Acute Low Back Pain Assessment
advertisement

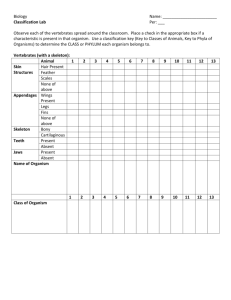
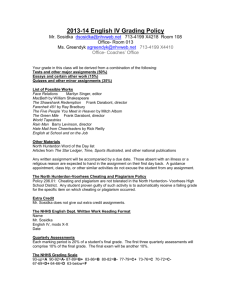
GP assessment for Acute Low Back Pain with radicular symptoms (please use in conjunction with MSK referral if patient needs referring to MSK) Patient Name: DOB: NHS Number: History of Present Condition (Including timeframes, nature of pain and onset): Relevant Past Medical History (e.g. previous cancer or serious illness/infection): Key Questions (essential to ask): Symptoms indicative of Cauda Equina Syndrome: Urinary incontinence/retention present on day of assessment Timescale: Yes No Faecal incontinence present on day of assessment Timescale: Yes No Altered sensation in saddle area present on day of assessment Timescale: Yes No Patients who report any of the above which are present on the day of attendance and are less than 3 months in duration should be immediately referred to the Emergency Department. Isolated constipation would not be an indication for an emergency MRI since this is a common symptom with back pain and is often related to codeine related products. Symptoms indicative of a potential Cauda Equina Syndrome/more serious neurological cause - Requiring urgent medical screening assessments +/- MRI before considering referral to MSK Patients who present with: Significant motor weakness e.g. Isolated foot drop Progressive neurological deficit in lower extremities Bilateral true sciatica Spinal pain/Sciatica with urological symptoms, e.g. stress incontinence, bladder frequency, urgency. A report of any of the following but not present on the day of attendance or are greater than 3 months in duration. o Saddle area numbness, o Urinary incontinence/retention o Faecal incontinence Sexual dysfunction Paresis (gait disturbance) (Adapted from the Cauda Equina pathway developed by the MSK service) 1 Neurological assessment, see videofor guidance. Ensure sufficient analgesia for accurate assessment, severe pain may need strong analgesia for rapid relief to enable assessment. Please see Analgesia Ladder in the ‘Pathway for patients presenting with new on-set motor loss in the presence of acute low back and radicular pain’ in RSS. Assessment Right Lower Limb Left Lower Limb guidance Ankle Plantar Patient asked to Achieved Achieved Flexion stand on one leg Not achieved Not achieved (L5/S1) and heel raise (with support) Ankle Patient lying on Normal Normal Dorsiflexion back or sitting on Reduced Reduced (L4/L5) edge of plinth Absent Absent Hallux Patient lying on Normal Normal Dorsiflexion back or sitting on Reduced Reduced (L5) plinth Absent Absent Knee Patient sitting on Normal Normal extension edge of plinth Reduced Reduced (L2-L4) Absent Absent Knee Flexion Patient sitting on Normal Normal (L5-S2) edge of plinth Reduced Reduced Absent Absent Hip Flexion Patient sitting on Normal Normal (L2) edge of plinth Reduced Reduced Absent Absent Sensation Pin prick test Normal Normal across lower leg Reduced Reduced dermatomes (see If reduced state If reduced state which figure below) which dermatome(s)3: dermatome(s)3: Ankle Reflex (S1) Babinski Response1 Knee Reflex (L3/L4) Patient in lying or sitting Consider Jendrassik Manoeuvre1 to aid assessment Patient in lying or sitting Present Reduced Absent Brisk Present Reduced Absent Brisk Present Absent Present Absent Patient in lying or sitting Consider Jendrassik Manoeuvre2 to validate findings Present Reduced Absent Brisk Present Reduced Absent Brisk 1When the Babinski response is present in an adult, it is often a sign of a brain or nervous system disorder. 2Jendrassik Manoeuvre is a distraction technique used to overcome the voluntary suppression of reflexes. The patient hooks the flexed fingers of the two hands together and forcibly tries to pull them apart; while this tension is being exerted the lower extremity reflexes are tested. 2 3The ‘evidence based’ dermatome map representing the most consistent tactile dermatomal areas for each spinal dorsal nerve root found in most individuals, based on the best available evidence. The dermatomal areas shown are not autonomous zones of cutaneous sensory innervation, except across the midline where overlap is minimal, adjacent dermatomes overlap to a large and variable extent. Blank regions indicate areas of major variability and overlap. S3, S4 and S5 supply the perineum but are not shown separately (Keegan and Garrett, 1948). Note consecutive dermatomes shown in buff or blue for clarity. From Apok, Gurusinghe, Mitchell and Elmsley (2011). Neurological Sign. Dermatomes and Dogma. Practical Neurology. 11:100-105. 3