FILENAME: - Consumer Learning
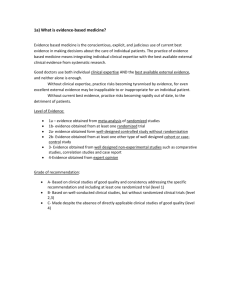
advertisement
19. Cancer Research Study Design – Part Two [Start of recorded material] RCTs RCTs are a type of intervention study in which the participants are randomly selected into an intervention in a control arm of the study. This is called randomisation. Scientifically this is considered to be the best study design to show that an intervention has had a significant effect. Method – Select a group of people. Randomly allocate them to either an intervention or a control group. Every person has the same chance of being allocated to either intervention or control. Follow-up participants over time and measure the outcome or disease in both groups. Strengths & Limitations The strength of the RCT is that the groups should be comparable except for the intervention which was received. The limitations include that an RCT might not be ethical if one of the treatment arms is known to be superior. Also, if the disease is rare, it maybe difficult to find enough patients for the study. If the study is too small, then it is impossible to tell if effects are due to the intervention or just random variation. Why Randomised Trials? Why are randomised controlled trials the gold standard of research? Because randomising patients to the control, or the treatment, arm reduces selection and other types of bias. Uncontrolled trials exaggerate benefits. Differences between patients are bigger than the effects of most treatments. Randomisation accounts for all of these differences. Randomisation is the single most important tool for reducing bias. RCT Example Here is an example of an RCT. The study question is; does physical activity reduce fatigue in lung cancer patients? We randomise; i.e. let chance determine, each patient into the physical activity group or the usual care group. Suppose at the end we find that 20% of the physical activity group are fatigued as compared to 45% of the usual care group. Statistics are used to determine how likely these values (20% and 45%) would be if physical activity had no effect on fatigue; i.e. if our results are due to chance or if there really is a difference in fatigue levels due to physical activity. Phases of Drug Development There are four phases in classical drug development. The phases of drug development are useful for other types of interventions as well such as surgery or psycho-social interventions, although not all of these phases are carried out all the time. Phase I trials look for the dose which would be used. Phase II tries to determine whether there is any activity or efficacy by the drug in this patient population. Phase III answers the -1- question of effectiveness. And Phase IV looks at the benefits and harms in routine practice. Throughout all of the phases, safety is assessed as well and if the drug appears to be unsafe, the trial maybe stopped. Click on the boxes to find out more about each phase. I Dose that can be tested further – Feasibility Phase I trials are for initial safety and dose finding. The goals are to refine the treatment, to investigate pharmacokinetics, to assess major adverse events and finally to decide whether it is ethical to continue testing in humans. There are usually a small number of participants, the dose or the timing is often increased until the maximum tolerable dose is found. II Activity that warrants further testing – Activity/Efficacy Phase II is the screening to look for evidence of biological activity. Does anything appear to be happening? The goals are to get an idea of the effective treatment on the disease process, what the major adverse events, are, if any, and to decide whether the treatment is worth studying in larger, longer trials. Phase II trials usually have a relatively small number of participants with patients who are similar to who will eventually get the drug, the follow-up is fairly short, and sometimes no comparison group. III Benefits and harms vs best standard – Effectiveness The phase three trial is the definitive assessment of safety and efficacy, and has the potential to modify clinical practice. A relatively larger number of participants are included. The inclusion criteria is wider so that patients are coming from the target population. The follow-up is long enough so that the effect of the drug, on a clinically relevant outcome, are able to be assessed with some certainty. IV Benefits and harms in routine practice - Application Phase IV studies are studies that look for longer term serious adverse effects after the drug has been approved for marketing. They are usually observational and are carried through some type of recording system, although sometimes RCTs are used. Phase III Summary To summarise, Phase III trials provide the definitive assessment of the effects of the intervention, determining whether or not there are tangible benefits to the patients, including duration of survival and quality of life. We require an evaluation of the intervention which is ethically acceptable, provides a reliable and relevant evaluation of the benefit to risk profile, and is as efficient as possible. Effects of Anticancer Treatment Throughout the development of anticancer treatment, there is always a balancing act between good and harm. A cancer treatment that extends survival by one month of highly acute toxicity is probably not worth it to most people. -2- Choice of Population Having a restricted eligibility criteria reduces the generalisability to the wider population. For example, if a trial has eligibility criteria that includes speaking English, being 30 to 60 years of age and male, a lot of the Australian population would be excluded and we wouldn’t know whether the treatment is as effective for those people who were excluded. Ethics Ethics requires us to consider the overall risks and benefits of carrying out a study. All human research requires ethical approval from an Ethics Committee. For a trial to be considered ethical, it has to have sound design and be carried out according to a detailed protocol. Researchers and Ethics Committees have to consider the individuals participating in the trials by attempting to minimise harm and maximise the benefit. Researchers are required to ensure that each participant has given their informed consent to participate in the trial. They are also required to truly not know which treatment arm is better, this is called equipoise, although they may have hypotheses. Members of the public want beneficial treatments to be approved as rapidly as possible while avoiding ineffective or harmful treatments. This can be a difficult trade off. Data Monitoring Committee One way to ensure the ethical conduct of a trial is use a Data Monitoring Committee. Data Monitoring Committees are independent advisory groups which meet periodically to review the study. They allow early termination in certain circumstances, and prevents premature termination due to pre-judgement of early unreliable trial results. Minimising Bias and… Minimising bias during a trial is a key part of the quality assurance process which is essential to carry out an ethical trial. Bias can be minimised during the design, by the method of allocation to treatment arm, randomisation, and by blinding, not letting the participant or the researcher know which arm the participant has been allocated to. Bias can also be minimised during the trial by adhering to intervention and control, adherence to the protocol, having high levels of retention and follow-up, and complete and accurate capture of outcome data. Minimising Variability Researchers must also try to minimise variability. The more patients we have in the trial, the more precise the estimate of the treatment effect will be. But if there are too many patients, we may expose more patients than necessary to inferior treatment. Optimal balance achieved by choosing the sample size so that whatever the data obtained, the trial will give an answer to the research question. Hierarchy of Evidence -3- This pyramid shows the level of evidence each type of study gives. At the top is the RCT and systematic reviews, or meta analyses of RCTs. Cancer Research Study Design [End of recorded material] -4-