RA 1
advertisement

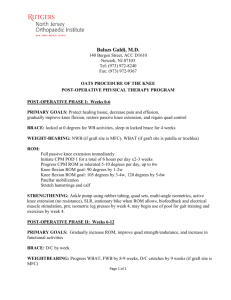
Rheumatoid Arthritis Patient Presentation Chief Complaint "I have pain in all of my joints, a swollen left knee, and stiffness every morning." HPI J H is a 58 yo woman who presents to her rheumatologist with generalized arthralgias, a swollen left knee, and morning stiffness. These symptoms have been occurring with increasing severity for the past week. She presented with the same symptoms when she came to clinic 2 months ago. PMH RA x 6 years hysterectomy 4 years ago HTN x 10 years FH Father died from complications after a traumatic fall at age 65. Mother died of hip fracture and pneumonia at age 78.No siblings. SH Housewife; married for 32 years; has two grown children with no known medical problems. Denies alcohol or tobacco use. Volunteers in the community extensively but has been doing less in the past 2 months. ROS Swelling in left knee; no rash, nausea, vomiting, or diarrhea; decreased ROM in hands; denies HA, chest pain, SOB, bleeding episodes, or syncope attacks; fatigue experienced daily during afternoon hours; denies loss of appetite or weight loss; reports minor visual changes corrected with stronger prescription glasses. Meds HCTZ 25 mg po Q AM Norvasc 10 mg po QD Relafen 750 mg, 2 tabs Q HS Prednisone 5 mg, 1/2tab po QAM Patient receives medications at a local community pharmacy. Medication profile indicates that she refills her medications on time the first of each month. All Penicillin (rash 25 years ago) PE Gen 1 Pleasant middle-aged Caucasian woman in moderate distress due to pain and swelling in knee VS BP 138/80, P 82, RR 14, T 98.8°F; Ht 66", Wt 144 lb. Skin No rashes; normal turgor; no breakdown or ulcers HEENT Atraumatic; moon facies; xerostomia Neck/LN Supple, no JVD or thyromegaly; no bruits; palpable lymphnodes Chest CTA CV RRR; normal S1,S2; nor m/r/g Abd Soft, NT/ND; (+) BS Breasts Normal; no lumps GU/Rect Deferred MS/Ext Hands-mild RA changes; swelling 3, 4, 5 PIP joints bilaterally; pain 3, 4 MCP joints on left; Boutonniere deformity 3,4 bilaterally; ulnar deviation bilaterally; decreased grip strength, L> R (patient is left-handed). Wrists-good ROM. Elbows-good ROM; slight permanent contracture on right; fixed nodule. Shoulders--decreased ROM(especially abduction) bilaterally Hips—decreased ROM on right; atrophy of quadriceps, L > R Knees-pain bilaterally; decreased ROM on left; edema on left Feet-no edema. Labs Na 135 mEq/L K 4.1 mEq/L CI 101 mEq/L CO2 22 mEq/L BUN 12 mg/dL SCr 0.8 mg/dL Hgb 10.0 g/dL Hct 31% WBC 13.5 x 103/mm3 PLt 356 x l03/mm3 Ca 9.1 mg/dL Urate 5.1 mg/dL T. chol219 mg/dL CK < 20 IU/L ANA negative 2 ESR 47 mm/hour RF positive, 1:1280 UA Normal Chest X-ray No fluid, masses, or infection; no cardiomegaly Synovial Fluid From knee; white cells 23.0 x 103/mm3, turbid in appearance Assessment 58 yo woman in moderate distress with acute flare of RA. RA not adequately controlled with current therapy. Patient is adherent with current medication regimen. HTN is controlled on present therapy. Questions Problem Identification 1. a. List the patient's drug-related problems. b. What information (signs, symptoms, laboratory values) indicates the presence and severity of rheumatoid arthritis? c. What additional information is needed to assess the patient? Desired Outcome 2. What are the goals of pharmacotherapy in this case? Therapeutic Alternatives 3. What non-pharmacological modalities may beneficial to this patient? b. What pharmacologic alternatives are available for the treatment of RA? Optimal Plan 4. What drug, dosage form, dose, schedule, and duration of therapy are best for this patient? Outcome Evaluation 5. What clinical and laboratory parameters are necessary to evaluate the patient's drug therapy? Patient Counseling 6. What information should be provided to the patient to enhance adherence, ensure successful therapy, and minimize adverse effects? 3