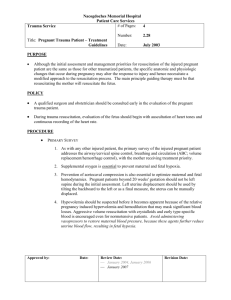
Trauma in pregnancy fact sheet
advertisement

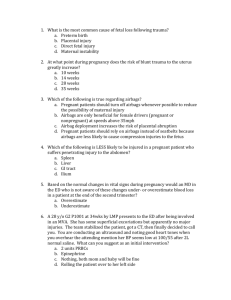
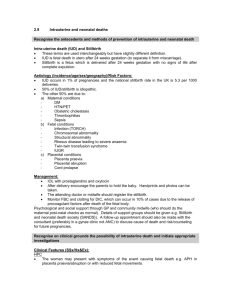
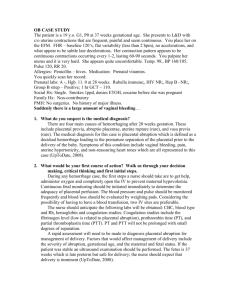
Trauma in Pregnancy (see APH also) General points Epidemiology Complications Assessment Investigation Treatment Best chance of fetal survival is to ensure maternal survival; lap belt should be as low as possible, shoulder belt to side, and between breasts Maternal shock assoc with 80% fetal mortality; fetal death in 1-2% (usually due to placental abruption / direct trauma); incidence of trauma in pregnancy 7%; blunt most common; worse prognosis if maternal age <20yrs / >35yrs, gestation <28/40; even if discharged home, incr risk of placental abruption, LWB, DVT Maternal: pelvic # (can usually still deliver PV); amniotic fluid embolism Obstetric: placental abruption (may be delayed 24-48hrs after trauma), uterine rupture, fetomaternal haemorrhage (in 8-30% cases Rh sensitisation of mother, neonatal anaemia, fetal cardiac arrhythmias, fetal death); placenta / cord lac, PROM, prem labour, direct fetal injury Prem labour may go unnoticed, esp if intubated + paralysed or altered LOC; fetal compromise may be occuring, even if asymptomatic Examination: PV usually inappropriate in ED (done by O+G – look for trauma to genital tract, cervical dilation, fetal presentation and station, test for amniotic fluid); assess lie, FHR, fundal height, tenderness, fetal mvmt, fetal position; PR and urinalysis Bloods: Rh status, Kleihauer if: major inj, Rh negative at risk of massive haemorrhage (not required if <16/40); coag for DIC XR: request XR’s on clinical grounds; use shield; no incr risk to fetus if radiation <0.1Gy and >20/40 (ie. Pelvis, chest, C spine OK) CTG: do ASAP; will diagnose placental abruption; do for at least 4hrs USS: do after significant trauma even if examination normal; FF may be from uterine rupture; assess gestational age, placental position, fetal wellbeing, amniotic fluid vol; 40-50% sens for placental abruption (CTG better) CT: accurate, non-invasive; time consuming, exposure 0.05-0.1Gy DPL: high sens, low spec; misses retroperitoneal injs; safe and accurate in pregnancy via open technique Avoid compression of IVC (L side, esp if >20/40), involve obs early, CS if fetal distress not responding to maternal resus ABC: may be difficult intubation 2Y to aspiration risk / breast enlargement / C spine; high flow O2; C spine immobilisation with wedges under spinal board; remember signs of shock occur late due to incr plasma vol; aggressive IVF 2Y survey: obstetric exam occurs here; NGT to decr risk of aspiration; IDC to allow better assessment of uterus; trt DIC Rh: anti-D if Rh – mother Prem labour: give tocolytics (eg. IV salbutamol, MgSO4) Penetrating inj: do laparotomy Indications for post-mortem CS: >24/40 + sudden maternal death without obvious fetal injury + rapid delivery possible If immediate, 70% survival with good outcome; if within 10mins, 15% survival with poor outcome; if within 20mins, 2% survival with very poor outcome Notes from: Dunn, Cameron, TinTin