1) What is evidence-based medicine?
advertisement

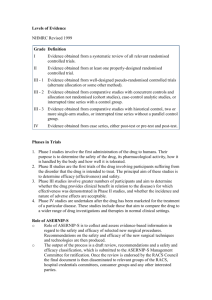
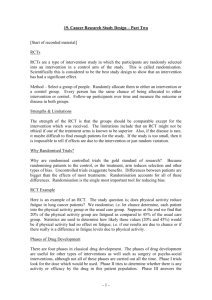
1a) What is evidence-based medicine? Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research. Good doctors use both individual clinical expertise AND the best available external evidence, and neither alone is enough. Without clinical expertise, practice risks becoming tyrannised by evidence, for even excellent external evidence may be inapplicable to or inappropriate for an individual patient. Without current best evidence, practice risks becoming rapidly out of date, to the detriment of patients. Level of Evidence: 1a – evidence obtained from meta-analysis of randomized studies 1b- evidence obtained from at least one randomized trial 2a- evidence obtained form well-designed controlled study without randomization 2b- Evidence obtained from at least one other type of well designed cohort or casecontrol study 3- Evidence obtained from well designed non-experimental studies such as comparative studies, correlation studies and case report 4-Evidence obtained from expert opinion Grade of recommendation: A- Based on clinical studies of good quality and consistency addressing the specific recommendation and including at least one randomized trial (level 1) B- Based on well-conducted clinical studies, but without randomized clinical trials (level 2,3) C- Made despite the absence of directly applicable clinical studies of good quality (level 4) 1b) What are the problems with randomisation studies? Randomized control trial o It is the gold standard for a clinical trial. RCT are often used to test the efficacy of various types of intervention within a patient population. o Double blinded Versus Single blinded o An RCT should eliminate selection & confounding bias o Prospective by design Problems with RCT’s in surgery • Quality of surgical trials is often poor with low power and small sample sizes • Expensive & time consuming • Surgical interventions are complex and difficult to standardise • Gradual changes over time in procedures and technique complicate results • Sometimes not ethical to randomise • Biases can still occur with even a carefully constructed RCT: – unconcealed allocation, – incomplete follow up, – no intention to treat analysis, – exclusions after randomisation – Selective reporting results – Blinding issues • Your patient may not be typical of those studied in the RCT (too young, too old, too frail, poor attender etc). The inherent variability of surgery requires precise definition of interventions and close monitoring of quality. _Variations on an operation are common and may influence success rates. When comparing operations, clear definitions are therefore needed of the limits on acceptable technical variation. _ The technical quality of operations undoubtedly affects outcome. Poor quality surgery represents failure to deliver the intended treatment, causing a difference between efficacy and effectiveness. Trials then measure deliverability, not efficacy Surgical learning curves cause difficulty in timing and performing randomised trials of new techniques Comparisons of surgical and non-surgical treatments with greatly different risks causes difficulties with patients' equipoise. patients often reject RCTs because they do not wish their treatment to be decided by chance Rare conditions and urgent and life threatening situations cause difficulties with recruitment, consent, and randomisation Blinding is particularly difficult in surgical trials, Only a third of surgical trials had adequate blinding of patients and/or surgeons Lack of funding, infrastructure, and experience of data collection Randomised trials in surgery: problems and possible solutions. BMJ2002. P McCulloch, Academic Unit of Surgery, University of Liverpool