Sliding Scale Insulin as a Method of Glycemic Control
advertisement
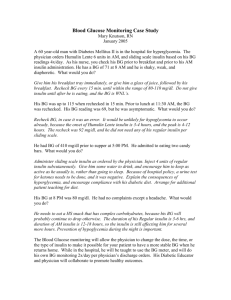
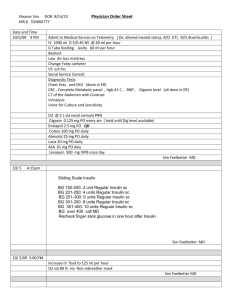
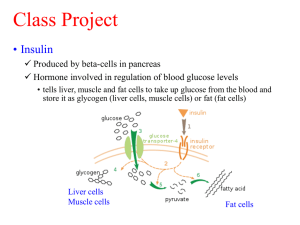
Running head: SLIDING SCALE INSULIN AS A METHOD OF GLYCEMIC CONTROL Sliding Scale Insulin as a Method of Glycemic Control Joella M. Show Ferris State University 1 SLIDING SCALE INSULIN AS A METHOD OF GLYCEMIC CONTROL Abstract I formulated a PICO question that asks about whether sliding scale insulin is a safe and appropriate method of glycemic control. The purpose of this article is to state my PICO question, state the purpose of nursing research, and provide information from research articles the answer my PICO question. I then give a recommendation to improve quality and patient safety for the non-critically ill hospitalized adult patient that requires insulin to manage their blood sugars for glycemic control. Keywords: sliding scale, glycemic control, patient, hospital, PICO, basal-bolus, insulin 2 SLIDING SCALE INSULIN AS A METHOD OF GLYCEMIC CONTROL 3 Sliding Scale Insulin as a Method of Glycemic Control The purpose of this PICO paper is to state my PICO question and how I was able to support the answer to my PICO question with nursing research that a can be used for evidence based nursing practice. Leaders in nursing practice use research to support their nursing practice. There is a formal way to communicate this research to other nurses. Using nursing research for evidence based nursing practice with improve quality and safety in patient care. PICO Question A PICO question is a clinical question that has been formatted to help a professional determine an evidence based answer for the clinical question. According to Stillwell, FineoutOverholt, Melnyk, and Williamson (2010) the acronym PICOT stands for “patient population (P), intervention of interest (I), comparison intervention of interest (C), outcome(s) of interest (O), and time it takes for the intervention to achieve the outcome(s) (T) (p. 41). I chose to leave out the (T) that represented time so my clinical question is a PICO rather than a PICOT question. My PICO question addresses sliding scale insulin, glycemic control, basal-bolus insulin and patient safety in the non-critical hospital setting. In the non-critically ill hospitalized adult population with Insulin Dependent Diabetes Mellitus (IDDM), how does administering sliding scale insulin therapy improve glycemic control when compared to administering a basal-bolus insulin regimen? This question would also apply to patients on steroids who require insulin to regulate their blood sugar levels. It is important for nursing research to be shared within the nursing community (Nieswiadomy, 2013). The results of research studies are often published in research and clinical journals or presented in lectures (Nieswiadomy, 2013). Nursing leaders can share nursing research within the nursing profession through reports, conferences, papers, and posters SLIDING SCALE INSULIN AS A METHOD OF GLYCEMIC CONTROL 4 (Nieswiadomy, 2013). As a student of Ferris State University (FSU) I have access to a large number of nursing journals in the Ferris Library for Information, Technology, and Education (FLITE). I am able to access nursing research through the FLITE library. I can share this research with my coworkers and manager in the hospital where I work. I can also use the research articles on the FLITE library to answer my PICO question. Research Findings Using the FLITE library research database I was able to complete several searches within CINAHL and PUBMED. I used the words sliding scale, glycemic control, patient, and hospital in the search engine to help narrow down the research findings. I only chose research literature that was less than five years old. Four articles stood out to me as appropriate for use in answering my PICO question. The first research article is a Retrospective Analysis. It is a Randomized Controlled Trial which is a level II in the hierarchy of evidence. This study included 331 participants. There were 121 patients in the control group who received a sliding scale (SS) insulin regimen and there were 210 patients in the experimental group who received a basal-bolus insulin regimen. The study concluded that patients who were treated with the basal-bolus insulin regimen “experienced more blood glucose measurements in the target range as compared with patients treated with SS with relatively low hypoglycemia rates” (Patel et al., 2009, p. 1774). The second research article is a Randomized Controlled Trial which is a level II in the hierarchy of evidence (Schroeder et al., 2012). This study included a small sample size of 30 participants in the control group who receive a sliding scale insulin regimen and 35 participants in the experimental group who received a basal-bolus insulin regimen. The study found that the SLIDING SCALE INSULIN AS A METHOD OF GLYCEMIC CONTROL 5 intervention group had improved glycaemic control, shorter hospital stays, and that it was easier to follow the basal-bolus insulin regimen (Schroeder et al., 2012, p. 71). The third research article is a Randomized Multicenter Trial which is a level II in the hierarchy of evidence (Umpierrez, 2011). This study uses an appropriate sample size of 211 participants. These participants are divided almost equally into a control group that receives a sliding scale insulin (SSI) regimen and an experimental group that receives basal-bolus insulin coverage regimen for control of their blood sugar. The study concluded that “basal-bolus treatment with glargine once daily plus glulisine before meals improved glycemic control and reduced hospital complications compared with SSI in general surgery patients”(Umpierrez, 2011, p. 256). The fourth research article is a level I in the hierarchy of evidence (Shaw, 2009). This article is also specifically nursing research that systematically reviewed six studies and evaluated them “using the American Diabetes Association (ADA) system for evidence ranking” (Shaw, 2009, p. 1). The result of the systematic review showed that “Five out of the six studies substantiate the current clinical practice guidelines that conclude SSI as primary treatment for hyperglycemia is ineffective and unreliable” (Shaw, 2009, p. 1). After reading several research articles (Schroeder et al., 2012; Umpierrez, 2011; Shaw, 2009; Patel et al., 2009) that compared SSI and basal-bolus insulin from level I & II on the hierarch of evidence for intervention studies (Stillwell, Fineout-Overholt, Melnyk, & Williamson, 2010), I am convinced that a basal-bolus insulin regimen is more appropriate than the sliding scale insulin regimen for glycemic control of the non-critically ill hospitalized adult patient. SLIDING SCALE INSULIN AS A METHOD OF GLYCEMIC CONTROL 6 Recommendations to Improve Quality and Safety According to the Standard 1 in the Scope and Standards of Practice written by the American Nurses Association (ANA) it is my responsibility as a professional nurse to check blood sugar levels and administer insulin therapy as ordered by my patient’s doctor (ANA, 2010). As a nurse I am concerned with the safety of my patient as I attempt to regulate their blood sugar according to the doctor’s orders. It is my responsibility to learn about evidence based nursing research and then to apply this evidence in my nursing practice in order to provide the most safe and excellent care possible for the good of my patient. I do not have the ability to directly change how I administer insulin to help maintain glycemic control for the patient I am taking care of. Standard 13 directs a nurse to collaborate with other medical professionals regarding patient care (ANA, 2010). If I become concerned that the hospital was not providing excellent patient care in regards to glycemic control because they were only using a SSI regimen rather than a basal-bolus insulin regimen for their IDDM patients then it would be appropriate for me to take this information to my manager and to the director of quality and safety for the hospital. I could ask them what their suggestions were for making this research based evidence about patient safety more widely known so hospital wide changes could occur in the way the patients were being treated. I could also consider offering this information to doctors that I have built open lines of communication with. Modifying the treatment regimen for patients with IDDM would require health care professionals to be open to change. According to Standard 8, “the registered nurse attains knowledge and competence that reflects current nursing practice” (ANA, 2010, p. 11). Nurses would require education about the change in the standard of care for patients with IDDM. The research articles listed above (Schroeder et al., 2012; Umpierrez, 2011; Shaw, 2009; Patel et al., SLIDING SCALE INSULIN AS A METHOD OF GLYCEMIC CONTROL 7 2009) mentioned the importance of nursing education when delivering basal-bolus insulin coverage. The pharmacy would need to be included in this change in patient care. The pharmacy would need to order the insulin required by the doctor’s order for basal-bolus insulin coverage for patients who require insulin for glycemic control. Changing from SSI to basalbolus insulin would probably require a committee with doctors, nurses, pharmacists, and staff from patient quality and safety. Conclusion In conclusion, research shows that sliding scale insulin coverage of non-critically ill adult patients who have been hospitalized is not based on research. A basal-bolus insulin regimen has been found to be more effective in controlling the blood sugars of a non-critically ill adult hospitalized patient. It is important for nurses to search for evidence to support their nursing practice. It is the responsibility of the professional nurse to share research findings with other nurses so that patients receive excellent evidence based nursing care. SLIDING SCALE INSULIN AS A METHOD OF GLYCEMIC CONTROL 8 References American Nurses Association [ANA] (2010). Nursing: Scope and standards of practice (2nd ed.). Silver Springs, MD: Author Fine-Overholt, E., Melnyk, B.M., Stillwell, S. B., & Williamson, K.M. (2010). Evidence-based practice step by step: Critical appraisal of the evidence: part I. The American journal of nursing, 110(7), 47-52. Doi:10.1097/01.NAJ.0000383935.22721.9c Nieswiadomy, R. M. (2012). Foundations of nursing research (6th ed.). Boston: Pearson. Patel, G. W., Roderman, N., Lee, K. A., Charles, M. M., Nguyen, D., Beougher, P., & ... Casteneda, E. (2009). Sliding scale versus tight glycemic control in the noncritically ill at a community hospital. Annals Of Pharmacotherapy, 43(11), 1774-1780. doi:10.1345/aph.1M331 Schroeder, J. E., Liebergall, M., Raz, I., Egleston, R., Ben Sussan, G., Peyser, A. & Eldor, R. (2012), Benefits of a simple glycaemic protocol in an orthopaedic surgery ward: a randomized prospective study. Diabetes Metab. Res. Rev., 28: 71–75. doi: 10.1002/dmrr.1217 Shaw K. (2009). The use of scheduled basal subcutaneous insulin in adult surgical patients: a systematic review of current research. Southern Online Journal of Nursing Research [serial online]. May 2009;9(3)Available from: CINAHL, Ipswich, MA. Accessed July 31, 2013. Umpierrez, G., Smiley, D., Jacobs, S., Peng, L., Temponi, A., Mulligan, P., & ... Rizzo, M. (2011). Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 Surgery). Diabetes Care, 34(2), 256-261. doi:10.2337/dc10-1407