Focus on Respiratory Rate: Improved reliability of measurements in
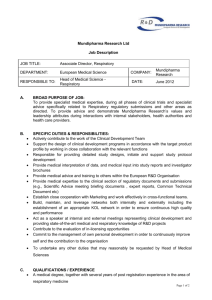
advertisement

1. Title Focus on Respiratory Rate: Improved reliability of measurements in acutely unwell adults by using electronic sensors? 2. Authors Ali Virk1, Naveed Khan1, Sophie Dorsey1, Anne Bonnici Mallia1, Mori Jones1, Elaine Hardman1, Joanne Roche1, Chris Subbe2, Bernd Duller3 3. Institution 1 Ysbyty Gwynedd, Penrhosgarnedd, Bangor, UK School of Medical Sciences, Bangor University, Bangor, UK 3 Philips Healthcare, Stuttgart, Germany 2 4. Introduction Respiratory Rate is the strongest predictor of adverse outcomes such as cardiac arrests or unscheduled critical care admission. We aimed to establish whether electronic respiratory sensors [a] would be able to monitor respiratory rate reliably in acutely unwell patients [b] would lead to changes in the values observed 5. Methods VITAL II is an interventional trial of an integrated monitoring system with automated notification of deteriorating patients. The Philips wireless IntelliVue CL Respiration Pod (Fig 1) is a sensor that uses 3D accelerometer technology to measure respiration. An attachment for the sensor allows placement to the patient’s chest for signal acquisition. The setting: 28 bedded ward in a district general hospital with a mixture of gastroenterological and general medical patients. The majority of patients were emergency admissions with acute illness. Reproducibility study: Respiratory rate was measured simultaneously in an unselected patient cohort over one minute by a trained clinician and the sensor. Measurements by the sensor were every 12 seconds and averaged over one minute. Frequency distribution during clinical application: We compared respiratory rates that were manually obtained as part of routine surveillance of vital signs and respiratory rates that were recorded from sensors in the same patient cohort during May 2014. 6. Results Reproducibility study: We recorded 140 datasets in 31 patients (Mean age 66 years, mean bodymass index 25). Respiratory rates measured by clinicians and by sensors had a high level of agreement (linear correlation 0.91) with a mean of 15.8 by clinician and 15.5 by sensor. The average of differences (mean bias) was -0.31 rpm (SD for differences 1.91 rpm, t=2,292, p=0,0229, t-test for paired samples). Frequency distribution: We analysed data from 1513 manual measurements and 103 measurement by the sensor. Analysis of distribution showed clustering of respiratory rates around the values of 16 (26%), 18 (33%), 20 (22%) in the manual cohort. Frequencies in the cohort measured by the Sensor were 16 (5%), 18 (9%) and 20 (5%). (Fig 2). 7. Discussion Electronic sensors are able to measure respiratory rates reliably in acutely unwell patients. Even in our environment where over 90% of sets of vital signs contain a respiratory rate in emergencies or with staff under pressure a significant number of values are possibly extrapolated or based on clinical impression rather than measurement. Faulty measurements could underestimate the severity of acute deterioration and delay escalation. The impact on clinical outcomes requires further evaluation. 8. Conflicts of interest The study was part of the VITAL II study, a clinical trial sponsored by Philips Healthcare. CPS is PI of the VITAL II study, and has received speaker fees from Philips. BD is a consultant for Philips. Fig 1: Respiratory rate sensor with additional capability to record heart rate and posture of a patient Fig 2: Respiratory rate distribution in manual (top panel) and electronic (bottom panel) acquisition in acutely unwell patients