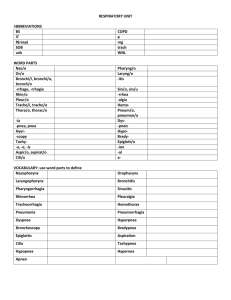
Physiology Ch. 41 p505-513 [4-25
advertisement

Physiology Ch. 41 p505-513 Regulation of Respiration Respiratory Center – composted of neurons located bilaterally in medulla oblongata and pons Divided into three groups: 1. Dorsal Respiratory group – Inspiration 2. Ventral Respiratory group – Expiration 3. Pneumotaxic Center – Rate and depth of breathing Dorsal Respiratory Group of Neurons – most fundamental role in respiration, mostly found in the nucleus of the tractus solitarius (NTS) of medulla (sensory terminal of both CN X and CN IX which transmit signals from peripheral chemoreceptors, baroreceptors, and other receptors in lungs Rhythmical Inspiratory Discharges from Dorsal Respiratory Group – basic rhythm of respiration dictated by dorsal group, which emit repetitive inspiratory action potentials. -Hypothesized to be a set of excitatory neurons which excite a second set, which inhibit the first (repeat) Inspiratory Ramp Signal – nerve signal to inspiratory muscles (diaphragm) is not a single action potential but begins weakly and increases steadily for 2s in normal respiration. -Then the signal ceases for 3s to turn off excitation of diaphragm and allows recoil for expiration -Inspiratory signal begins again for another cycle, again and again -Ramp signal allows for steady increase in volume as opposed to inspiratory gasps Two qualities of Ramp that are controlled: 1. Control of rate of increase of ramp signal – heavy inspiration ramp increases rapidly 2. Control of limiting point at which ramp suddenly ceases, controlling rate of respiration Pneumotaxic Center Limits Duration of Inspiration and Increases Respiratory Rate – located in nucleus parabrachialis in pons transmits signals to inspiratory area -controls “switch-off” point of inspiratory ramp which controls duration of filling phase of lung cycle -strong pneumotaxic signal = less inspiratory time and vice versa -function is to limit respiration and increases rate of breathing consequently Ventral Respiratory Group of Neurons (Inspiration and Expiration) – found in nucleus ambiguus and nucleus retroambiguus -neurons remain inactive during quiet respiration, therefore normal breathing = dorsal neurons -do not participate in basic rhythmical oscillation that controls respiration -when respiratory drives for increased ventilation is > than normal, signals spill into ventral neurons which contribute to the extra drive, used during heavy exercise for overdrive breathing -stimulation of some neurons cause inspiration vs others cause expiration Lung Inflation Signals Limit Respiration (Hering-Breuer Inflation Reflex) – in addition to CNS, sensory nerve signals from lungs control respiration -stretch receptors in walls of bronchi transmit signals through vagal nerves to dorsal respiratory group when lungs become overstretched to “switch-off” inspiration (similar to pneumotaxic center) -this is called the Hering-Breuer Inflation Reflex -also increases rate of respiration similar to pneumotaxic center Control of Overall Respiratory Center Activity – relates to control of ventilation in response to demand Chemical Control of Respiration – goal of respiration is to control O2 CO2 and H+ in tissues, respiratory activity responsive to changes in these concentrations -CO2 and H+ excess act on respiratory center itself to cause greater inspiration -O2 acts on chemoreceptors in carotid and aortic bodies which transmit signal to respiratory center -None of the respiratory centers are directory affected by blood CO2 and H+, but an additional area called the chemosensitive area in the medulla is sensitive to PCO2 or H+ which excite the major areas Excitation of Chemosensitive Neurons by H+ is Primary Stimulus – chemosensitive area is directly affected by H+ ions, but H+ is hard to cross blood brain barrier. CO2 is secondarily exciting this area -CO2 has little effect on chemosensitive area, but it does have an indirect effect: -reacts with H2O to form H2CO3, which dissociates to H+ and HCO3-, and then H+ has effect -Blood brain barrier more permeable to CO2 than H+, so CO2 has a more potent effect -Respiratory center activity is increased very strongly by changes in blood CO2 -CO2 excitation of respiratory center is strong for first few hours, but decreases to 1/5th effect over 1-2 days:: results from renal readjustment of H+ ion concentration by increasing bicarb which bind excess H+ in brain -Therefore, CO2 has strong acute effect on respiration but weak chronic effect after adaptation Changes in O2 have little Direct Effect on Control of Respiratory Center – O2 has no effect on respiratory center but act instead on chemoreceptors -O2 delivery is regular despite changes in ventilation due to hemoglobin system, and so adequate delivery occurs regardless of lung respiration, which is NOT true for CO2 (major controller of respiration) -Lack of O2 causes peripheral chemoreceptor response Peripheral Chemoreceptor System for Control of Respiratory Activity through O2 – these receptors are located outside the brain and are sensitive to changes in O2, but to a lesser extent CO2 and H+ -Most are located in carotid and aortic bodies, and transmit info to the respiratory center 1. Carotid Bodies located in bifurcations of common carotid arteries and transmit signals through CN IX to dorsal respiratory area of medulla 2. Aortic Bodies located along arch of aorta and transmit signals through vagi to the dorsal respiratory area of medulla a. These bodies receive special blood supply from nearby arteries, 20x the total blood flow than the weight of the bodies themselves (only exposed to arterial blood, NOT VENOUS) -Decreased Arterial O2 Stimulates Chemoreceptors – when O2 falls below normal, chemoreceptors are stimulated (particularly sensitive to changes in range of 60-30mmHg -Increased CO2 and H+ Ions Stimulate Chemoreceptors and indirectly increases respiratory activity, however the direct effects of these on the respiratory centers are much more powerful -stimulation of receptors are 5x as fast, yet not as powerful (important during exercise) -Mechanism of stimulation by chemoreceptors happens through gland like cells called glomus cells which synapse directly with nerve endings Effect of Low Arterial PO2 to Stimulate Alveolar Ventilation when Arterial CO2 and H+ are Normal – only the ventilatory drive, due to effect of low O2 on chemoreceptors, is active -no effect on ventilation as long as PO2 in arteries remains above 100mmHg, but lower the ventilation doubles when PO2 is below 60mmHg… Therefore PCO2 and H+ regulate ventilation more than O2 Chronic Breathing of Low O2 Stimulates Respiration More (Acclimatization) – mountain climbers that slowly ascend can withstand lower atmospheric O2 than if they ascend rapidly. Reason for this acclimatization is that respiratory center in brain loses 4/5ths of its sensitivity to PCO2 and H+ -excess ventilatory blow-off of CO2 that would normally inhibit an increase in respiration fails to occur, and low O2 can drive respiratory system to a much higher level of alveolar ventilation Regulation of Respiration During Exercise – O2 and CO2 increase 20x during exercise, and ventilation + metabolic increase in O2 consumption are the same, keeping PO2, PCO2 and H+ normal in arteries. -an increase in ventilation during exercise is caused by the brain transmitting signals to exercising muscles as well as respiratory center at the same time (analogous to vasomotor stimulation during exercise causing increase in arterial pressure) -Therefore, the same time that brain is sending signals to exercising muscles, it sends signals to respiratory center Interrelation Between Chemical Factors and Nervous factors in Control of Respiration During Exercise – occasionally, the nervous control during exercise is too strong or too weak, in which case chemical signals play a significant role in bringing about final adjustment of respiration required to keep oxygen CO2 and H+ normal -at onset of exercise, alveolar ventilation increases instantaneously without an initial increase in PCO2, great enough to initially decrease arterial PCO2 below normal -reason is that brain provides anticipatory signals at onset of exercise to increase alveolar ventilation, but after 30-40 seconds Neurogenic Control of Ventilation during Exercise May be partly a Learned Response – with repeated periods of exercise, the brain becomes progressively more able to provide proper signals to keep blood PCO2 at its normal level (responsible by cerebral cortex) Voluntary Control of Respiration – respiration can be controlled voluntarily and that one can hyper/hypoventilate enough to make serious changes in PCO2, pH, and PO2 Effect of irritant Receptors in the Airways – epithelium of trachea, bronchi, and bronchioles is suppled with nerve endings called pulmonary irritant receptors to cause coughing and sneezing Function of Lung “J” Receptors – Juxtaposition receptors in alveolar walls near pulmonary capillaries are stimulated when capillaries become engorged with blood or when pulmonary edema occurs, may give person feeling of dyspnea Brain Edema Depresses Respiratory Center – activation of respiratory center may be depressed or inactivated by acute brain edema from concussion, alleviated by intravenous injection of hypotonic solutions of mannitol Anesthesia – overdosage with anesthetics causes respiratory depression and arrest (sodium pentobarbital). Periodic Breathing – occurs when person breathes deeply for short interval and then slightly or not at all for an additional interval, repeating. Caused by disease states -Cheyne-Stokes breathing is characterized by waxing and waning respiration between 40-60s Mechanism of Cheyne-Stokes Breathing – when person overbreathes, blowing off too much CO2 from pulmonary blood while at the same time increasing blood oxygen, it takes several seconds before changed pulmonary blood can be transported to the brain and inhibit excess ventilation. -by this time, person has overbreathed for few extra seconds -When blood finally reaches respiratory center, center becomes depressed an excessive amount beginning the opposite cycle – (CO2 increases and O2 decreases_ -basic cause of Cheyne Stokes breathing occurs in everyone, but in normal conditions it is damped.. Damping factors can be overridden: 1. When long delay occurs for transport of blood from lungs to brain, changes CO2 and O2 in alveoli can continue for many more seconds than usual, causing storage capacity for these gases to be exceeded, and Cheyne-Stokes breathing occurs a. Happens in cardiac failure when blood flow is slow 2. Increased negative feedback gain in respiratory control areas causes Cheyne-Stokes breathing. This means that a change on blood CO2 or O2 causes far greater change in ventilation than normal a. Brain feedback tendency for periodic breathing is now strong enough to cause CheyneStokes breathing without extra blood flow delay between lungs and brain i. Happens with brain damage that turns off respiratory drive entirely for a few seconds, then an extra intense increase in blood CO2 turns it back on with great force Sleep Apnea – means absence of spontaneous breathing during sleep lasting 10s or longer 300-500 times per night, can be caused by obstruction of upper airways, pharynx, or impaired central nervous system respiratory drive Obstructive Sleep Apnea is Caused by Blockage of Upper Airway – During sleep, muscles that normally keep passage open to allow air to flow into lungs during inspiration relax, but the airway passage remains open enough to permit adequate flow of air. -some people have narrow passage, and relaxation of muscles can cause pharynx to completely close -loud snoring and labored breathing occur in patients with sleep apnea after falling asleep. -Followed by period of silence where no breathing occurs, followed by gasps of air and snoring again -Periods of apnea result in increases in PCO2 which greatly stimulate respiration -Patients with sleep apnea have excessive daytime drowsiness, increased sympathetic activity, high heart rates, pulmonary and systemic hypertension, and risk for cardiovascular disease -occurs in older or obese persons with more fat masses in the neck -can be associated with nasal obstruction, large tongue, tonsils, or certain palate shapes -surgery can be done to remove fat tissue, nasal ventilation Central Sleep Apnea Occurs When Neural Drive to Respiratory Musclesis Transiently Absent – some people have ceased CNS drive to ventilatory muscles during sleep -damage to central respiratory centers or abnormalities of respiratory neuromuscular junctions -may have decreased ventilation when they are awake as well, but voluntary breathing is normal -worsen during sleep, increasing apnea and decreasing PO2 and increasing PCO2 until critical level is reached