Online Appendix for the following JACC article TITLE
advertisement

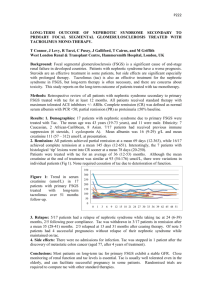
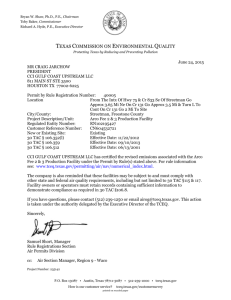
Online Appendix for the following JACC article TITLE: Cardioprotective Effect of 3 Adrenergic Receptor Agonism: Role of Neuronal Nitric Oxide Synthase AUTHORS: Xiaolin Niu, MD, PHD, Vabren L. Watts, PHD, Oscar H. Cingolani, MD, Vidhya Sivakumaran, PHD, Jordan S. Leyton-Mange, MD, Carla L. Ellis, MD, Karen L. Miller, Konrad Vandegaer, BS, Djahida Bedja, Kathleen L. Gabrielson, DVM, PHD, Nazareno Paolocci, MD, David A. Kass, MD, Lili A. Barouch, MD APPENDIX Expanded Methods Experimental model Under anesthesia with 2% isoflurane, C57BL/6J male mice (9-10 weeks old, Jackson Laboratory, Bar Harbor, ME) chests were opened through a lateral thoracic window between ribs 2 and 4, and a 27G needle was placed beside the transverse aorta. nNOS-/-/B6129S male mice (9-10 weeks old, Jackson Laboratory, Bar Harbor, ME) underwent parallel procedures. The band was secured using a 7.0 prolene suture, and the needle was then removed and the chest was closed. The remaining third were exposed to sham surgery as control, using the same procedure as TAC without binding the aorta. Half of the TAC mice were treated with BRL (Tocris Bioscience, Ellisville, Missouri) at 0.1 mg/kg/hour via osmotic minipumps (Alzet Inc, Cupertino, CA) which were subcutaneously implanted one day post TAC. The other half of TAC mice received osmotic pumps containing only vehicle (PBS). All animals underwent echocardiography after 1 and 3 weeks. Myocardial tissue was either preserved in 10% formalin or snapfrozen in liquid nitrogen for subsequent analysis. Mice were housed in a university animal facility with a 12-hour light-dark cycle and allowed water and food ad libitum. Animal treatment and care was provided in accordance with institutional guidelines. The institutional Animal Care and Use Committee of the Johns Hopkins University School of Medicine approved all protocols and experimental procedures. Cardiac function and geometry M-mode left ventricular (LV) end-systolic and end-diastolic cross-sectional diameter (LVESD, LVEDD), and the mean of septal and posterior wall thicknesses were determined from an average of 3-5 beats. Left ventricular (LV) fractional shortening (FS%) and calculated LV mass were determined using a cylindrical model as previously described (16). Echocardiography was evaluated by investigators blinded to the different treatment groups. Histological evaluation and cellular morphometry Myocyte cross-sectional diameter was determined from digitized images of hematoxylin and eosin (H&E) stained slides and analyzed using Image J program (NIH, Bethesda, MD). Myocardial fibrosis was determined by Masson trichrome staining and was scored by a pathologist blinded as to tissue source using a semi-quantitative scale (0= absent; 3= severe fibrosis). Average data reflect results from 3-4 hearts in each group. Measurement of cardiac superoxide generation Lucigenin-enhanced chemiluminescence Fresh-frozen myocardium was homogenized in 20 mM HEPES buffer containing 1 tablet of mini EDTAfree protease inhibitor cocktail (Roche, Indianapolis, IN) and 1 mM PMSF (Roche), then centrifuged at 800g for 10 minutes at 4oC to get the supernatant. Supernatants (from at least 4.77 mg tissue) were loaded with Krebs-HEPES buffer (120 mM NaCl, 4.7 mM KCl, 1.2 mM MgSO4, 1.2 mM KH2PO4, 2.5 mM CaCl2, 25 mM NaHCO3, 20mM Hepes and 5.5 mM glucose), 5 M lucigenin (Sigma Aldrich, St. Louis, MO) and 100 uM nicotinamide adenine dinucleotide phosphate (NADPH, Sigma Aldrich) to the liquid scintillation counter (LS6000IC, Beckman Instruments, Fullerton, CA). Signals were recorded as counts per minute (CPM) and data were normalized to the weight of loaded tissue as CPM/mg tissue. In the same experiment, another aliquot of each lysate was pre-incubated with 100 M potent nNOS specific inhibitor Vinyl-L-NIO (L-VNIO, Cayman Chemical, Ann Arbor, Michigan) for 30 minutes at 4oC to determine the superoxide generation by acute inhibition of nNOS. Electron Paramagnetic Resonance Fresh-frozen myocardium was homogenized in 1X PBS buffer containing 0.1mM DTPA (Sigma Aldrich). Samples were diluted to the 1 mg/mL in 1x PBS and treated with 1 mM 1-hydroxy-3methoxycarbonyl-2,2,5,5-tetramethyl pyrrolidine (CMH, Enzo Life Sciences) for 10 minutes. Stock solutions (10 mM) of CMH were made in nitrogen purged 0.9% (w/v) NaCl, 25 g/L Chelex 100 (BioRad) and 0.1 mM DTPA(18). Samples were assayed in 50 µL glass capillary tubes at room temperature using the Bruker E-Scan EPR spectrometer. Spectrometer settings were as follows: sweep width, 100 G; microwave frequency, 9.75 GHz; modulation amplitude, 1 G; conversion time, 5.12 ms; time constant 5.12 ms; receiver gain, 2 x 102; number of scans, 4. Western blot analysis Snap-frozen LV tissue was homogenized in cell lysis buffer (Cell Signaling Technology, Danvers, MA) with 0.01% phosphatase inhibitor cocktails (Sigma), 1 tablet of mini EDTA-free protease inhibitor cocktail and protease inhibitor PMSF (1 mM Roche). 60 µg heated protein was separated on 4-12% BisTris NuPAGE Novex mini gel (Invitrogen, Carlsbad, CA), electrophoresed and transferred to a PVDF membrane. Phosphospecific antibodies eNOS-Ser1177 (1:1000) and -Ser114 (1:1000) were purchased from Cell Signaling Technology (Lake Placid, NY), and p-eNOS Thr495 (1:1000) from BD Biosciences (San Jose, CA). eNOS (1:1000), iNOS (1:500), nNOS (1:500), and GAPDH, 1:10000 were purchased from Santa Cruz Biotechnology). The densitometric volume of digitalized band was evaluated by Image J program. Low-temperature SDS-PAGE was performed to determine eNOS monomer-to-dimer ratio. 50 µg of protein with 5-fold Laemmli buffer (0.32 M Tris-HCl, pH 6.8, 0.5 M glycine, 10% SDS, 50% glycerol, and 0.03% bromophenol blue) was loaded onto a 7.5% Tris-Glycine ready gel (Bio-Rad) and run on ice at 100 Volts for 5 hours at 4°C. Then, protein was transferred to PVDF on ice under 14 Volts overnight at 4°C Subsequent procedures were as same as the regular Western blot. Results Appendix Figure 1. Effect of BRL on LV hypertrophy in TAC mice. (A) Increased heart weight to body weight ratio caused by 3 weeks of TAC was reduced by BRL treatment. This effect was independent of body weight. (B) Examples of Masson trichrome stain demonstrating increased fibrosis by 3 weeks of TAC (400x). (C) Summary data of increased myocyte diameter (left) and fibrosis scale (semi-quantitative scoring system; 0=none, 3=marked fibrosis; right) by 3 weeks of TAC. BRL reduced the myocyte diameter but had no change in fibrosis scale. *P<0.05 vs. sham; †P<0.05 vs. TAC. A * 30 *† 100 50 Body weight (g) Heart weight/ Tibia length (mg/cm) 150 20 10 0 0 SHAM TAC SHAM TAC-BRL B TAC TAC-BRL C SHAM Myocyte width(μm) 20 TAC * 15 *† 10 5 0 Sham TAC TAC-BRL Fibrosis (0-3 scale) 2.5 TAC-BRL * 2.0 * 1.5 1.0 0.5 100m 0.0 SHAM TAC TAC-BRL Appendix Figure 2. No changes in eNOS-Thr95 phosphorylation or iNOS expression by BRL treatment. (A) p-eNOS Thr495/eNOS and total eNOS expression were unchanged between sham, TAC and TAC-BRL groups. (B) iNOS protein expression was unchanged by BRL treatment. A SHAM TAC Thr495 TAC-BRL 0.4 p-eNOS/total eNOS total NOS GAPDH total eNOS/GAPDH 2.5 p-eNOS Thr495 2.0 1.5 1.0 0.5 0.0 SHAM B SHAM iNOS GAPDH TAC TAC-BRL TAC TAC-BRL 0.3 0.2 0.1 0.0 SHAM TAC TAC-BRL