Genetic_Disorders
advertisement

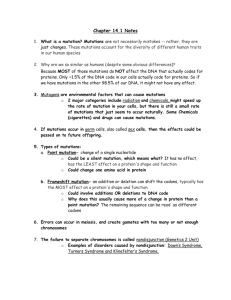
Genetic Disorders. Peds. Froberg. Katelyn Rogers. 03.22.10. 1. Learn the basic characteristics of cytogenetic, Mendelian and nonclassical inherited disorders Genetic Disorders: Method of Study •Classical genetics: requires knowledge of gene product to ID gene •Reverse genetics: protein unknown, use marker linkage to locate gene of interest Disorders •Chromosomal: # or structure, ex. trisomy 21 Good for cytogenetic ID •Mutant genes of large effect: Mendelian disorders (SCD), often requires molecular techniques •Multifactorial: polygenetic + environment (DM, HTN, CHD) Less amenable to genetic studies Cytogenetics •Cytogentic disorders identified through karyotyping •Karyotyping: visual image of chromosomes –NL karyotype 46 xx (xy) –22 homologous pairs + sex chr. •Method: –Cell culture (usually peripheral blood lymphocytes) –Arrest in metaphase (colchicine) –Stain G banding (Giemsa stain) –Light and dark bands, sort by size –Banding pattern –Centromere location: •metacentric: middle •submetacentric: off-center •acrocentric: near end •telocentric: not in humans •Limitations: Requires viable cells, visible changes (4 mil bp) •Advantages: Good for aneuploidy, large structural changes, del, t, i Examples: •47, xy, +21 (Trisomy 21 in male) •46, xx, del 5q•46, xy, t(9;22) (Philadelphia Chr in male) Mutations •Definition: heritable alteration in genome •Types: –Substitution: point mutation –Insertion: alters reading frame –Deletion: alters reading frame, i.e., frameshift •Consequences: –Codon mutations: •Missense: one AA for another –Ex.: CTC to CAC, glu to val in SCD (sickle cell dx) •Nonsense: stop; CAG to UAG = stop –Ex: B thal –Noncoding sequence: •Promoter or enhancer: decreased or no transcription •Introns: defective splicing, most common cause B-thal Cytogenetic Disorders •50% of early abortions, 5% stillbirths, 0.5-1% live births •Aneuploid = < 46 > –Secondary meiotic nondisjunction or anaphase lag –Monosomy (autosomal usually fatal) and trisomy (some viable) •Mosaicism = 2 or more cell lines in genome –Secondary early mitotic errors –Most common with sex chr. and Down syndrome •Chromosome breakage syndromes –Autosomal recessive –Have increased risk of CA –Multi-organ system changes: •Fanconi anemia: developmental problems, aplastic anemia, myelodysplasia, leukemia (they may get breast Ca and others) •Bloom syndrome: short stature, photosensitivity, risk cancer Rates vary greatly. Common: anencephaly, spina bifida, hypospadias, cleft lip and palate. Look at diffc in number and large structural malformations. Ultimately results in abbreviated product. 1 •Ataxia-telangectasia: neurodegenerative disorder, risk ALL & lymphoma •Rearrangements: –Reciprocal translocation: usually compatible with life, but associated with CA or abnl offspring (during metaphase they cannot line up correctly). –Robertsonian translocations: centric fusion of acrocentric chr. (rRNA from p of 13, 14, 15, 21, 22), lose part of p, abnl offspring (can’t line up correctly during metaphase) –Isochromosome: one arm lost, other duplicated & fused to centromere, so two p or two q (iXq) –Ring: deletion at both ends & fusion (2 breaks) –Inversions: compatible with NL development (few assc w CA) •Trisomy 21 (Down Syndrome): most common chr disorder, causes MR –Incidence ~1/800; 95% extra chr., 4% Robertsonian trans (familial), 1% mosaics (milder MR) –Correlated with maternal age: incidence <20 ~1/1550, >45 ~1/25. Due to maternal meiotic non-disjct in 95% –CSx: •flat face, oblique palpebral fissures, epicanthal folds, severe MR [ IQ 25-50 in 80% ], congenital heart disease (40%), ALL & AML ~10-20x risk, Alzheimer Disease at ~40, abnl immune response (lung infections & thyroid disorders) •80% survive >30 years P portions lost in Robertsonian. Isochrom is similar, linkage of p or qs together. Origins & examples of triploidy, trisomy & monosomy. A. Both maternal & paternal origins. Trisomies are fairly common. Can also be mosaic with subtle features of trisomy 21. 18 (Edward Syndrome): 1/8000 births, overlapping fingers, MR, low set ears, heart defects 13 (Patau syndrome): 1/6000, heart defects, polydactyly, cleft lip & palate, microphthalmia, MR Know that 18 & 13 do exist, but they do have similar phenotypes so you don’t need to distinguish. Nondisjunction. Edwards- overlapping digits, rocker bottom feet. Low set ears. Most common trisomies. MS, CV, renal, feet anomalies. There can 2 be a variety of karyotypes Don’t need to distinguish, just know characteristics. Trisomy 13 Features Trisomy 13: Polydactyl Trisomy 13: Facies Trisomy 18 Cleft lip,plate. Abnl hair, extradigits. Underdevpd chin, low set ears Abnl feet, ears, micrognathia, etc. •Cri du chat (5p- syndrome): –Severe MR –Microcephaly –Round face –Some survive to adults •Sex chromosome disorders: –More common than autosomal, better tolerated because of lyonization (inactivation of X, protective) & lack of genetic material of Y chr: lyonization (16th day embryonic life, Xist gene, secondary methylation). •subtle/chronic problems sexual development & fertility •often 1st recognized at puberty •more Xs ~ more likely MR (so lyonization is very impt) •Klinefelter Syndrome: Male hypogonadism; 1 or more Ys & 2 or more Xs –82% = 47, XXY, ~50% from 1st meiotic paternal non-disjct, 15% mosaics, incidence 1/850 live male births –Principal cause male infertility –Testes: tubular atrophy, prominent Leydig cells Face is round, ears are low. •Turner Syndrome: monosomy X, hypogonadism in phenotypic female –45, X (57%) but only 1% survive to birth •del Xp, i (Xq), or partial del of Xp or Xq *so variable phenotypes –CSx: edema in infancy in most severely affected = cystic hygroma (massively dilated lymphatics of neck), congenital HD esp. coarctation of aorta –Later: #1 cause primary amenorrhea, short stature, webbed neck, broad chest, widely spaced nipples –Streak ovaries secondary to accelerated loss of oocytes by 2 years -Nothing wrong with intelligence, mostly a psychosocial px Cystic hygroma in female stillborn fetus. Top: cartoon of Triploidy Note features of Turner Synd Edema in hand in newborn w/ Turner Synd 3 2. Be able to distinguish features of autosomal dominant, autosomal recessive and X-linked genetic disorders Classical Genetic Disorders (Mendelian) •Expressed mutations in single genes of large effect (sickle cell anemia) –Pleiotropism: multiple end effects (several organ systems altered) –Genetic heterogeneity: same effect by mutations at several genetic loci Transmission Patterns: Autosomal dominant Autosomal recessive X-linked –Manifested in heterozygous state –Single largest category Mendelian disorders –All sex-linked are X-linked –Affects males & females –Parents not affected –Most recessive –Affected X unaffected = 50% transmission –Siblings 1 in 4 –Male is hemizygous for X so expressed in –Some due to new mutations –Expression more uniform males –Clinical features modified by variable –Penetrance usually complete –Sons of affected male not affected expressivity (seen in all with gene, but –Onset early in life, new mutations –Daughters carriers expressed differently) & reduced penetrance undetected –Sons of heterozygous female have 1 in 2 (i.e., 50% of those with gene express trait) –Enzymes involved chance –Age of onset may be delayed: Huntington Dx –Heterozygote has 1/2 nl & 1/2 abnl: –Female may be affected because of skewed –Often structural protein or transport •inborn errors of metabolism lyonization protein: hereditary spherocytosis, Marfan •CF, SCD, PKU, a1-antitrypsin deficiency, most –Usually partial expression (G6PD def.) syndrome, familial hypercholesterolemia, NF, storage diseases, Ehlers-Danlos –Examples: DMD, hemophilia, Wiscott& tuberous sclerosis Aldrich, & chronic granulomatous disease Biochemical Basis of Mendelian Disorders •Direct effect on protein or indirect–consequences: accumulation of substrate or abnl product •Enzyme defects: –Decrease end-product: albinos - no melanin secondary to deficiency of tyrosinase –Increased substrate: phenylalinine-PKU –Failure to inactivate toxic substrate: a1-antitrypsin deficiency •Receptor or transport defect: Failure to cross cell membrane (familial hypercholesterolemia) •Structural protein defect: Affects function (DMD, SCD) •Adverse drug reactions: Oxidative injury (G6PD def) Specific Disorders •Marfan Syndrome: connective tissue disorder, 70-85% autosomal dominant, variable expression –Marfanoid appearance: tall, long fingers, lax joints, dolicocephalic (face like Lassie-elongated), frontal bossing, scoliosis, kyphosis, ectopia lentis, aortic cystic medial degeneration (dissection cause of death in 30-40%) “Abe Lincoln Phenotype”. –Cause: defective fibrillin (extracellular matrix protein for elastin, mapped to 15q21.1)multiple tissues & bone deformations. Aorta: Cystic medl degentn Cystic medial degeneration SM cells of media (pink) are Young Man. Pale areas are SM cells, but spaces in btwn! separated by cystic spaces degenerative. Found in middle aorta mostly. (vacuoles) & basophilic matl. •Ehlers-Danlos Syndrome: –Heterogeneous group of defects of collagen synthesis or assembly –Inheritance by all three Mendelian patterns –Variable phenotypes –Largely affects skin & ligaments- can do many things that most people can’t do with their bodies. Lack of elastin staining. Eventually aortas dissect. 3. Understand the pathogenesis of the most common genetic diseases Receptor Defects: •Familial hypercholesterolemia: due to mutation in gene for LDL receptor–loss of feedback control –Increased cholesterol –Early AS (atherosclerosis) & MI –Mendelian disorder: multiple mutations –Heterozygous (1 in 500): increased cholesterol 2-3X, increased AS & xanthomas –Homozygous: 5-6X increased cholesterol, early AS, MI in 20s Image at right: 3 & 4. Plasma conc of chol and whether homozyg, hetero or nl, the cholesterol levels get up into 800-1000 with homozygotes and then progressively less. Inversely correlated with # of LDL receptors. 4 Liver is impt for cholesterol metabolism. Only Receptors for IDL & LDL are impt. Possible mutations: 7% in serum. VLDL produced in liver fat Cholesterol taken up, merge with lysosomes, Transport is most common, where they have tissue lipoprot lipase releases TGs. IDL & Free cholesterol in cytoplasm. If oversupply trouble going from ER to golgi. LDL taken up into liver cell. leads to inhibition of LDL rec & HMGCoA. Synthesis mutns most severe. Enzyme Defects •Lysosomal Storage Diseases: –Membrane-bound bags of hydrolytic enzymes, autophagy & heterophagy –Enzyme defect leads to substrate accumulation in cell –Mutations may affect enzyme activator, post-translational processing, substrate activator, lack of transport protein Lysosomal enzy prot is targeted through the golgi with Complex substrate made up of multiple M-6-P tag that directs through the lysosome. componentstiny products. Gangliosidosis (fat + Carb that is often seen in neurotissue) •Tay Sachs (GM2) most common of 3 types affecting hexosaminidase A, all with similar phenotypic effects –Eastern European (Ashkenazi) Jews (carrier rate 1 in 3) founder effect –Gangliosides accumulate in all tissues but neurons in CNS & retina affected most (ballooning degeneration with oil red o-positive vacuoles) –NL at birth–CSx by 6 months–mental and motor deterioration, blindness, cherry-red spot on macula –Multiple mutations on Chr 15 (Sandoff & activator def on chr 5) Know the names of dx, and briefly the clinical manifestations. Whorled= redundant membs. 5 Neimann-Pick Disease •Heterogeneous group that lead to accumulation of sphingomyelin & cholesterol •Two major types •Type A accounts for 75-80% (def. sphingomyelinase) –Severe infantile form, CSx by 6 months –Viscera & CNS affected (hepatosplenomegaly) –Skin xanthomas –Small uniform lipid vacuoles accumulate in mononuclear phagocytes and neurons with increase in size to 90m –Spleen to 10X NL –Retinal cherry-red spot in 1/3 to ½ (similar to seen in Tay-Sachs) –Have FTT, generalized lymphadenopathy, progressive psychomotor deterioration, death 1-2 yrs Residual white pulp looks nl, red pulp is replaced monocytic/phagocytic cells w/ vacuolated cytoplasm. These stain for lipid. Gaucher Disease •Group of autosomal recessive disorders with defect in glucocerebrosidase –Most common lysosomal storage disorder –Cleaves glucose from ceramide –Accumulates in macrophages ( abundant cytoplasm) –Three clinical subtypes •Type 1: –99% –Chronic non-neuropathic form –Accumulation esp. in spleen & bone marrow, esp. European Jews •Gaucher cells in spleen, liver, bone marrow: fibrillary distended cytoplasm (PAS-positive) •CSx: 1st appear in adult life, often pancytopenia or thrombocytopenia secondary to hypersplenism –May have bone pain or pathologic fractures, but compatible with long life Gaucher cells in bone marrow have pale LN filled w/ pale eosinphilic Gaucher cells fill alveoli in PAS positive (left) & unstained histiocytes granular (basophilic) cytoplasm with a fibrillar histiocytes in Gaucher Disease lungs of patient w/ long- (right) in Gaucher Disease appearance standing disease Mucopolysaccharidoses (MPS) •Group of deficiencies of degradation of glycosoaminoglycans, accumulate within macrophages and endothelium (found in cartilage, heart valves, & bones) –MPS I H: Hurler syndrome, def a-L-iduronidase, most severe form of MPS •NL at birth •6 mos hepatosplenomegaly •skeletal deformities death in 6-10 yrs of CV complications –MPS II H: Hunter syndrome (just be vaguely familiar with this) •X-linked •milder CSx •no corneal clouding Image at right: course muscular features. Hunter live longer. 6 Glycogen Storage Diseases •Glycogenoses: deficiency of one of enzymes of glycogen synthesis or degradation, liver and muscle target organs, Types I-VIII –Hepatic forms: von Gierke disease (Type I), def. G-6-phosphatase •hepato-renomegaly: glycogen in cortical tubular epithelium, hypoglycemia, FTT, bleeding tendency, 50% mortality –Myopathic forms: McArdle syndrome (Type V), def. muscle phosphorylase •accumulation of subsarcolemmal glycogen •painful cramps after exercise without increase in venous lactate •normal longevity Cell Growth Gene Defects •Most in somatic cells–CA, ~5% transmitted through germline, proto-oncogenes and tumor-suppressor genes –Neurofibromatosis-1 (von Recklinghausen disease): 1/3000, 50% autosomal dominant, penetrance 100% but variable expressivity. Have: •multiple neural tumors •numerous pigmented skin lesions (90%)–”cafe au lait” spots •iris hamartomas–Lisch nodules –Neurofibromas: •Arise from nerve trunks in skin •Soft, multinodular tumors 1 cm to > 20 cm (plexiform) •Contain all elements, i.e., proliferating neurites, Schwann cells and fibroblasts within loose myxoid stroma •Mal transformation 3% –NF-1: Gene mapped to chr 17q11.2, variable expression, pts also have bone cysts, scoliosis, meningiomas, optic gliomas –NF-2: Bilateral acoustic schwannomas, may not have skin tumors, no Lisch nodules, mapped to chr 22 Multifactorial Inheritance (most common cause of congenital dx) •Increased risk if parents severely affected •Greatly modified by environment •Risk in sibling of affected child same (2-7%) •Ex: DM, cleft lip and palate, CHD, HTN Nonclassic Inheritance •Triple repeats (cause a variety of genetic disorders) •Genomic imprinting (uncommon, but an impt concept) •Mutations in mitochondrial genes (least common, not talking about these) Nonclassic Inheritance: Triple Repeat Mutations •Fragile X, HD, myotonic dystrophy –Fragile X: One of most common forms of familial MR, X-linked, IQ 40-70, macro-orchidism in 80%, long face, large mandible, large everted ears •20% of affected males are carriers, 30% of carrier females have MR, anticipation = clinical features worsen with successive generations (for these reasons it is considered an non-classic inheritance) •Mechanism: nl to have 6-54 tandem repeats of CGG at Xq27 •“Premutations”: 52 - 200 CGG repeats (these people look like carriers) •“Full mutations”: 250 - 4000 repeats, amplified in oogenesis (people have the dx/manifestation sof it) Nonclassic Inheritance: Genomic Imprinting •“Parent of origin” effects, one parent expressed for given gene –Prader-Willi & Angelman syndromes: same area deleted; del15q1113 –PWS: MR, short stature, hypogonadism, FTT early, obesity later, all cases del is in paternal chr 15 –AS: MR, ataxic gait, SZ, inappropriate laughter = “happy puppets,” have deletion on maternal chr 15 –Mechanism: methylation of DNA –Some cytogenetically nl have two copies of 15 from one parent = uniparental disomy (can play a role in genomic imprinting and cause the disorder) Trinucleotide repeat blot showing pre- and full mutations. Southern Blot, using restriction endonucleases. As CCG repeats inc the size incs. PCR is a lot faster and cheaper for the most part. 7 Genomic Imprinting as seen in Prader-Willi & Angelman Syndromes It has to do with the “sex of the deletion”, maternal or paternal. Both chrs from mother uniparental disomy PW. Angelman Syndrome Molecular Diagnosis •Detection of inherited mutations •Detection of acquired mutations in neoplasia •Dx & classification of hematopoietic neoplasms •Dx of infectious diseases (TB & HIV) •Determination of relatedness & identity in transplantation, paternity testing and forensic medicine •Advantages: –Very sensitive (can be disadvantage) –Cells need not be alive •any cell works (except mature RBCs with no nucleus) 8 Questions 1. 2. Does nondisjunction occur during meiosis or mitosis in aneuploid cytogenetic disorders? Faconi anemia is what kind of cytogenetic disorder? a. Aneuploid b. Mosaicism c. Chromosome breakage syndromes d. Rearrangement 3. What chromosome abnormality causes most of Trisomy 21? 4. What syndrome displays severe MR, microcephaly, found face & some survive to adults. 5. In what transmission pattern is penetrance usually complete? a. Autosomal dominant b. Autosomal recessive c. X-linked 6. Aortic cystic medial degeneration is a trigger word to make you think of which specific disorder? 7. What is mutated in familial hypercholesterolemia? 8. Tay Sachs is caused by what mutation? 9. What accumulates in Neimann-Pick Disease? 10. A defect in glucocerebrosidase leads to which autosomal recessive disorder? 11. Hurler syndrome is the most severe form of MPS and is caused by a defect in what? 12. Is the delation paternal or maternal in PWS? Answers: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Meiosis C Extra chromosome Cri du chat B Marfan Syndrome In the gene for the LDL receptor Chromosome 15 (& chromosome 5) is mutated affecting hexosaminidase Sphingomyelin Gaucher Disease A-L-iduronidase Paternal 9