File - Study Guides
advertisement
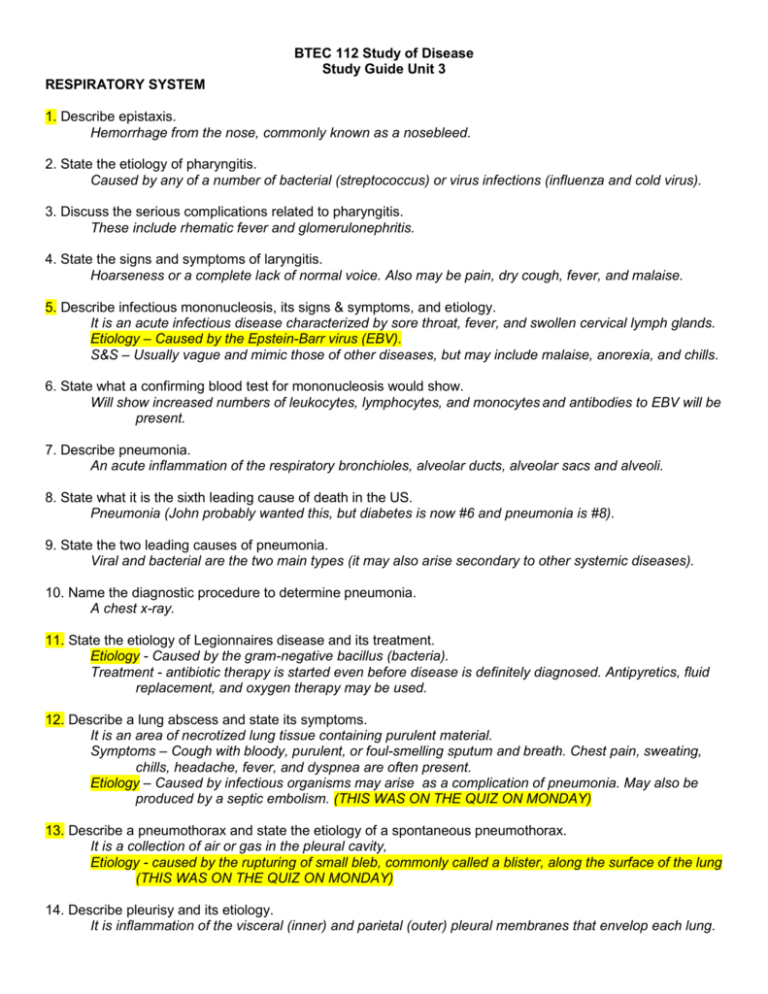
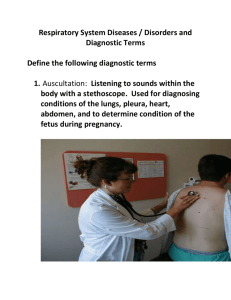
BTEC 112 Study of Disease Study Guide Unit 3 RESPIRATORY SYSTEM 1. Describe epistaxis. Hemorrhage from the nose, commonly known as a nosebleed. 2. State the etiology of pharyngitis. Caused by any of a number of bacterial (streptococcus) or virus infections (influenza and cold virus). 3. Discuss the serious complications related to pharyngitis. These include rhematic fever and glomerulonephritis. 4. State the signs and symptoms of laryngitis. Hoarseness or a complete lack of normal voice. Also may be pain, dry cough, fever, and malaise. 5. Describe infectious mononucleosis, its signs & symptoms, and etiology. It is an acute infectious disease characterized by sore throat, fever, and swollen cervical lymph glands. Etiology – Caused by the Epstein-Barr virus (EBV). S&S – Usually vague and mimic those of other diseases, but may include malaise, anorexia, and chills. 6. State what a confirming blood test for mononucleosis would show. Will show increased numbers of leukocytes, lymphocytes, and monocytes and antibodies to EBV will be present. 7. Describe pneumonia. An acute inflammation of the respiratory bronchioles, alveolar ducts, alveolar sacs and alveoli. 8. State what it is the sixth leading cause of death in the US. Pneumonia (John probably wanted this, but diabetes is now #6 and pneumonia is #8). 9. State the two leading causes of pneumonia. Viral and bacterial are the two main types (it may also arise secondary to other systemic diseases). 10. Name the diagnostic procedure to determine pneumonia. A chest x-ray. 11. State the etiology of Legionnaires disease and its treatment. Etiology - Caused by the gram-negative bacillus (bacteria). Treatment - antibiotic therapy is started even before disease is definitely diagnosed. Antipyretics, fluid replacement, and oxygen therapy may be used. 12. Describe a lung abscess and state its symptoms. It is an area of necrotized lung tissue containing purulent material. Symptoms – Cough with bloody, purulent, or foul-smelling sputum and breath. Chest pain, sweating, chills, headache, fever, and dyspnea are often present. Etiology – Caused by infectious organisms may arise as a complication of pneumonia. May also be produced by a septic embolism. (THIS WAS ON THE QUIZ ON MONDAY) 13. Describe a pneumothorax and state the etiology of a spontaneous pneumothorax. It is a collection of air or gas in the pleural cavity, Etiology - caused by the rupturing of small bleb, commonly called a blister, along the surface of the lung (THIS WAS ON THE QUIZ ON MONDAY) 14. Describe pleurisy and its etiology. It is inflammation of the visceral (inner) and parietal (outer) pleural membranes that envelop each lung. Etiology – Caused by infection of the pleura by bacteria or viruses. 15. Describe chronic obstructive pulmonary disease and state the diseases that commonly lead to COPD. A group of pulmonary diseases characterized by the inability to get air into or out of the lungs (to ventilate). Chronic bronchitis (blue bloaters), emphysema (pink puffers) commonly lead to COPD. 16. State how COPD can be treated and how lost pulmonary function can be restored and the disease cured. Bronchodilator medication, mycolytics, antibiotics to avoid respiratory tract infections, and oxygen therapy. There is no cure and pulmonary functions cannot be restored. 17. State the etiology of chronic bronchitis. Smoking, prolonged exposure to polluted air, respiratory infections, and allergies. 18. Describe emphysema and its signs & symptoms associated with the disease. Permanent enlargement of the air spaces beyond the terminal bronchioles resulting from destruction of alveolar walls. S & S – dyspnea, tachypnea, wheezing and coughing. 19. Describe tuberculosis, etiology and the diagnostic procedures used to detect the disease. Is a slowly developing bacterial lung infection characterized by progressive necrosis of lung tissue. Etiology – Caused by mycobacterium tuberculosis. Diagnostic Procedures – Thorough, physical exam, chest x-ray, and positive tuberculin test. 20. Describe pneumoconiosis. Is a disease of the respiratory tract caused by inhaling inorganic dust (etiology) particles over a prolonged period. It is an occupational disorder. 21. Discuss pulmonary edema and its etiology. It is a diffuse extravascular accumulation of fluid in the pulmonary tissues and air spaces. Etiology – Most commonly represents the projection of cardiac disease processes such as atherosclerosis, hypertension, or valvular disease. 22. Discuss cor pulmonale. Hypertrophy and failure of the right ventricle of the heart. 23. Compare and contrast respiratory acidosis and alkalosis. Respiratory Acidosis (Hypocapnia) Excessive acidity (CO2 too high) Impairment of ventilation or excessive CO2 in the air Weakness, shallow respiration, confusion, muscle tremors, and tachycardia Treat the cause Respiratory Alkalosis (Hypercapnia) Excessive alkalinity (CO2 too low) Acute or chronic hyperventilation numbness or tingling of extremities, light headedness, muscle spasms, periods of apnea Treat cause: acute – breath into bag, give sedative 24. Describe the treatment and prognosis of lung cancer. Involves a combination of surgery, radiation therapy, and chemotherapy because it metastasizes to other tissues by the time it is diagnosed. Overall survival rate has changed little during the past 30 years CARDIOVASCULAR SYSTEM 1. Define the following terms: Bradycardia – abnormally slow heart beat Bruit – abnormal noise of venous or arterial origin heard during auscultation Diuretic – medication that increases urine excretion Effusion – seeping of fluid into a body cavity or part Embolus – blood clot or undissolved mass (piece of tissue, fat globule, or air bubble) carried through the circulatory vessels by the blood or lymph flow Hypoxia – deficiency of oxygen Lumen – space within an artery, vein, intestine, or other tubular structure Orthopnea – respiratory condition in which there is discomfort in breathing in any but erect standing or sitting positions Parenteral – any route of administration not involving the gastrointestinal tract Pitting edema – form of tissue swelling beneath the skin that, when pressed firmly with a finger, will maintain the indentation produced by the finger for a few minutes. Syncope – transient loss of consciousness due to inadequate blood flow to the brain. Diastolic pressure – lowest arterial pressure reached during any ventricular cycle (140/70) Systolic pressure – period of maximum arterial blood pressure (140/70) Vasodilator – a drug that expands the walls of the blood vessels, improving blood flow and resulting in lower blood pressure Vegetation – an abnormal growth of tissue around a valve, composed of blood platelets, bacteria, and a protein involved in clotting 2. State what the P, QRS, and T waves represent. P wave – the first wave of the electrocardiogram – it represents the spread of electrical impulse through the arterial musculature. QRS complex – the most important complex in the electrocardiogram, it represents the spread of the electrical impulse through the ventricular muscle. T wave – it represents the period of recovery for the ventricles. 3. State what is meant by blood pressure. It is the measure of contraction (systole) and relaxation (systole) of the heart number. (150...systole/80...diastole) 4. State the approximate number of heart beats per minute for a normal adult. 60 – 100 beat per minute (bpm) 5. State what is considered average blood pressure and what is considered high blood pressure. Average blood pressure – 120/80 High blood pressure – 140/90 6. Describe the relationship of rheumatic fever and rheumatic heart disease and its etiology. Rheumatic fever – usually strikes children and adolescents from 5 to 15 years of age, although it may occur at other ages. It affects the joints, heart, central nervous system, skin, and other body tissues. Rheumatic heart disease – When the inflammation occurs in the heart (acute carditis) the valves of the heart may be permanently scarred, maybe causing fatal heart failure years later. Etiology – Fever is a hypersensitivity to a group A infection by hemolytic streptococci. The antibodies manufactured to combat the streptococci react to produce lesions at specific site, especially in the heart and joints, which causes the rheumatic heart disease.(THIS WAS ON THE QUIZ MONDAY) CONTINUED..... 7. Describe pericarditis and its etiology. Pericarditis is an inflammation or the pericardium, the saclike membrane that surrounds and protects the heart muscle. Etiolgy - usually caused by bacterial, fungal, or viral infection of the pericardium. The disease may also be caused by neoplasms metastasizing from other organs, rheumatic fever, uremia or coronary thrombosis. Trauma or any injury that causes blood leak into the pericardium sac may also incite pericarditis. Classic symptom – pleuritic pain that increases with inspiration 8. Describe endocarditis, its etiology and state what type of growths form in the heart and around valves. Endocarditis , also known as infective or bacterial endocarditis, is inflammation of the membrane lining the valves and chambers of the heart. Etiology most common cause is infection from strep bacterial. Can also be caused by rheumatic fever, SLE, seen with IV drug abusers. Growths form called vegetation form around the heart and valves. 9. How are murmurs graded? They are graded by intensity from I to VI 10. Differentiate between valvular insufficiency and valvular stenosis. In both cases, the result is an enlarged left atrium. Valvular insufficiency – when blood from the left ventricle flows back into the left atrium. Valvular stenosis – blood flow is obstructed from the left atrium to the left ventricle. 11. State the treatment of choice for mitral insufficiency or stenosis. The treatment of choice is surgical excision of a heart valve and valve reconstruction or valve replacement with an artificial valve. 12. Describe essential hypertention. It is persistently elevated blood pressure that develops without apparent cause. 13. Describe angina pectoris, its etiology and classic symptoms. It is chest pain resulting from ischemia to a part of the myocardium. Etiology – Issues with blood supply and demand. The classic symptoms are burning, squeezing, and tightness in the chest; they may radiate to the neck and left arm and shoulder blade, generally after exertion. 14. State the medical treatment for angina pectoris. Treatment is nitroglycerin preparations taken either sublingually or applied topically. If coronary disease that causes this does not respond to treatment, it may require a surgical procedure. 15. Describe a myocardial infarction (MI) and its classic symptom. It is a life-threatening condition caused by the occlusion of one or more coronary arteries and the subsequent necrosis of a section of the heart muscle tissue served by those arteries. Classic symptom is crushing chest pain that may radiate to the left arm, neck and jaw. The pain may be similar to angina pain but usually is severe and is not relieved by the same measures. 16. Name diagnostic procedures used to diagnose myocardial infarction. Medical history revealing CAD (coronary artery disease) and episodes of chest pain will help the diagnosis. Electrocardiography (EKG) and echocardiogram Blood tests for elevated cardiac enzyme levels (CPK & CPK-MB) over a 72-hour period. 17. Describe congestive heart failure and state the symptoms related to left and right ventricular failure. It is a condition in which the pumping ability of the heart is progressively impaired to the point that it no longer meets bodily needs. Symptoms of left ventricular failure are pulmonary edema, dyspnea, and fatigue. Symptoms of right ventricular failure are distended neck veins, enlarged liver and spleen, ankle edema...systemic. JOHN ELUDED THAT THESE SYMPTOMS MIGHT BE ON THE TEST 18. State what is meant by cardiac arrest. It is the sudden, unexpected interruption of heart function. 19. Describe an aneurysm and name the three types. It is a local dilation of an artery or chamber of the heart due to weakening of its walls. Aneurysms may be sacculated (shaped like a sac), fusiform (spindle-shaped enlargement), or dissecting (the layers of the vessel wall are separated) 20. Describe arteriosclerosis and atherosclerosis and state the diagnostic procedure to diagnose. Arteriosclerosis is widespread thickening of the walls of small arteries an arterioles with a resulting less of elasticity. Artherosclerosis is a type of arteriosclerosis which is a condition characterized by the accumulation of yellowish plaques of cholesterol, lipids, and cellular debris on the inner layers of the walls of large and medium-sized arteries Diagnostic procedure – usually diagnosed during a routine physical exam (x-rays, arteriograms, blood pressure measurements and labs test) 21. Describe thrombophlebitis. Thrombophlebitis is inflammation of a vein in conjunction with the formation of a clot from the streaming blood constituents. 22. Describe the etiology of the following anemias: Iron deficiency anemia – lack of iron for formation of hemoglobin, hemorrhage Pernicious anemia – lack of protein that allows stomach to absorb vitamin B12 Sickle cell anemia – hereditary, abnormal erythrocytes are formed that don’t carry oxygen well. Folic acid deficiency anemia – inadequate intake of folic acid (B complex vitamin) Aplastic anemia – unknown causes include exposure to toxins and the hepatitis virus. It is an insufficient or total absent erythrocytes production 23. Describe polycythemia vera and state the primary treatment. It is a chronic blood disorder characterized by increased numbers of red blood cells, leukocytes, thrombocytes, and increased hemoglobin concentration. More common in late middle-aged men Primary treatment – phlebotomy treatment (blood letting) to reduce the hematocrit to the normal range ***24. Describe and differentiate acute myeloblastic leukemia, acute lymphoblastic leukemia, chronic myelocytic leukemia and chronic lymphocytic leukemia. Myeloblastic leukemia – by the hypoproliferation of abnormal, immature white blood cells called blasts Acute lymphoblastic leukemia – abnormal growth of lymphocytes precursors called lymphoblasts Chronic myelocytic leukemia – proliferation of abnormal white cell cursors called granulocytes in the bone marrow Chronic lymphocytic leukemia – accumulation of immature, immunologically ineffective B lymphocytes NOT SURE WHAT TO USE TO DIFFERENTIATE 25. Contrast Hodgkins disease and lymphosarcoma (non-Hodgkins lymphoma). Hodgkins disease Usual presenting symptoms (enlarged, firm, non-tender, painless regional lymph nodes) Neoplastic malignancy of the lymphatic system Labs are used to find the disease Treatment ranges from combination of chemotherapy, followed by radiation to bone marrow cell transplant Lymphosarcoma (non-Hodgkins lymphoma) Usually does not have presenting symptoms (asymptomatic) Group of malignant diseases of the lymphatic system Biopsy of nodes or bone marrow are used to find it Treatment ranges from radiation or the combination of chemotherapy and radiation to bone marrow transplant for those younger than 60 26. State how the definitive diagnosis can be made for Hodgkins disease. Definitive diagnosis is established by identifying the presence of Reed-Sternberg cells in lymphatic tissue. THE ANSWERS THAT ARE HIGHLIGHTED ARE THE QUESTIONS THAT JOHN ASKS BEFORE CLASS AND ALSO SOME ARE NOTED THAT WERE ON THE QUIZ MONDAY NIGHT THE QUESTION THAT WERE ON THE PRESENTATIONS ARE: Lung cancer presentation: WHERE DOES LUNG CANCER METASTASIZE TO? Adrenal glands, liver, brain and bone. Heart disease presentation: WHAT IS THE #1 CAUSE OF DEATH IN WOMEN BESIDES CANCER? Heart disease Asthma presentation: INFLAMMATION (I guess of the bronchioles, I wasn’t sure what she said) CAUSES ASTHMA. True/False? True