Froberg_Tropical_disease_Zoo_vector_4.8.10
advertisement

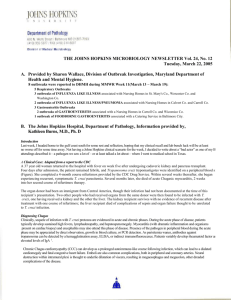
Tropical, Vector-borne and Zoonotic Infectious Disease Pathology – Froberg---4.8.10 PURPOSE •To learn the etiological agents and life cycles of the major tropical, vector-borne and zoonotic parasites. •To learn the major pathology associated with the important tropical, vector-borne and zoonotic pathogens. CHAGAS’ DISEASE (AMERICAN TRYPANOSOMIASIS) TRYPANOSOMA CRUZI •Organism: hemoflagellate (motile) •Vector: Triatoma infestans (reduviid, kissing or assassin bug) •Transmission: Vector lives in thatched or mud houses, biting sleeping victim at night, depositing infected feces in wounds. •Zoonosis: between mammals and vector •Dx: finding trypomastigotes in blood - -Epidemiology: Chagas Disease is most common in Central America and northern South America. -Chagas is also a transfusion risk in the United States from infected blood donors who have immigrated from Latin America -mirco: Charac “U” or “C” shape of T. cruzi in peripheral blood -Nuclei (green) and kinetoplasts(black) are stained blue with Geimsa Life Cycle: 1 - Dliated cardiomyopathy with destruction of the ventricular wall and an apical aneurysm 2 to Chagas Diseases Virulence Factors •Produces homolog of decay-accelerating factor (DAF) that inhibits formation of C3 convertase & blocks alternate pathway of complement •Produces neuraminidase that cleaves sialic acids from host proteins lining lysosomes - destabilizes organelle •Produces hemolysins that form pores in lysosomal membranes •Burst host cells in going from amastigote to trypomastigote forms (huge inflam response) Amastigotes of T. cruzi within cardiac myocyte Apical aneurysm from T. cruzi infection AFRICAN TRYPANOSOMIASIS SLEEPING SICKNESS •Trypanosoma brucei rhodesiense (East Africa). Acute, virulent. •T. b. gambiense (West Africa), Chronic •Transmission: Tsetse fly •Within host, parasite undergoes successive changes of surface antigens, VSG (variable surface glycoprotein) waves of parasitemia (unique!) •Zoonotic: wild mammals man •Disease: –Waves of antibody-induced parasite deaths recurrent fever. –Invasion heart, liver, spleen, nodes (lymphocytes, macrophages) brain often fatal lethargy coma death •Brain: Leptomeningitis demyelinating panencephalitis plasma cells containing glycoprotein globules (flame cells) -Chancre at site of Tsetse fly bite with transmission of Trypanosomes Life Cycle: •Clinical: –Stage 1: Chagoma (local, transient inflammatory lump) at site of bite –Stage 2: Dissemination: Myocarditis; enlarged spleen, liver, & lymph nodes –Stage 3: Years later (10-30% infected persons): cardiac inflammation and fibrosis, dilated cardiomyopathy, apical aneurysm •Myenteric plexus damage aperistalsis mega-esophagus + mega-colon •Prevalence: –Only in western hemisphere. –Most common cause of heart failure in Latin America –Up to 1/2 million in USA transfusion hazard -Romana’s sign from acute conjunctival T. cruzi infection ONCHOCERCA VOLVULUS (FALARIAL NEMATODE) •Transmission: Black flies: genus Simulium (tropical Africa) •Cycle: Adult worms mate in skin local infl. Nodule microfilariae eye keratitis and retinitis blindness •Rickettsia-like bacteria of genus Wolbachia live within nematode-probably cause pathology -S/Sx: Dermatitis from Onchocerca adults in skin Tropical, Vector-borne and Zoonotic Infectious Disease Pathology – Froberg---4.8.10 -Keratitis (clouding of cornea) & blindness associated with microfilarial infection of eye •Pathology: Parasite-laden macrophages in granulomatous inflammation Filariasis WUCHERERIA BANCROFTI Brugia malayi (less common) •Mosquito is vector. Tropics. •Larva circulates in blood mature worm in lymphatics •Humans only reservoir •Nematode worm intense inflammation, necrosis, destructive scarring •Resulting lymphatic obstruction massive edema (elephantiasis) •Wuchereria bancrofti 90% of infections -Epi: Tropical distribution of filarial nematodes -Dx: Diagnosis is made by finding microfilaria in blood smear VISCERAL LEISHMANIASIS (KALA-AZAR: BLACK DISEASE) •Etiology: –L. donovani (Old World) –L. chagasi (New World) •Clinical: Systemic dissemination nodes, liver, spleen •Pathology: Like mucocutaneous but involving viscera •Death: Bacterial infection, pancytopenia, progressive wasting Enlarged liver & spleen in Pt with visceral leishmaniasis Cross section of adult filarial nematode within lymphatic channel fibrinous Rx obstruction Massive lymphedema from filariasis – thickening of skin from lymphedema and poor circ LEISHMANIASIS •Mucocutaneous Leishmaniasis (Espundia) -3 types: visceral, cutaneous, and mucocutaneous •Etiology: Leishmania braziliensis (protozoan) •Transmission: Sandfly. Only in tropical New World •Thrive in macrophage phagolysosomes, proton pump raises pH, lipophosphoglycans inhibit lysosomal enzymes •Glycolipid gp63 = complement-cleaving proteinase •Cell-mediated immunity protective, parasite causes Th1 Th2 switch which inhibits macrophage activation (TQ) •Dense glycocalyx binds C3b and resists lysis by C5-9. -Epi: Tropical distribution -Life Cycle: amastigotes can survive within macrophages –Disfiguring –destructive inflammation, nose –anus –vulva Kupffer cell containing amastigotes in visceral leishmaniasis SCHISTOSOMA MANSONI, S. JAPONICUM, S. HEMATOBIUM •Life cycle: complex: Snail larvae human (via skin) mature adult worms in portal & pelvic veins eggs granulomas with eosinophils - so Th1 & Th2 responses •Disease: –S. mansoni, S. japonicum liver cirrhosis & portal HTN –S. hematobium bladder hemorrhage & Sq carcinoma Life Cycle: -SM & SJ come out in feces; SH in urine Eosinophilic & granulomatous inflammation around Schistosome eggs in bladder •Clinical: 2 Squamous cell carcinoma of bladder in pregnant Pt with Schistosomiasis ZOONOSES •Pathogens that are spread to humans from other animals •Transmission may involve insect/arthropod vectors, direct or indirect transmission 3 Tropical, Vector-borne and Zoonotic Infectious Disease Pathology – Froberg---4.8.10 Not all of these in the lecture: •Epidemiology: prevalence if clothing not changed –war, poverty •Brill-Zinsser: recurrent typhus after long latent interval -decades, probs due to change in host immunity RICKETTSIA •Rickettsia: small aerobic gram negative coccobacilli •Vector-borne obligate intracellular parasites •Infect endothelial (TQ!)& smooth muscle cells •Endotoxin •Abrupt onset fever, chills, headache, myalgia, rash •Rx: tetracyclines Q FEVER •Q fever: Coxiella burnetti, worldwide •Droplet inhalation or direct contact •Reservoir: cattle, sheep, goats •Clinical: subacute, fever, HA, malaise –lungs: interstitial pneumonitis –liver: LFP, hepatomegaly, 1/3 jaundice •Epidemiology: slaughterhouse & farm animals •Pathology: –lung intersitial pneumonitis –liver & BM ring granulomas –DX: serology –Rx: tetracycline –Prognosis: rarely fatal Ring granuloma in liver (also in BM) RG = Central lipid vacuole surrounded by macros EPIDEMIC TYPHUS •Rickettsia prowazekii, ~worldwide •Vector: body louse (Pediculus corporis) •Louse lives only on humans or in human clothes •Clinical: fever, vasculitis rash, cerebral damage •Mortality 5-25% •Pathology: –skin necrosis & gangrene –heart, lungs, etc. ecchymosis/hemorrhage –brain typhus nodule (perivasc cuffing of vessel w/microglia cells) ROCKY MOUNTAIN SPOTTED FEVER (misnomer) •Rickettsia rickettsia: U.S., esp. SE & SC •Vector: Dermacentor ticks (wood, dog, lone star) •Reservoir: dogs & wild rodents •Clinical: rash incl. soles & palms, fever, chills, myalgia, DIC •Mortality 3% -- mainly from DIC •Pathology: –skin vascular necrosis & thrombosis –brain perivascular inflammation (like typhus nodule) –lungs pneumonitis -bugs in endothelium of bld vessels •Epidemiology: –90% April September –Most common in children -Central/SE US Erythematous maculopapular rash of RMSF. Rash often involves soles and palms Denuded endothelium & thrombosis from RMSF ANAPLASMOSIS (EHRLICHIOSIS) •Ehrlichia canis, Anaplasma phagocytophilum, E. ewingii, E. chaffeensis, U.S. •Vector: ticks (deer, wood, dog) •Reservoir: unknown •Clinical: like RMSF: Fever, HA, rash 20% •Pathology: like RMSF but less severe, thrombocytopenia •Dx: “purple blobs” in WBCs Morulae (bact clumps) in WBCs in Pts with Anaplasmosis: Tropical, Vector-borne and Zoonotic Infectious Disease Pathology – Froberg---4.8.10 LYME DISEASE •Borrelia burgdorferi, spirochete, US, Europe & Japan •Vector: hard-shelled ticks (Ixodes scapularis) •Reservoirs: deer, deer mice •Clinical: –tick bite erythema migrans –dissemination cranial neuritis, meningoencephalitis, heart block, myocarditis –late chronic chronic, destructive arthritis, neuropathy •Dx: serology, PCR, culture •Pathology: –skin Perivasc lymphocytes & plasma cells –meninges hypercellular CSF, IgGs vs. Borrelia –joints like Rheumatoid arthritis (usu a large jnt) ¨plasma cell synovitis ¨“onionskin”- like arteries (most commonly seen in SLE) ¨erosion of cartilage Epi: May- July highest incidences; most in NE and N. Central US and west coast LEPTOSPIROSIS •Spirochetes, multiple serotypes, worldwide •Spread: contaminated water or occupational exposure •Reservoirs: wild & domestic animal •Clinical: most subclinical, fever, myalgia –meningitis ~aseptic –liver 10% jaundice, mortality ~10% –lungs pneumonitis, hemorrhage •Pathology: scant inflammation TULAREMIA •Francisella tularensis –small gram-negative coccobacillus –worldwide •Spread: contact, ticks, inhalation •Reservoirs: rabbits, ticks, beaver (many!) •Clinical: protean, fever, chills, malaise –ulceroglandular ulcer, draining nodes –systemic bacteremia, pneumonia •Pathology: –early = neutrophilic infl., then granulomatous infl., stellate abscess (pale histocytes surrounded by dark lymphocytes) •Dx: serology, culture •Rx: streptomycin •Mortality < 1% with antibiotics PLAGUE •Yersinia pestis –gram-negative rod, intracellular –~ worldwide •Vectors: –urban plague, rats (Rattus rattus) rat flea (Xenopsylla cheopsis) humans –sylvatic plague rodents, rabbits (SW US) •Clinical: high fever & painful bubo –bubonic = lymph node abscess 4 –pneumonic = rapidly develop pulmonary signs (deadliest) •Pathology: neutrophilic response –lymph nodes ulcerating lymphadenitis –lungs hemorrhagic, necrotizing bronchopneumonia, fibrinous pleuritis •Mortality: without antibiotics –bubonic ~75% –pneumonic ~90% •USA ~30 cases/yr Practice Questions: 1. What is the vector for Chagas’ disease? 2. Which of the following are virulence factors in Chagas’ disease? a. Decay-accelerating factor b. Neuroaminidase c. Hemolysins d. Burst host cells e. All of the above 3. Trypanosoma brucei is responsible for which disease? How is it transmitted? What is unique about this parasite? 4. What is transmitted by black flies, mates in human skin, and causes blindness? 5. WUCHERERIA BANCROFTI is transmitted by what vector? Causing what disease? 6. What can thrive in macrophages phagolysosomes proton pump raises pH, lipophosphoglycans inhibit lysosomal enzymes? What effect does this bug have on Th2? 7. What group of diseases are caused by an obligate intracellular parasites that infects endothelia? 8. Q Fever is transmitted by? Describe ring granulomas. 9. Ulcerograndular, stellate abscess, and small gram negative coccobacilli are characteristic of what disease? 10. Yersinia pestis is transmitted by what vector? Answers: 1. 2. 3. reduviid E Sleeping sickness, Tsetse fly, parasite undergoes successive changes of surface antigens, VSG (variable surface glycoprotein) 4. ONCHOCERCA VOLVULUS 5. Mosquito, elephantiasis 6. Mucocutaneous Leishmaniasis; •Cell-mediated immunity protective, parasite causes Th1 Th2 switch which inhibits macrophage activation 7. RICKETTSIA 8. Droplet inhalation; Ring granuloma = Central lipid vacuole surrounded by macros 9. TULAREMIA 10. rats (Rattus rattus) rat flea (Xenopsylla cheopsis) humans