PRIORITY NURSING DIAGNOSIS Impaired skin integrity r/t impaired
advertisement
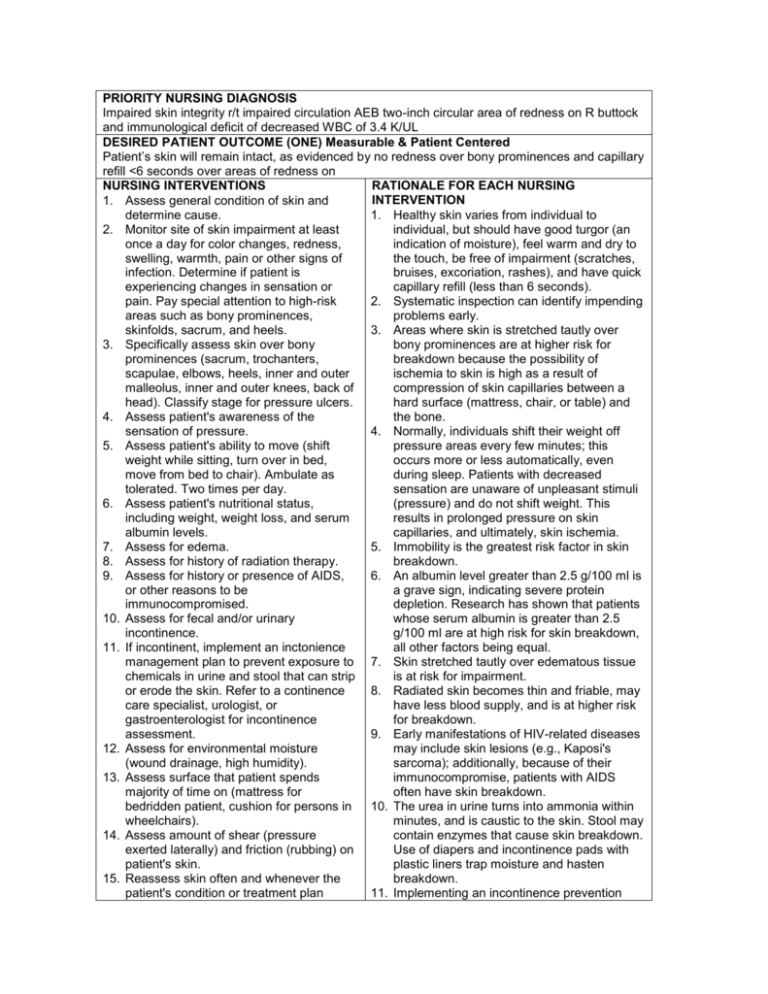
PRIORITY NURSING DIAGNOSIS Impaired skin integrity r/t impaired circulation AEB two-inch circular area of redness on R buttock and immunological deficit of decreased WBC of 3.4 K/UL DESIRED PATIENT OUTCOME (ONE) Measurable & Patient Centered Patient’s skin will remain intact, as evidenced by no redness over bony prominences and capillary refill <6 seconds over areas of redness on NURSING INTERVENTIONS RATIONALE FOR EACH NURSING INTERVENTION 1. Assess general condition of skin and determine cause. 1. Healthy skin varies from individual to 2. Monitor site of skin impairment at least individual, but should have good turgor (an once a day for color changes, redness, indication of moisture), feel warm and dry to swelling, warmth, pain or other signs of the touch, be free of impairment (scratches, infection. Determine if patient is bruises, excoriation, rashes), and have quick experiencing changes in sensation or capillary refill (less than 6 seconds). pain. Pay special attention to high-risk 2. Systematic inspection can identify impending areas such as bony prominences, problems early. skinfolds, sacrum, and heels. 3. Areas where skin is stretched tautly over 3. Specifically assess skin over bony bony prominences are at higher risk for prominences (sacrum, trochanters, breakdown because the possibility of scapulae, elbows, heels, inner and outer ischemia to skin is high as a result of malleolus, inner and outer knees, back of compression of skin capillaries between a head). Classify stage for pressure ulcers. hard surface (mattress, chair, or table) and 4. Assess patient's awareness of the the bone. sensation of pressure. 4. Normally, individuals shift their weight off 5. Assess patient's ability to move (shift pressure areas every few minutes; this weight while sitting, turn over in bed, occurs more or less automatically, even move from bed to chair). Ambulate as during sleep. Patients with decreased tolerated. Two times per day. sensation are unaware of unpleasant stimuli 6. Assess patient's nutritional status, (pressure) and do not shift weight. This including weight, weight loss, and serum results in prolonged pressure on skin albumin levels. capillaries, and ultimately, skin ischemia. 7. Assess for edema. 5. Immobility is the greatest risk factor in skin 8. Assess for history of radiation therapy. breakdown. 9. Assess for history or presence of AIDS, 6. An albumin level greater than 2.5 g/100 ml is or other reasons to be a grave sign, indicating severe protein immunocompromised. depletion. Research has shown that patients 10. Assess for fecal and/or urinary whose serum albumin is greater than 2.5 incontinence. g/100 ml are at high risk for skin breakdown, 11. If incontinent, implement an inctonience all other factors being equal. management plan to prevent exposure to 7. Skin stretched tautly over edematous tissue chemicals in urine and stool that can strip is at risk for impairment. or erode the skin. Refer to a continence 8. Radiated skin becomes thin and friable, may care specialist, urologist, or have less blood supply, and is at higher risk gastroenterologist for incontinence for breakdown. assessment. 9. Early manifestations of HIV-related diseases 12. Assess for environmental moisture may include skin lesions (e.g., Kaposi's (wound drainage, high humidity). sarcoma); additionally, because of their 13. Assess surface that patient spends immunocompromise, patients with AIDS majority of time on (mattress for often have skin breakdown. bedridden patient, cushion for persons in 10. The urea in urine turns into ammonia within wheelchairs). minutes, and is caustic to the skin. Stool may 14. Assess amount of shear (pressure contain enzymes that cause skin breakdown. exerted laterally) and friction (rubbing) on Use of diapers and incontinence pads with patient's skin. plastic liners trap moisture and hasten 15. Reassess skin often and whenever the breakdown. patient's condition or treatment plan 11. Implementing an incontinence prevention 16. 17. 18. 19. 20. 21. 22. 23. 24. results in an increased number of risk factors. Monitor client’s skin care practices, noting type of soap or other cleansing agents used, temperature of water, and frequency of skin cleansing. Individualize plan according to the client’s skin condition, needs, and preferences. For clients with limited mobility, use a risk assessment tool to systematically assess immobility-related risk factors. DO not position patient on site of skin impairment. If consistent with overall client management goals, turn and position the client at least every 2 hours. Transfer the client with care to protect against adverse effects of external mechanical forces such as friction, pressure, and shear. Evaluate for use of specialty mattress, beds, or devices as appropriate. Maintain the HOB at the lowest possible degree of elevation to reduce shear and friction, and use lift devises, pillows, foam wedges, and pressure-reducing devices in bed. Implement a written treatment plan for topical treatment of the site of skin impairment. Select a topical treatment that will maintain a moist wound-healing environment and that is balanced with the need to absorb exudate. Avoid massaging around site of skin impairment and over bony prominences. Teach skin to use pillows, foam wedges and pressure-reducing devices to prevent pressure injury. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. plan with the use of skin protectant or a cleanser protectant can significantly decrease skin breakdown and pressure ulcer formation. That may contribute to skin maceration. Patients who spend the majority of time on one surface need a pressure reduction or pressure relief device to distribute pressure more evenly and lessen the risk for breakdown. A common cause of shear is elevating the head of the patient's bed; the body's weight is shifted downward onto the patient's sacrum. Common causes of friction include the patient rubbing heels or elbows against bed linen and moving the patient up in bed without the use of a lift sheet. The incidence and onset of skin breakdown is directly related to the number of risk factors present. Cleansing should not compromise the skin. Avoid harsh cleansing agents, hot water, extreme friction or force, or cleansing too frequency. A validated risk assessment tool such as Braden scale should be used to identify clients at risk for immobility related skin breakdown. DO not position an individual directly on a pressure ulcer. Continue to turn/reposition the individual regardless of the support surface in use. Establish turning frequency based on the characteristics of the support surface and the individual’s response. Having the appropriate mattress and use of pillows to elevate and separate pressure spots can reduce pressure ulcers. A written plan ensures consistency in care and documentation. Choose dressings that provide a moist environment, keep periwound skin dry, and control exudate and eliminate dead space. Research suggests that massage may lead to deep-tissue trauma. The use of effective pressure-reducing seat cushions for elderly wheelchair users significantly prevented sitting-acquired pressure ulcers.