AMS_PowerPoint_Haematopoietic_2
advertisement

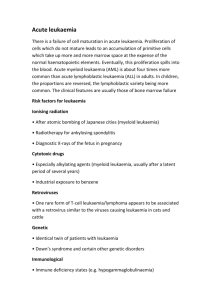
1 Pathogenesis: A reduction in the number of granulocytes in the blood (neutropenia) can be seen in a wide variety of conditions, including the effects of drugs, neoplasms and autoimmune conditions. 2. Congenital Neutropenia: Periodic or cyclic neutropenia is an autosomal dominant disorder with variable expression that begins in infancy and persists for decades. It is characterised by periodic neutropenia that develops approximately every 21 days and lasts approximately 2 to 3 days. It is thought to result from impaired feedback regulation of granulocyte production and release. 3. Acquired Neutropenia: Many cases of neutropenia are drug related. Chemotherapeutic drugs used in the treatment of cancer cause predictable dose-dependant suppression of bone marrow function. 4. Clinical Course: > Infection; < 250/uL. 1. 2 1. 2. 3. 4. 5. 6. Cause: Epstein Barr Virus Mode of Transmission: Oral contact with EBVcontaminated saliva. Pathogenesis: The virus initially penetrates the nasopharyngeal, and salivary epithelial cells. It then spreads to the underlying oropharyngeal lymphoid tissue , and more specifically to B lymphocytes. Incubation period: 4 to 8 weeks Clinical Course: > Fever; Enlarged Lymph Nodes; Severe Pharyngitis; > Leucocytes (of particular note lymphocytes) Common Manifestations: Hepatitis and splenomegaly 3 4 Leukaemia's are malignant neoplasms arising from the transformation of a single blood cell line derived from haematopoietic stem cells. 2. The leukaemia's are classified as acute and chronic lymphocytic or myelogenous leukaemia’s according to cell lineage. 3. Because leukemic cells are immature and poorly differentiated, they proliferate rapidly and have a long life span, they do not function normally, they interfere with the maturation of normal blood cells, and they circulate in the bloodstream, cross the blood brain barrier, and infiltrate many body organs. 1. 5 1. - - - - Acute Lymphocytic Leukaemia (ALL): Most common cancer in children and adults. ALL encompasses a group of neoplasms composed of precursor B or T lymphocytes referred to as lymphoblast's. Most cases of ALL are of pre-B cell origin. Approximately 90 percent of persons with ALL have numeric and structural changes in in the chromosomes of their leukaemic cells. Symptoms include fatigue resulting from anaemia, low grade fever, night sweats and weight loss, bleeding due to decreased platelet count and bone pain. Increases in uric acid crystallization and infection. 6 1. Acute Myeloid Leukaemia: - Diverse group of neoplasms affecting myeloid precursor cells in the bone marrow. - Associated with acquired genetic alterations that inhibit terminal myeloid differentiation. - Normal marrow elements are replaced by an accumulation of relatively undifferentiated blast cells with a resultant suppression of the remaining progenitor cells that leads to anaemia, neutropenia and thrombocytopenia. 7 1. - - Chronic Lymphocytic Leukaemia: Accounts for approximately one third of all leukaemia’s. Mainly a disorder of older persons. Manifests as a result of differences in immunoglobulin variable (V)- gene mutations, expression of cell surface CD markers and the presence of zeta-associated protein (ZAP70). Clinical Signs and Symptoms: progressive infiltration of the bone marrow and lymphoid tissues by neoplastic lymphocytes; lymphadenopathy, hepatosplenomegaly, fever; abdominal pain, weight loss, progressive anaemia and thrombocytopenia, rapid rise in lymphocyte count. 8 The lymphomas represent malignancies that arise in the peripheral lymphoid tissues. 2. Non-Hodgkin lymphomas represent a group of heterogeneous lymphocytic cancers that are multi-centric in origin and spread to various tissues throughout the body, including the bone marrow. 3. Hodgkin lymphoma is a group of cancers characterised by Reed-Sternberg cells that begins as a malignancy in a single lymph node and then spreads to contiguous lymph nodes. 4. Both types of lymphomas are characterised by manifestations related to uncontrolled lymph node and lymphoid tissue growth, bone marrow involvement, and constitutional symptoms (fever, fatigue, weight loss), related to rapid growth of abnormal lymphoid cells and tissues. 1. 9 1. Represent a diverse group of either B cell or t cell 2. 3. 4. 5. 6. neoplasms. Impairment of the immune system and infectious agents may play a role (EBV infection; HTLV-1; HIV; Acquired or Congenital immunodeficiencies; Helicobacter pylori). Origin: Lymph nodes (either B cells/T cells). B Cell Lymphoma: Burkitt Lymphoma T Cell Lymphoma: Anaplastic Large Cell Lymphoma Clinical Manifestations: Indolent or aggressive. 10 1. 2. 3. a) b) Specialised form of lymphoma that features the presence of an abnormal cell called a Reed-Sternberg cell. Bimodal Differs from NHL: HL arises in a single node or chain of nodes and spreads first to anatomically contiguous lymphoid tissues; whereas, NHL frequently originates at extranodal sites and spreads in an unpredictable fashion. HL has distinctive morphological features i.e. Reed Sternberg Cells. 11 Porth, C.M. 2011. Essentials of Pathophysiology, 3rd edn. 12 Nodular lymphocyte-predominant Hodgkin Lymphoma 2. Classical Hodgkin Lymphoma 3. Clinical manifestations: most persons with Hodgkin lymphoma present with painless enlargement of a single node or group of nodes. The initial lymph node involvement typically is above the level of the diaphragm . There may be complaints of chest discomfort with cough or dyspnoea. 4. Additional Symptoms that suggest Hodgkin Lymphoma include fevers, chills, night sweats and weight loss. 1. 13 14 Is a B cell malignancy of terminally differentiated plasma cells. 2. The cause of multiple myeloma is unknown. Risk factors are thought to include chronic immune stimulation, autoimmune disorders, exposure to ionising radiation and occupational exposure to pesticides and herbicides. 3. Characterised by proliferation of malignant plasma cells in the bone marrow and osteolytic bone lesions throughout the skeletal system. 4. Main sites involved in multiple myeloma are the bones and bone marrow. 1. 15 Porth, C.M. 2011. Essentials of Pathophysiology, 3rd edn. 16 1. 2. 3. 4. 5. The white blood cells include the ______________, monocytes/macrophages and lymphocytes. There are two types of acute Leukaemia: acute ____________ and acute ________________. Neutrophils are very important as a first line of defence against viral/bacterial infection. Explain what a neutrophil does and the condition that results from a deficiency of neutrophils. Definitive marker for Hodgkin Lymphoma _____________________. What are the two major differences between Hodgkin Lymphoma and NHL. 17 1. Caused by defects associated with platelets, coagulation factors and vessel integrity. 2. Disorders of platelet plug formation include a decrease in platelet numbers due to inadequate platelet production (bone marrow dysfunction), excess platelet destruction (thrombocytopenia), abnormal platelet function (thrombocytopathia) or defects in von Willebrand factor. 18 Refers to a decrease in the number of circulating platelets to a level less than 100,000/uL. 2. The greater the decrease in the platelet count, the greater the bleeding. 3. Major causes: decreased platelet production (loss of bone marrow function), decreased platelet survival (caused by a variety of immune and non-immune mechanisms), splenic sequestration (excessive pooling of platelets in the spleen) and dilution (massive blood or plasma transfusions). 4. Immune Thrombocytopenia Purpura (ITP) . ITP includes a history of bruising, bleeding from the gums, epistaxis, melena and abnormal menstrual bleeding in those with moderately reduced platelet counts. 1. 19 Porth, C.M. 2011. Essentials of Pathophysiology, 3rd edn. 20 1. Blood coagulation defects can result from deficiencies or impaired function of one or more of the clotting factors. 2. Haemophilia A: is an X-linked recessive disorder that primarily affects males. 3. Haemophilia A: can arise as a result of a new mutation in the factor VIII gene. 4. Characteristically, bleeding occurs in soft tissues, the GIT, hip, knee, elbow and ankle joints. 21 1. Describe the manifestations of thrombocytopenia. 2. _______________ from mucous membranes of the nose, mouth, gastrointestinal tract, and uterine cavity is characteristic of platelet bleeding disorders. 3. A reduction in platelet number is referred to as _______________. 4. Haemophilia A is an ________________ recessive disorder that primarily affects males. 5. A common clinical manifestation of essential _______________ is thrombosis and haemorrhage. 22 23 Porth, C.M. 2011. Essentials of Pathophysiology, 3rd edn. 24 1. The function of red blood cells, facilitated by the iron-containing haemoglobin molecule, is to transport oxygen from lungs to the tissues. 2. The production of red blood cells, which is regulated by erythropoietin, occurs in the bone marrow and requires iron, vitamin B12 and folate. 3. The red blood cell, which has a life span of approximately 120 days, is broken down in the spleen. 25 Porth, C.M. 2011. Essentials of Pathophysiology, 3rd edn. 26 Deficiency of red cells or haemoglobin, results from excessive loss (blood loss anaemia), increased destruction (haemolytic anaemia), or impaired production of red blood cells (iron deficiency, megaloblastic, and aplastic anaemia. 2. Blood loss anaemia is characterised by loss of ironcontaining red blood cells from the body; haemolytic anaemia involves destruction of red blood cells in the body with iron being retained in the body. 3. Manifestations of anaemia are caused by the decreased presence of haemoglobin in the blood, tissue hypoxia due to deficient oxygen transport and recruitment of compensatory mechanisms designed to increase oxygen delivery to the tissues. 1. 27