Postoperative Delirium
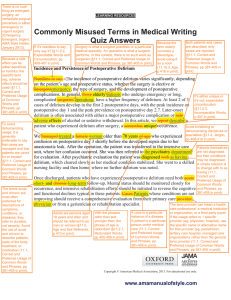
advertisement
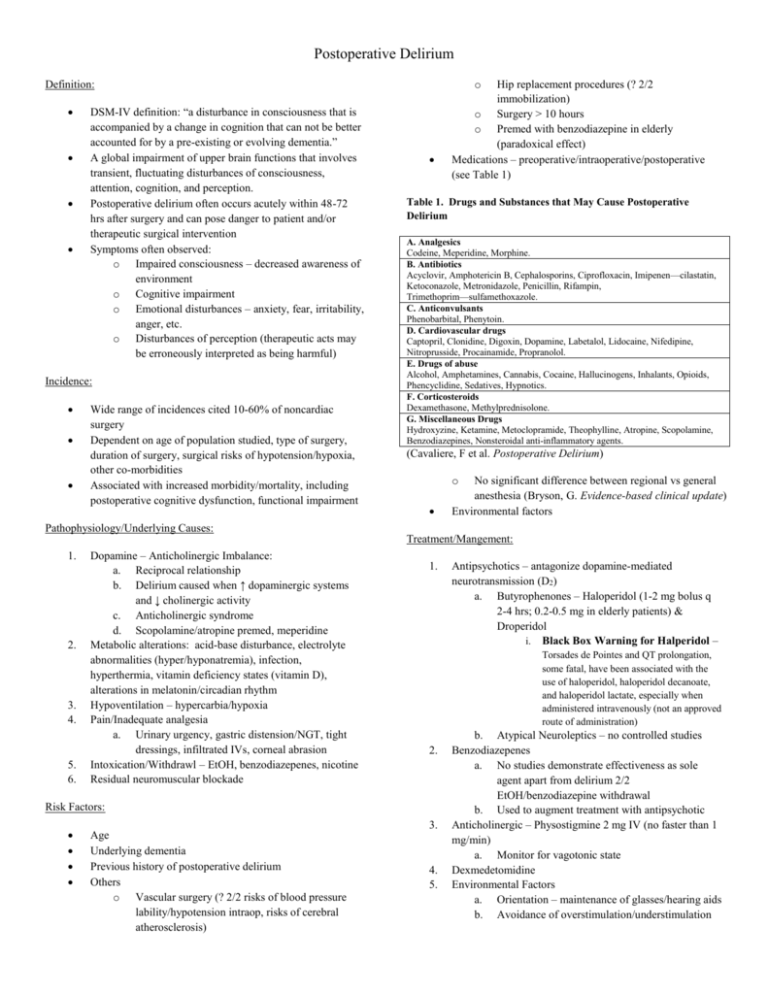
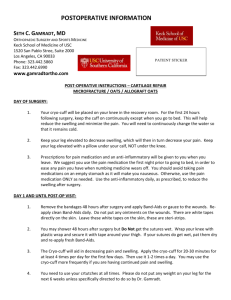
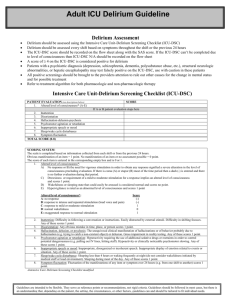
Postoperative Delirium o Definition: DSM-IV definition: “a disturbance in consciousness that is accompanied by a change in cognition that can not be better accounted for by a pre-existing or evolving dementia.” A global impairment of upper brain functions that involves transient, fluctuating disturbances of consciousness, attention, cognition, and perception. Postoperative delirium often occurs acutely within 48-72 hrs after surgery and can pose danger to patient and/or therapeutic surgical intervention Symptoms often observed: o Impaired consciousness – decreased awareness of environment o Cognitive impairment o Emotional disturbances – anxiety, fear, irritability, anger, etc. o Disturbances of perception (therapeutic acts may be erroneously interpreted as being harmful) Incidence: Wide range of incidences cited 10-60% of noncardiac surgery Dependent on age of population studied, type of surgery, duration of surgery, surgical risks of hypotension/hypoxia, other co-morbidities Associated with increased morbidity/mortality, including postoperative cognitive dysfunction, functional impairment Hip replacement procedures (? 2/2 immobilization) o Surgery > 10 hours o Premed with benzodiazepine in elderly (paradoxical effect) Medications – preoperative/intraoperative/postoperative (see Table 1) Table 1. Drugs and Substances that May Cause Postoperative Delirium A. Analgesics Codeine, Meperidine, Morphine. B. Antibiotics Acyclovir, Amphotericin B, Cephalosporins, Ciprofloxacin, Imipenen—cilastatin, Ketoconazole, Metronidazole, Penicillin, Rifampin, Trimethoprim—sulfamethoxazole. C. Anticonvulsants Phenobarbital, Phenytoin. D. Cardiovascular drugs Captopril, Clonidine, Digoxin, Dopamine, Labetalol, Lidocaine, Nifedipine, Nitroprusside, Procainamide, Propranolol. E. Drugs of abuse Alcohol, Amphetamines, Cannabis, Cocaine, Hallucinogens, Inhalants, Opioids, Phencyclidine, Sedatives, Hypnotics. F. Corticosteroids Dexamethasone, Methylprednisolone. G. Miscellaneous Drugs Hydroxyzine, Ketamine, Metoclopramide, Theophylline, Atropine, Scopolamine, Benzodiazepines, Nonsteroidal anti-inflammatory agents. (Cavaliere, F et al. Postoperative Delirium) o No significant difference between regional vs general anesthesia (Bryson, G. Evidence-based clinical update) Environmental factors Pathophysiology/Underlying Causes: Treatment/Mangement: 1. 2. 3. 4. 5. 6. Dopamine – Anticholinergic Imbalance: a. Reciprocal relationship b. Delirium caused when ↑ dopaminergic systems and ↓ cholinergic activity c. Anticholinergic syndrome d. Scopolamine/atropine premed, meperidine Metabolic alterations: acid-base disturbance, electrolyte abnormalities (hyper/hyponatremia), infection, hyperthermia, vitamin deficiency states (vitamin D), alterations in melatonin/circadian rhythm Hypoventilation – hypercarbia/hypoxia Pain/Inadequate analgesia a. Urinary urgency, gastric distension/NGT, tight dressings, infiltrated IVs, corneal abrasion Intoxication/Withdrawl – EtOH, benzodiazepenes, nicotine Residual neuromuscular blockade 1. Torsades de Pointes and QT prolongation, some fatal, have been associated with the use of haloperidol, haloperidol decanoate, and haloperidol lactate, especially when administered intravenously (not an approved route of administration) 2. Risk Factors: 3. Age Underlying dementia Previous history of postoperative delirium Others o Vascular surgery (? 2/2 risks of blood pressure lability/hypotension intraop, risks of cerebral atherosclerosis) Antipsychotics – antagonize dopamine-mediated neurotransmission (D2) a. Butyrophenones – Haloperidol (1-2 mg bolus q 2-4 hrs; 0.2-0.5 mg in elderly patients) & Droperidol i. Black Box Warning for Halperidol – 4. 5. b. Atypical Neuroleptics – no controlled studies Benzodiazepenes a. No studies demonstrate effectiveness as sole agent apart from delirium 2/2 EtOH/benzodiazepine withdrawal b. Used to augment treatment with antipsychotic Anticholinergic – Physostigmine 2 mg IV (no faster than 1 mg/min) a. Monitor for vagotonic state Dexmedetomidine Environmental Factors a. Orientation – maintenance of glasses/hearing aids b. Avoidance of overstimulation/understimulation