Trauma In Pregnancy
advertisement

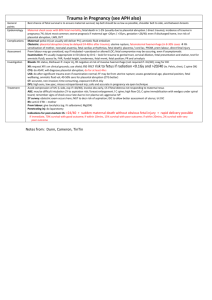
Trauma In Pregnancy General Points Best chance of fetal survival is to ensure maternal survival; lap belt should be as low as possible, shoulder belt to side, and between breasts Epidemiology Maternal shock associated with 80% fetal mortality; fetal death in 1-2% (usually due to placental abruption / direct trauma); incidence of trauma in pregnancy 7%; blunt most common Worse prognosis if: maternal age <20yrs / >35yrs, gestation <28/40 Even if discharged home, risk of placental abruption, LBW, DVT Complications Maternal: pelvic # (can usually still deliver PV); amniotic fluid embolism Obstetric: placental abruption (may be delayed 24-48hrs after trauma), uterine rupture, fetomaternal haemorrhage (in 8-30% cases rhesus sensitisation of mother, neonatal anaemia, fetal cardiac arrhythmias, fetal death); placenta / cord laceration, premature rupture of membranes, premature labour, direct fetal injury Assessment Premature labour may go unnoticed, especially if intubated + paralysed or altered LOC; fetal compromise may be occuring, even if asymptomatic Examination: PV usually inappropriate in ED (done by O+G – look for trauma to genital tract, cervical dilation, fetal presentation and station, test for amniotic fluid); assess lie, fetal heart rate, fundal height, tenderness, fetal movement, fetal position; PR and urinalysis Investigation Bloods: rhesus statusl coag for DIC Kleihauer if: major injury, Rh negative at risk of massive haemorrhage (not required if <16/40) XR: request XR’s on clinical grounds; use shield; no risk to fetus if radiation <0.1Gy and >20/40 (ie. Pelvis, chest, C spine OK) CTG: do ASAP; will diagnose placental abruption; do for at least 4hrs USS: do after significant trauma even if examination normal; free fluid may be from uterine rupture; assess gestational age, placental position, fetal wellbeing, amniotic fluid volume; 40-50% sensitivity for placental abruption (CTG better) CT: accurate, non-invasive; time consuming, exposure 0.05-0.1Gy DPL: high sensitivity, low specificity; misses retroperitoneal injuries; safe and accurate in pregnancy via open technique Management Avoid compression of IVC (left side, especially if >20/40), involve O+G early, Caesarian section if fetal distress not responding to maternal resus ABC: may be difficult intubation secondary to aspiration risk / breast enlargement / C spine; high flow O2; C spine immobilisation with wedges under spinal board; remember signs of shock occur late due to plasma volume; aggressive IV fluids Secondary survey: obstetric exam occurs here; NG tube to risk of aspiration; IDC to allow better assessment of uterus; treat DIC Rhesus: anti-D if Rh – mother Premature labour: give tocolytics (eg. IV salbutamol, MgSO4) Penetrating injury: do laparotomy Indications for post-mortem Caesarian section: >24/40 + sudden maternal death without obvious fetal injury + rapid delivery possible If immediate, 70% survival with good outcome; if within 10mins, 15% survival with poor outcome; if within 20mins, 2% survival with very poor outcome TVUS: Empty gestational sac + Empty gestational sac + USS Investigation In Fetal Demise No cardiac activity + No yolk sac No fetal pole + + diameter <20mm = inconclusive do follow up gestational sac diameter >15mm (7/40) OR >21mm (8/40) (90% specificity) gestational sac diameter >9-16mm OR CRL >5-6mm (non-viable) gestational sac diameter >10-13mm gestational sac diameter >18-20mm (non-viable) If beta-hCG above discriminatory zone (>2000) and no IUP, or mass in ovary / tube = likely ectopic (90% PPV) If beta-hCG >6500 and no fetal heart seen on USS = 80% chance of miscarriage If beta-hCG below discriminatory zone (<2000) and inconclusive scan = pregnancy unknown location 48hr follow up (serial beta-hCG’s or repeat USS) Management If unstable: ?cervical shock resus, IV fluids, atropine 600mcg IV if bradycardic (to max 3mg), speculum ASAP; can consider uterine compression, vaginal packs, compression of abdominal aorta, urinary catheter, ergometrine / oxytocin Empathy; pan when toileting Rh prophylaxis – early pregnancy bleeding, singleton, <13/40 250iu IM early pregnancy bleeding, multipleton, >13/40 625iu IM Chance of Rh- mother developing antibodies to Rh+ child is <20% regardless (ie. 15%) of whether antiD is given; Kleihaur done to quantify fetomaternal haemorrhage and thus work out amount to give; of mother’s serum has detectable anti-D antibodies at 24-48hrs then correct dose has been given; if given after 3-10/7, still has some effect; 1ml protects against 6mls of fetal blood; 85% Caucasians are Rh +ive; antiD decreases risk from 1% to 0.3% Complete: conservative management Incomplete / inevitable: women’s preference 1) ERPOC – infection risk, cervical trauma, uterine perforation, intrauterine adhesions 2) Medical – misoprostol 600mcg PO (PGE1 analogue uterotonic; used in MTOP, miscarriage, induction of labour; stable, low cost, easy to give, patient acceptance; contraindications: previous uterine surgery ( risk of uterine rupture) 3) Watch and wait – longer duration of PV bleeding and pain, need for blood transfusion Discharge with Early Pregnancy Clinic referral if: bleeding not severe, easy hospital access, good discharge advice (come back if deterioration, avoid sex and tampax if threatened), cervical os closed, >6/40 with IUP on scan USS before discharge if: can’t get to EPAC <72hrs, high maternal anxiety and in-hours, >6/40 with no IUP on USS Refer gynaecology if: ?ectopic (unilateral pain, severe, pain, PMH ectopic / tubal surgery / PID), ?actively miscarrying (heavy bleeding / products / USS evidence of miscarriage), unwell, non-viable fetus on USS