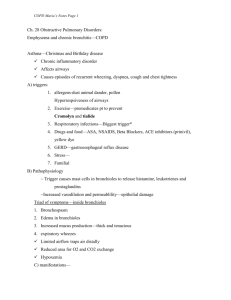
COPD-Case-Study
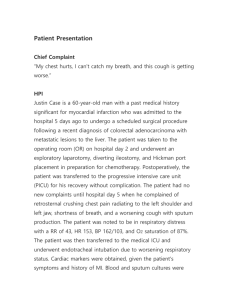
advertisement

COPD Case Study Part 1 Patient name: DH DOB: 7/14 Admit Date: 8/23 Age: 65 Sex: Male Education: Bachelor's degree Occupation: Retired manager of local grocery chain Hours of work: N / A Household members: Wife age 62, well; four adult children not living in the area Ethnic background: Asian American Religious affiliation: Methodist Referring physician: Marie McFarland, MD (pulmonary) Chief complaint: "My husband has had emphysema for many years. He was working in the yard today and got really short of breath. I called our doctor, and she said to go straight to the emergency room.” Patient history: Onset of disease: The patient has a long-standing history of COPD secondary to chronic tobacco use, 2 PPD for 50 years. He was in his usual state of health today with marked limitation of his exercise capacity due to dyspnea on exertion. He also notes two-pillow orthopnea, swelling in both lower extremities. Today, while performing some yard work, he noted the sudden onset of marked dyspnea. His wife brought him to the emergency room right away. There, a chest radiograph showed a tension pneumothorax involving the left lung. Patient also states that he gets cramping in his right calf when he walks. PMH: Had cholecystectomy 20 years ago. Total dental extraction 5 years ago. Patient describes intermittent claudication. Claims to be allergic to penicillin. Diagnosed with emphysema more than 10 years ago. Has been treated successfully with Combivent (metered dose inhaler )-2 inhalations qid (each inhalation delivers 18 mcg ipratropium bromide; 130 mcg albuterol sulfate). Diagnosed with Type 2 Diabetes three years ago, treated with Janumet daily. Home Meds: Combivent, Lasix, Janumet, O2 2 L/hr via nasal cannula at night Smoker: Yes, 2 PPD for 50 years Family Hx: What? Lung cancer Who? Father Physical exam: General appearance: Acutely dyspneic Asian American male in acute respiratory distress Vitals: Temp 97.6°F, BP 110/80 mm Hg, HR 118 bpm, RR 36 bpm Heart: Normal heart sounds; no murmurs or gallops HEENT: Within normal limits; funduscopic exam reveals AV nicking Eyes: Pupil reflex normal Ears: Slight neurosensory deficit acoustically Nose: Unremarkable Genitalia: Unremarkable Throat: Jugular veins appear distended. Trachea is shifted to the right. Carotids are full, symmetrical, and without bruits. Rectal: Prostate normal; stool hematest negative Neurologic: DTR full and symmetric; alert and oriented X 3 Extremities: Cyanosis, 1 + pitting edema Skin: Warm, dry to touch Chest/lungs: Hyper resonance to percussion over the left chest anteriorly and posteriorly. Harsh inspiratory breath sounds are noted over the right chest with absent sounds on the left. Using accessory muscles at rest. Abdomen: Old surgical scar RUQ. No organomegaly or masses. BS reduced. Circulation: R femoral bruit present. Right PT and DP pulses were absent. Nutrition Hx: General: Wife relates general appetite is only fair. Usually, breakfast is the largest meal. His appetite has been decreased for past several weeks. She states that his highest weight was 135Ibs 6 months ago, but feels he weighs much less than that now. Usual dietary intake: AM: Egg, hot cereal, bread or muffin, hot tea (with milk and Equal) Lunch: Soup, sandwich, hot tea (with milk and Equal) Dinner: Small amount of meat, rice, 2-3 kinds of vegetables, hot tea (milk and Equal) Food allergies/intolerances/aversions: NKA Previous nutrition therapy? No, was told to omit potatoes when diagnosed with Type 2 DM. Food purchase/preparation: Wife Vit/min intake: None Anthropometric data: Ht 5' 4", Wt 122 lbs, UBW 135 lbs Dx: Acute respiratory distress, COPD, peripheral vascular disease with intermittent claudication, Type 2 DM Tx Plan: ABG, pulse oximetry, CBC, chemistry panel, UA Chest X-ray, ECG Proventil 0.15 in 1.5 mL NS q 30 min X 3 followed by Proventil 0.3 mL in 3 mL normal saline q 2 hr per HHN (hand-held nebulizer); Spirogram post nebulizer Tx Solumedrol 10-40 mg q 4-6 hr; high dose = 30 mg/kg q 4-6 hr (2 days max), SSI as needed IVF D5 ½ NS at 75 mL/hr NPO Hospital course: In the emergency room, a chest tube was inserted into the left thorax with drainage under suction. Subsequently, the oropharynx was cleared. A resuscitation bag and mask was used to ventilate the patient with high-flow oxygen. Endotracheal intubation was then carried out, using the laryngoscope so that the trachea could be directly visualized. The patient was ventilated with the help of a volume-cycled ventilator. Ventilation is 7.5 L/min with a Fi02 of 100%, a positive end-expiratory pressure of 6, and a tidal volume of 700 mL. Respiratory Therapy and a pulmonologist were consulted for vent management. Daily chest radiographs and ABGs were used each AM to guide settings on the ventilator. A nutrition consult was ordered on Day 2 of admission, physician requested TF recommendations. Lab Sodium Potassium Chloride PO4 Magnesium Osmolality CO2 Glucose BUN Creatinine Calcium ALT AST Alk Phos Albumin T. Protein Prealbumin pH pCO2 p02 HCO3 Normal 135-145 mEq/L 3.5-5 mEq/L 95-105 mEq/L 2.3-4.7 mg/dL 1.8-3 mg/dL 285-295 mmol/kg/H20 23-30 mEq/L 70-110 mg/dL 8-18 mg/dL 0.6-1.2 mg/dL 9-11 mg/dL 4-36 U/L 0-35 U/L 30-120 U/L 3.5-5 g/dL 6-8 g/dL 18-35 mg/dL 7.35-7.45 35-45 mmHg >80 mmHg 24-28 mEq/L Day 1 138 3.9 101 4.5 1.9 293 30 193 9 0.7 9.1 15 12 114 3.2 6.1 16 7.2 65 56 38 Patient Care Summary Sheet Day: 2 Temp (C) Pulse Respiration BP Intake Oral IV TF Formula/Flush Shift Total Output Cath Emesis BM Drains Shift Total Gain Loss Signatures Room: 12 Nights 36.6 80 Wt YTDY: 55.5 110/80 NPO 75 - - - - - - 400 - Wt Today: 55.5 Days 36.5 85 Evenings 36.7 83 125/92 117/80 75 - - - - 25 25 475 150 200 25 5 75 25 45 45 75 50 45 -- -- -- -- 760 275 75 25 300 50 455 750 -55 Mary Rogers -275 Linda Clark 200 125 175 75 725 +35 Jane Patten 75