibitors were designed to inhibit ras but only gave responses in 29% of patients Thalidomide achieves responses in 51% of patients (but you need high doses) o Anti-angiogenesis (anti-VEGF) - angiogenesis is important in tumour growth, vascularity and metastasis o TNFa synthesis inhibition o Immunomodulatory o Because of high dose requirement - SFX - somnolence, peripheral neuropathy, VTE Lenalidomide is really good for 5q- - removes transfusion dependence in 2/3 of patients o Anti-inflammtory, enchance t/nk cells, anti-angiogenic - pretty much returns bone marrow microenvironment to normal 6. The use of non-intensive chemo in MDS The idea behind immunosuppression is getting rid of the clonal t cells and letting the others grow o Antithymocyte globulin (ATG) is effective in hypoplastic MDS patients o Cyclosporin blocks IL2 production but is of limited benefit outside hypoplastic RA patients o Cytarabine & 5-aza-cytidine hypomethylate DNA (i.e. p15, which is hypermethylated in many high risk MDS cases) and gives a 49% response rate 7. The use of intensive chemo in MDS There is a reluctance to treat people with high dose chemo + SCT until they actually develop AML because these patients are already profoundly cytopenic and most cannot tolerate >2 chemo cycles FLAG/Ida is what is used now for high risk MDS because it has minimal toxicity and gives rapid haemoatopoietic recovery o Younger patients and those with favourable karyotypes have more favourable responses High dose chemo +AlloSCT is the only cure but most patients are elderly so you can’t give the full whack chemo dose because transplant related mortality increases with age o Less ability to deal with toxicity o Increased incidence and severity of GVHD o Increased non-malignant causes of death Predictors for outcome in AlloSCT o Older Age is poorer outcome o Morphology (RAEB onwards is poorer outcome; 3year survival 30%) o High risk cytogenetics is poorer outcome o Prolonged disease duration, marrow fibrosis, t-MDS are all poor outcome There is a huge difference in survival amongst MDS patients who have a sibling and a matchedstranger AlloSCT Hence, patients who are young enough and have a sibling donor should go for high dose chemo + alloSCT early in the disease course 2.40 - IMMUNE COMPLICATIONS IN CLL 1. Incidence of infections in CLL 50% patients have recurrent infections Incidence of infections increases with: o Age o Disease progression – hypogammaglobulinaemia, AI disease o Repeated therapies – neutropenia, AI disease?? Prevent infections with: o IVIG - useful for peventing bacterial infections o Fluconazole for candida (but this increases incidence of non-albicans candida infections) o septrin/ co-trimoxazole to prevent PCP o GCSF may improve neutropenia o Immunizations against strep pneumo, haemophilus, influenza 2. Hypogammaglobulinaemia (low IgG?) & impaired immunity in CLL Hypogammaglobulinaemia may be due to defective cell mediated immunity due to abnormally functioning T cells and thus dysregulated B cell function o Reduced Cd4:Cd8 ratio is seen o Leads to increased risk of encapsulated organism infection Skin shows decreased tuberculin response VZV- shingles o Related to disease progression Complement system is also defective in CLL - reduced opsoniosation of bacteria by C3b 3. Neutropenia in CLL Neutropenia = bacterial & fungal infections o Strep Pneumonia is the most common and severe o Staph Aureus, Haemophilus influenza, legionella and slamonella also common o Fungal - PCP, candida, aspergillus Mostly arises because of therapy, not disease o Steroids = defective chemotaxis + lymphopenia PCP, candida o Fludarabine (purine analogue) = lymphopenia + myelosuppression Strep pneumo, CMV/HSV/VZV, PCP, mycobacterium fortuitum o Anti-CD52 (alemtuzumab) Bacterial, CMV, PCP infections CMV reactivation is at highest risk when CD4<50 4. Tumours in CLL Skin cancer Kaposi Sarcoma (HHV8) 5. AI complications in CLL AIHA o Incidence = 4-40% o Due to polyclonal IgG autoantibodies production against RBCs secondary to immune dysregulation (not Ab production by the malignant cells) o = anaemia, jaundice, splenomegaly, reticulocytes, +ve coombs test o Treat with steroids, rituximab, may need transfusion Auto-Immune thrombocytopenic purpura o Incidence 1-2% o IgG antibodies against platelets + premature destruction by the spleen o Treat with steroids, IVIg Pure red cell aplasia o Incidence <1%, occurs early in disease o = anaemia, erythroid hypoplasia in BM o Treat with steroid and ciclosporin Risk factors for AI disease: o Disease stage, age, high WCC o Male o CD38, ZAP70, porr risk cytogenetics, beta2m 2.41 - HODGKIN LYMPHOMA 1. Clinical features of Hodgkin lymphoma D - any lymphoma with the presence of Reed-sternberg and mononuclear hodkin cells on morphology. Rarer than NHL and more likely to present with localised disease. I - rare 4-5/100k A - 2 peaks; late adolescence and >60 S/G/A/P C - (cervical) lymphadenopathy is usually the presenting feature. Hepatosplenomegaly may occur in advanced disease. B symptoms (fever may be episodic) are also present Investigations - Bloods; High WCC, anaemia, high ESR & LDH - LN aspirate/ biopsy is diagnostic; perhaps with CT guiding for central nodes 2. Classification of Hodgkin lymphoma 2 broad categories o Nodular, lymphocyte dominant HL - behaves more like a NHL o Classical HL Nodular sclerosis Mixed cellularity Lymphocyte rich Lymphocyte depleted Incidence Age Gender aetiology Affected organs Affected cell Relapse Immunophenotype Cytogenetics Nodular 5% Anyone 70%male Peripheral LNs Germinal B Can DLBCL CD20+, 45+, 79a+, 15-, 30-, 138BCL6+, SmIg weak BSAP+, Oct2 +, BOB1+ 3q27 translocations (BCL6) Classical 95% Normal 2 peaks equal Possibly EBV Mediastinal/cervical LNs Heterogeneous rare CD20-, 45-, 79a-, SmIg-, 15+, 60+,138+, IRF4/MUM1 + BSAP+, Oct2-, BOB1REL/ FAS mutations 3. Aetiology of HL Familal factors (HLA polymorphisms implicated in classical HL) EBV and HIV shows strong links in classical HL patients o EBV is present in reed-sternberg cells in 40-50% of patients o HL incidence increases 4x after glandular fever o HL incidence rises are CD4 count rises (i.e. after you start treating someone for HIV) ALPS (very rare) can predispose to nodular LDHL 4. Mechanisms of HL Constitutive activation of Nfkb = proliferation and survival of HL B cells o Defective Ikb may be involved in HL cases not secondary to infection In EBV related HL, LMP1 mimics Cd40 = nfkb activation and LMP2 confers proliferation and anti-apoptosis Impaired cell mediated immunity in HIV/old age means that reduced immunosurveillance is another problem in controlling proliferating b cells 5. Staging of HL Staging is based on o Examination o CXR mediastinal widening, hilar LNpathy o CT o PET (more useful for monitoring disease after follow up) Staging is 1,2,3,4 depending on structures involved either side of diaphragm (+A/B) 6. Treatment of HL Combo involved field radio and chemo (ABVD/BEACOPP) Use PET to monitor disease after 2 cycles ?Anti CD20 in nodular HL ?Anti CD30 in classical HL Treatment SFX = toxicity, malignancies, CVD 7. Prognosis of HL Median survival untreated in less than a year 5 year survival of early stage HL is now >90% Prognostic factors are: a. Disease stage b. Age c. Albumin d. Lymphocyte count e. LDH f. ESR 2.42 - MYELOMA BONE DISEASE 1. Bone disease in myeloma Is the most frequent presentation of MM; 70% of cases o 60% present with osteolytic lesions o 10% present with diffuse osteopenia o Very rarely patients present with increased bone formation; POEMS syndrome The consequences of increased bone resorption in MM are: o Pathological fractures (37%) o Osteoporosis o Hypercalcemia (9%) o Bone pain o Spinal cord compression (3%) 2. Recap of normal bone-cell functions Osteoblasts are derived from mesencymal stem cells. Osteoclasts come from the myeloid precursor Osteoblasts produce osteoid matrix, the main components of which are type 1 collagen and hydroxyapatite. o The matrix is calcified extracellularly o Osteoblasts are stimulated by growth factors eg IGF, EGF, BMP/TGFb, GPCR o The GF Wnt requires LRP5/6 as a cofactor to activate transcription. Sclerostin, a molecule produced by osteoclasts, prevents this interaction and thus inhibits osteoblast growth via this pathway. Osteoclasts resorp bone o RANKl is a key stimulator of osteoclasts. It is made by osteoblasts o OPG is a decoy RANKl receptor +ve osteoclasts -ve osteoclasts Humoral PTH, T4, VitD Cortisol, T cell [IL4,18,IFNg] Local IL6, RANKl, M-CSF, PDGF, IGFs OPG 3. Pathogenesis of bone disease in MM Myeloma cells stimulate osteoclasts directly via MIP1a, IL3, HGF Myeloma cells stimulate bone marrow stromal cells via adhesion o Stromal cells produce sclerostin, dickkopf1, activin A and other molecules that inhibit osteoblasts o Stromal cells display RANKl to stimulate osteoclasts Osteoclasts produce IL6 which stimulates plasma cells - vicious circle The RANKl/OPG ratio is usually increased in MM- it may have prognostic value Serum MIP1a, dickkopf1, activin A is also increased and may have prognostic value 4. Treatment of myeloma bone disease Prevent the first skeletal-related event/ prevent recurrence after a first event o Bisphosphonates - induce osteoclast apoptosis and inhibit migration into bones o The mechanism is by inhibition of FFP synthase o Zoledronic acid is the best one but needs to be given IV. Clodronate is second choice. o Side effects: Oral therapy - GI intolerance; ulcers in upto 1/3 patients IV - flu/fevers are common, renal disease and jaw osteonecrosis are rare o Current guidelines are tio give them for two years for all symptomatic px, have regular dental monitoring and then after 2 years its at the prescribing doctors discretion Palliate and control bone pain o Analgesia o Palliative radio 5. Other drugs in MM Proteasome inhibitors o Proteasomes degrade Ikb = free Nfkb = transcription o The end point of the RANKl pathway of osteoclast activation is Nfkb o Bortezomib bind to the chymotryptic site in the core of the proteasome to inhibit it o Bortezomib increases bone marrow density Monoclonal Antibodies o Denosumab (anti-RANKl) leads to osteoclast apoptosis and prevents skeletalrelated-events but increases risk of death compared to zoledronic acid o Anti-Dkk1 antibodies lead to bone formation in mice Novel anabolic agents eg BHq880, sotatercept 2.43 - MYELODYSPLASTIC SYNDROMES 1. Recap of clinical features of MDS D - heterogeneous haematological disorders characterised by ineffective clonal haematopoiesis, peripheral cytopenias and hypercellular BM. I A - 70-75years S G A - previous chemo/radio are risk factors P C - cytopenias = anaemia, thrombocytopenia, neutropenia 2. WHO Classification of MDS Name Refractory cytopenia with unilineage dysplasia Refractory anaemia with ring sideroblasts 5q- syndrome Refractory cytopenia with multilineage dysplasia Refractory anaemia with excess blasts 1 Refractory anaemia with excess blasts 2 unclassifiable Feature One of anaemia/neutropenia/ thrombocytopenia >15% ring sideroblasts Hypolobulated megaKcytes Pelger-huet anomaly %of patients 10 (usually anaemia) 5 5 20 5-9% blasts 10-19% blasts 20 20 10 Survival worsens and potential to transform into leukaemia increases as you move down the table Has features of the IPSS which were covered in a previous lecture [2.39] 3. Pathogenesis of MDS BM features: o Hypercellular o Dysplastic/megaloblastic erythropoiesis (RA) Ringed sideroblasts - formed when iron accumulates in mitochondria of developing erythroblasts. Identify with Prussian blue stain o Dysgranulopoiesis; hyporgranular neutrophils o Micromegakaryocytes o Increased blast number in RAEB Pathogenesis o Reduced proliferation and differentiation of erythroid progenitors o Excess presence of apoptosed progenitors High caspase 1/3 activity Escape from apoptosis and transformation to AML may be due to bcl2 expression seen in RAEB o VEGF is increased in MDS o Immune dysfunction in MDS: Autoantibody production, monoclonal gammopathy, hypo- or hypergammaglobulinaemia Presence of antinuclear antibodies, rheumatoid factor, anti-DNA antibodies, positive Coombs test Increased frequency of auto-immune disorders (~10%-15% of MDS patients): vasculitis, arthritis, pleuritis, pericarditis, myositis Decreased NK-cell activity, decreased antibody-dependent killing and diminished CD4 numbers T-cells inhibit MDS CFUE ; CD8+ cells inhibit CFU-GM 4. Treatment of MDS