Adult ICU Delirium Guideline (University of Rochester
advertisement
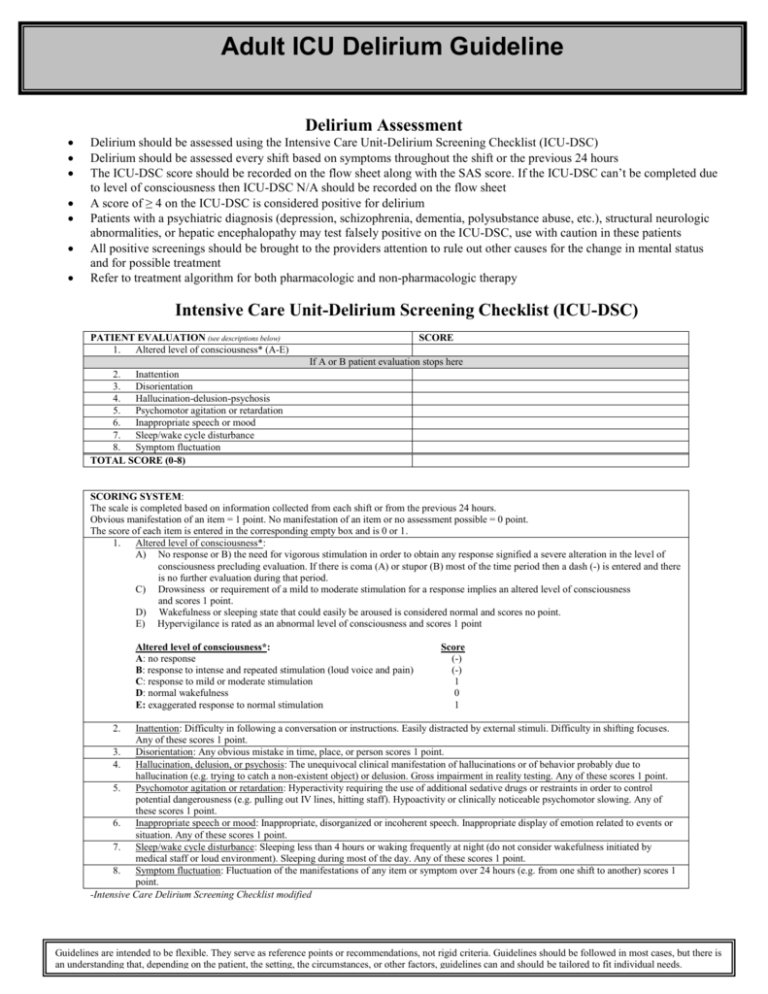
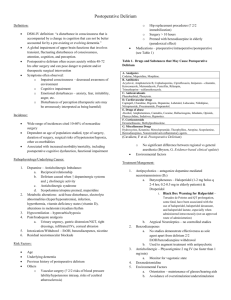
Adult ICU Delirium Guideline Delirium Assessment Delirium should be assessed using the Intensive Care Unit-Delirium Screening Checklist (ICU-DSC) Delirium should be assessed every shift based on symptoms throughout the shift or the previous 24 hours The ICU-DSC score should be recorded on the flow sheet along with the SAS score. If the ICU-DSC can’t be completed due to level of consciousness then ICU-DSC N/A should be recorded on the flow sheet A score of ≥ 4 on the ICU-DSC is considered positive for delirium Patients with a psychiatric diagnosis (depression, schizophrenia, dementia, polysubstance abuse, etc.), structural neurologic abnormalities, or hepatic encephalopathy may test falsely positive on the ICU-DSC, use with caution in these patients All positive screenings should be brought to the providers attention to rule out other causes for the change in mental status and for possible treatment Refer to treatment algorithm for both pharmacologic and non-pharmacologic therapy Intensive Care Unit-Delirium Screening Checklist (ICU-DSC) PATIENT EVALUATION (see descriptions below) 1. Altered level of consciousness* (A-E) SCORE If A or B patient evaluation stops here 2. Inattention 3. Disorientation 4. Hallucination-delusion-psychosis 5. Psychomotor agitation or retardation 6. Inappropriate speech or mood 7. Sleep/wake cycle disturbance 8. Symptom fluctuation TOTAL SCORE (0-8) SCORING SYSTEM: The scale is completed based on information collected from each shift or from the previous 24 hours. Obvious manifestation of an item = 1 point. No manifestation of an item or no assessment possible = 0 point. The score of each item is entered in the corresponding empty box and is 0 or 1. 1. Altered level of consciousness*: A) No response or B) the need for vigorous stimulation in order to obtain any response signified a severe alteration in the level of consciousness precluding evaluation. If there is coma (A) or stupor (B) most of the time period then a dash (-) is entered and there is no further evaluation during that period. C) Drowsiness or requirement of a mild to moderate stimulation for a response implies an altered level of consciousness and scores 1 point. D) Wakefulness or sleeping state that could easily be aroused is considered normal and scores no point. E) Hypervigilance is rated as an abnormal level of consciousness and scores 1 point Altered level of consciousness*: A: no response B: response to intense and repeated stimulation (loud voice and pain) C: response to mild or moderate stimulation D: normal wakefulness E: exaggerated response to normal stimulation Score (-) (-) 1 0 1 2. Inattention: Difficulty in following a conversation or instructions. Easily distracted by external stimuli. Difficulty in shifting focuses. Any of these scores 1 point. 3. Disorientation: Any obvious mistake in time, place, or person scores 1 point. 4. Hallucination, delusion, or psychosis: The unequivocal clinical manifestation of hallucinations or of behavior probably due to hallucination (e.g. trying to catch a non-existent object) or delusion. Gross impairment in reality testing. Any of these scores 1 point. 5. Psychomotor agitation or retardation: Hyperactivity requiring the use of additional sedative drugs or restraints in order to control potential dangerousness (e.g. pulling out IV lines, hitting staff). Hypoactivity or clinically noticeable psychomotor slowing. Any of these scores 1 point. 6. Inappropriate speech or mood: Inappropriate, disorganized or incoherent speech. Inappropriate display of emotion related to events or situation. Any of these scores 1 point. 7. Sleep/wake cycle disturbance: Sleeping less than 4 hours or waking frequently at night (do not consider wakefulness initiated by medical staff or loud environment). Sleeping during most of the day. Any of these scores 1 point. 8. Symptom fluctuation: Fluctuation of the manifestations of any item or symptom over 24 hours (e.g. from one shift to another) scores 1 point. -Intensive Care Delirium Screening Checklist modified Guidelines are intended to be flexible. They serve as reference points or recommendations, not rigid criteria. Guidelines should be followed in most cases, but there is an understanding that, depending on the patient, the setting, the circumstances, or other factors, guidelines can and should be tailored to fit individual needs. TREATMENT ALGORITHM Is the Patient Delirious (ICU-DSC positive (Score ≥4))? (See Delirium Assessment) NO Reassess for delirium every shift Treat pain and anxiety YES Consider differential diagnosis to r/o other causes for change in mental status e.g. Sepsis, CHF, metabolic disturbances Remove deliriogenic drugs1 Non-pharmacological therapy2 SAS of 6 to 7 SAS of 4 to 5 Is the patient in pain? YES Give analgesic (See pain guideline) Assure adequate pain control Reassess target sedation goal (See pain guideline) (See sedation guidelines) NO Consider antipsychotic3 Give adequate sedative for safety then minimize and/or Consider treatment for *Acute Delirium*3 1. DELIRIOGENIC MEDICATIONS Consider stopping or substituting for: -Benzodiazepines -Corticosteroids -Metoclopramide -H2 Antagonists -Anticholinergics -Promethazine -Diphenhydramine 3. ANTIPSYCHOTIC THERAPY While tapering or discontinuing sedatives, consider: -Haloperidol 5 mg IV/PO q6h, increase dose by 5 mg to max of 20 mg q6h (consider lower starting dose in elderly patients) -Quetiapine 50-400 mg/day PO divided twice daily -Olanzapine 2.5-20 mg/day PO divided once or twice daily Haloperidol 1-10mg IV q2h prn can be used for breakthrough symptoms *Acute Delirium* Haloperidol 3-5 mg IV x1 for acute delirium (ICU-DSC positive and SAS of 6 to 7) SAS of 2 to 3 Double previous Haloperidol dose every 20 minutes until patient controlled or maximum dose of 40 mg is reached Haloperidol maintenance dose is 25% of total dose given to control agitation every six hours Monitor QTc daily if on a scheduled antipsychotic regimen -Hold if QTc is > 0.5 msec Discontinue antipsychotics if high fever, QTC prolongation, or drug- 2. NON-PHARMACOLOGIC THERAPY Orientation Provide visual and hearing aids Encourage communication and reorient patients Have familiar objects in the room Attempt consistency in nursing staff Allow television during day with daily news Non-verbal music Environment Sleep hygiene: Lights off at night, on during day Control excess noise at night Ambulate and mobilize early and often Clinical Parameters Maintain systolic blood pressure >90 mmHg Maintain oxygen saturations >90% Treat underlying metabolic derangements and infections induced rigidity occurs Prepared by C. Groth, Adapted from ICUdelirium.org Last updated 10/2010 Guidelines are intended to be flexible. They serve as reference points or recommendations, not rigid criteria. Guidelines should be followed in most cases, but there is an understanding that, depending on the patient, the setting, the circumstances, or other factors, guidelines can and should be tailored to fit individual needs.