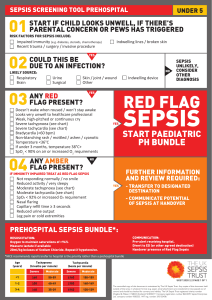
Paediatric SIRS Vital Signs
advertisement

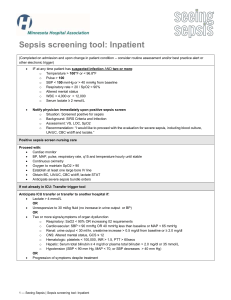
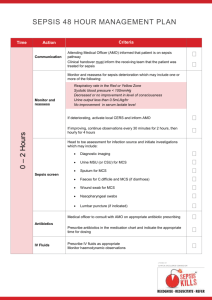
Pediatric SIRS Vital Signs: Poor Predictor of Need for Critical Care Retrospective study of children <18 years of age presenting to a pediatric emergency department Systemic inflammatory response syndrome vital signs identified only 23% of children requiring ventilation or vasoactive agents. SIRS vital signs were defined as abnormal temperature (<36°C or >38.5°C) plus tachycardia or tachypnea (>2 mean standard deviations, adjusted for age). Temperature-corrected heart rate (10 beats/minute subtracted for each 1°C over 38.5°C) which is still tachycardic is a useful indicator of sepsis More important than identifying any one specific vital sign abnormality is tracking vital signs after rehydration and antipyretic therapy Consider sepsis in any child who has persistent tachypnea or tachycardia despite temperature normalisation. Reference Katherine Bakes, MD reviewing Scott HF et al. Acad Emerg Med 2015 Apr WSHT Sepsis Screening tool To be used for ALL unwell children presenting to the ED Could this child have sepsis? Look for: Tick Recognise Temperature <36 oC or >38.5oC Value o Tachycardia (use age appropriate PEWS chart) <1yr 1-5yrs 6-11yrs 12-16 16+ >180 >140 >120 >100 >90 Altered mental state: Sleepy, floppy, lethargic or irritable Mottled skin, or prolonged capillary refill time or ‘flash’ capillary refill time /min Suspected site/source: If 3 criteria present: THINK SEPSIS: This is a clinical emergency Bleep Paediatric Team If not: Sepsis unlikely, explore other causes : Time / Date : C Sign : Respond Paediatric Sepsis 6: Achieve the following within 1 hour - Refer to SORT sepsis pathway (www.strs.nhs.uk or www.sort.nhs.uk) 1 2 3 4 5 Reassess 6 R1 R2 R3 Time Sign Give High Flow Oxygen Record Blood Pressure and start urine collection (fresh nappy) Obtain iv/io access Take blood cultures, blood gas (include glucose & lactate) Give Ceftriaxone 80mg/kg Think: If neutropaenic, immunocompromised or a neonate, refer to local guidance Fluid Resuscitation if required - 20ml/kg 0.9% Saline, reassess, repeat as needed Within 1 hour of treatment Persistent abnormal physiological parameters (HR, RR, CRT) Lactate >2 Signs of fluid overload ( hepatomegaly, desaturations, crepitations) Yes/No If “Yes” to any of above (R1-3) - escalate care to Paediatric and A&E Consultant, Anaesthetist Also contact South Thames Retrieval Service (STRS) or SORT Tel - (STRS): 020 7188 5000 If patient stabilised – admit to ward / HDU, review with at least hourly observations for at least 4 hours