File - Jessa Pamaran HCPNS
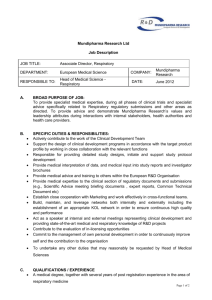
advertisement

Running head: POOR OXYGEN SATURATION LEVEL FOLLOWING LAMINECTOMY Complex Issues and Patient Safety Jessa Pamaran 821417797 Humber College March 16, 2015 The human body is known to work as a whole. In the health care field, patients are being taken care of holistically because one affected part of the body can affect all. People have different POOR OXYGEN SATURATION LEVEL FOLLOWING LAMINECTOMY norms based on lifestyle or culture. These norms and baselines, also called as vital signs, are what the health care providers use to assess if the patients’ body systems are functioning effectively (Perry and Potter, 2014). When results from vital signs are not within its normal ranges, it is when a person’s body is not within its physiological state, so nurses can intervene and plan of care is introduced. In addition, vital signs are one of the significant data that health care providers value especially in the post anesthesia care unit or PACU. Nurses can compare patients’ vital signs prior the surgery and after. There are different measures of vital signs: blood pressure, pulse rate, respiratory rate, temperature, oxygen saturation level, and pain. A patent airway is one of the priorities that the health care team focus on to refrain risks of further complications (Karcz and Papadakos, 2013). It is crucial that patients are to have an adequate amount of gas exchange especially during post op because most of the patients are immobilized. Post op patients can breathe in a limited manner depending on the anesthesia used during surgery that alters pulmonary function (Karcz and Papadakos, 2013). In this paper, I will be focusing on how nurses can intervene when oxygen saturation level is measured as less than a human’s normal range. It is critically important in post-operative period to monitor the patients’ respiratory status. In the post anesthesia care unit or PACU, respiratory complications are considered a major cause of mortality of post-op patients (Karcz and Papadakos, 2013). The anesthesia being used by the surgeons impairs lung function due to lack of stimulation, and even affects normal individuals (Karcz and Papadakos, 2013). It is crucial for the nurse to take a set of vital signs pre-op and postop, giving special attention to O2 saturation result, prior implementing sufficient oxygenation especially to post op patients. There are few approaches when a nurse can intervene in providing adequate oxygenation. 2 POOR OXYGEN SATURATION LEVEL FOLLOWING LAMINECTOMY First, the nurse can encourage the patient to do some coughing and deep breathing exercises, i.e. pursed lip breathing, to remove retained anesthetic gases (Lewis, 2014). Based on the case scenario given, hyperventilation is present which can be a lead factor for hypoxia. Deep breathing exercises can help the patient regain his or her normal breathing pattern and lung expansion. Coughing is also encouraged to release any secretions if there is an accumulation of fluid in the lungs present (Perry and Potter, 2014). Accumulation of fluid in the lungs can lead to more severe respiratory complications; therefore, positioning the patient in a lateral “recovery” or side-lying position helps the patient to have a full chest expansion (Lewis, 2014). The patient’s position is to be changed every one to two hours to gain perfusion of both lungs and to avoid pressure ulcers while keeping spine alignment (Harvey, 2005). This also helps the nurse to assess the incision site for any drainage or signs of infection following laminectomy. Another approach to provide adequate oxygenation is by encouraging the patient to use an incentive spirometer at least ten deep breaths every hour (Harvey, 2005). The incentive spirometer helps the patient achieve their baseline inspiratory volume on the device (Perry and Potter, 2014). The use of incentive spirometer is another way of performing a deep breathing exercise, and is mainly necessary especially if there is a language barrier present between the nurse and the patient. Furthermore, another approach to ease hypoxia is oxygen therapy as per doctor’s order to provide comfort and amount of oxygen needed (Perry and Potter, 2014). The oxygen can be administered via nasal cannula or face mask. These routes are considered as low-flow systems in a sense that they deliver oxygen that is below 6L/minute (Perry and Potter, 2014). It is advisable to keep the oxygen concentration based on patient’s respiratory pattern to avoid drying of the mucosa and to keep the oxygen concentration as low as possible unless contraindicated (Perry and Potter, 2014). Monitoring of SpO2 via pulse oximetry is to be continued to ensure sufficient oxygen 3 POOR OXYGEN SATURATION LEVEL FOLLOWING LAMINECTOMY administration. Lastly, consulting the surgeon or a respiratory therapist is the best option especially if symptoms worsen. The surgeon may prescribe an opioid analgesic knowing that the patient is in pain following laminectomy. An opioid analgesic is often used with post op patients who have moderate to severe pain (Lewis, 2014). The opioid analgesic can help calm the patient, which results to respiratory rate to drop back to the patient’s baseline and the oxygen saturation level to increase at least up to 95% on room air. The respiratory therapist is also needed to help in maintaining a patent airway for the post op patient and maintenance of mechanical ventilator if present (Harvey, 2005). To sum it up, postoperative care is highly essential because it is the period when patients start to heal. Vital signs is the best way to gather information from the patients as to whether they handled the surgery well. The patients have been exposed to multiple risks during surgery and close monitoring for complications, especially respiratory complications as they heal is valuable (Lewis, 2014). Nurses should monitor patients and compare pre op and post op baseline levels to ensure desired healing process. Patients’ comfort should always be a priority to avoid risks of harm and a patient-centered care approach should always be manifested. It is also the nurses’ job to provide patient teaching especially when patients are close to being discharged (Lewis, 2014). References: 4 POOR OXYGEN SATURATION LEVEL FOLLOWING LAMINECTOMY Harvey, C. (2005). Spinal surgery patient care. Orthopedic Nursing, 24(6), 437. Karcz, M., & Papadakos, P.J. (2013). Respiratory complications in the post anesthesia care unit: A review of pathophysiological mechanisms. Canadian Journal of Respiratory Therapy, 49(4), 21-29. Lewis, S., Dirksen, S., Heitkemper, M., Bucher, L., & Camera, I. (2014). Medical-Surgical Nursing in Canada. Assessment and Management of Clinical Problems (3rd ed.). Toronto: Elsevier Canada. Perry, A. G., & Potter, P. (2014). Fundamentals of Nursing (5th ed.). Toronto: Elsevier Canada. 5