File
advertisement

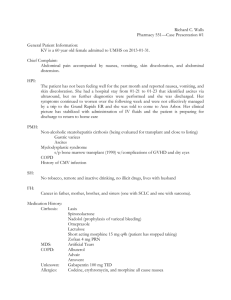
Coppin State University Helen Fuld School of Nursing Primary Health of the Family N700 Student Name: Sylvia Assiamah Date Submitted: 2/27/14 A. Demographic Data: Age, Race, LNMP 58 years old African American male B. HPI (History of present illness) B.B is a 58 year old AA male who presents with c/o severe sharp LUQ abdominal pain associated with nausea and vomiting. He states the pain started approximately 2 days ago after he ate chili. The pain seems to come on as a spasm/cramping that is quite sharp, then either goes away or turns into a burning sensation that goes to the chest. The symptoms seem to be reduced with rest. He complains of occasional indigestion at night, but has not problems sleeping. He state that during the past 7 years he has taken Mylanta for indigestion, and it tends to offer some relief, but is not helping now. C. Objective Data: Physical exam findings Vital Signs- Temp: 97.8 F RR: 22 BP: 116/74 P: 82 Height: 5 ‘8” Weight: 170 lbs. General appearance/skin: Neatly dressed, well developed, and appears anxious. Skin turgor fair, no jaundice. Mouth: Lips moist. Pale oral mucosa, Tongue dry and tender to touch. Lungs: CTA Heart: S1, S2 WNL. No MRG. Abdomen: No venous distension .Symmetrical without obvious bulging. No visible peristaltic waves, High pitched hyperactive BS. No bruits or venous hums. C/o tenderness in epigastric area. Negative Murphy’s sign, psoas and rebound. Rectal: Small non-inflamed external hemorrhoids. No rashes or irritation. No tenderness on palpitation. Normal sphincter function. Prostate smooth. No masses. Hard brown stool. D. Assessment: Differential diagnoses(es) provide rationale for each differential Gastric Cancer: B.B presents with abdominal pain, nausea, and vomiting. These may be presenting signs of gastric cancer. PUD: B.B describes abdominal pain that comes and goes, with a burning sensation in his chest. An antacid offers some relief. These are characteristic symptoms of PUD. GERD: indigestion and burning in the chest are common symptoms seen with GERD. Angina: this can present as indigestion and burning in the chest. Cholecystitis: B.B presents with nausea, vomiting, and chest discomfort after eating spicy foods. Pancreatitis: Nausea and vomiting along with abdominal pain are symptoms of possible pancreatitis. Final Assessment Peptic Ulcer Disease (PUD) duodenal: Duodenal ulcers occur as a result of imbalance between the normal duodenal productive mechanisms and the amount of acid delivered to the duodenum from the stomach. T.B’s abdominal pain with indigestion, age, sex, alcohol intake, stress and history of NSAID use support the diagnosis of PUD E. Plan of Care: This is to include the following information. Pharmacological 1. Metronidazole 500mg, PO 2x/day, for 2 weeks. 2. Omeprazole 20 mg, PO 2x/day for 2 weeks. 3. Clarithromycin 500mg, PO 2x/day for 2 weeks Education 1. Take the prescribed medications for the full 2 weeks as prescribed. 2. Potential side effects of the medication (super infection, diarrhea, constipation) 3. Reduce stress 4. Minimize alcohol tobacco, and spicy foods, or foods that cause increased symptoms. Diagnostic evaluation(s) 1. Hgb/HCT, Albumin, CMP, LFTs, Stool hemoccult, H. pylori Referral(s) None at this time Follow-up 1. Follow up with this office in 2- 4 weeks. Reference Anand, BS. (2012). Peptic ulcer disease. Medscape Reference. Retrieved from http://emedicine .medscape.com/article/181753-overview

![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)