Effect of Staff Education Intervention on Delirium and Dementia
advertisement

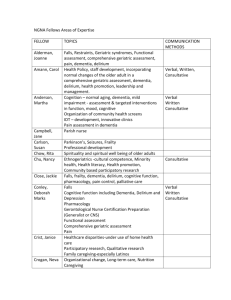
Cincinnati Project, Lead by former Cincinnati Chapter Executive Director, Clarissa Rentz MSN., R.N. The Study: Effect of a Staff Education Intervention on Delirium and Dementia Knowledge and Self Efficacy and Patient Outcomes It is well documented that older hospitalized patients are at greater risk for delirium which is associated with disability and prolonged length of stays. Therefore, the Alzheimer’s Association of Greater Cincinnati, The Christ Hospital (TCH) and TriHealth Inc., undertook a quasi-experimental study to address this challenging nursing care and economic issue. The first component of the study examined the effect of a four hour educational program on nursing knowledge and self -efficacy as it pertained to the differentiation of dementia vs. delirium, associated risk factors and early identification with implementation of care strategies (citations). Nurses (n=167) and PCAs (n=67) from 2 designated non-ICU units from each hospital participated in the educational intervention. Participants completed a 20 item knowledge test and 22 item Dementia/Delirium Self Efficacy (DDSE) survey at three intervals; pre-education, immediately post and 3-months later. Knowledge score increased significantly (P<.05) for both groups from pre to post intervention with slight fading of effect at 3 months. RN mean test score was higher all three times but PCAs showed a greater increase following the intervention than the RNs. Overall self-efficacy followed the same pattern. The second component of the study investigated the effect of the education intervention on patient outcomes. An extensive chart review of patients 65 years and older with a 48 hour minimum length of stay was conducted on the four designated units: 402 pre-intervention; 391 post-intervention. There were no significant demographic differences between groups, including gender, age, and number of comorbidities, prescribed medications, or dementia diagnosis. Results were analyzed for differences between groups and overall trends. Fewer patients post-intervention experienced delirium (122 vs.111). Falls, though infrequent; were reduced from 7 to 3. However, overall length of stay was significantly reduced by almost 8.4 hours in the post-intervention group (n-111) resulting in a 932 hours reduction in hospital stay. In conclusion, a targeted dementia/delirium nursing education intervention can improve nursing knowledge and selfefficacy in the care of patients at risk for delirium as well as produce positive patient outcomes and decrease hospitalization stays and subsequent costs. Recommendations for practice include; implementation of routine patient delirium risk assessment similar to current practices for fall risk or pressure ulcer risk. According to Clarissa in my phone chat with her, the post surveys showed an overwhelming indication that staff now felt more competent to identify dementia and delirium. The most change was in the surveys from PCA’s. (Patient Care Assistants) In fact, now feels that it is MOST important to train those lower level direct care staff members such as PCA’s. Clarissa also feels that the 4 hour training was not necessary, that two hours would be sufficient. She also noted that the small change in the number of falls was probably related to the fact that the hospitals already had undertaken a fall prevention project. She also Now, she says that since this was not considered a big study and they only did it for three months, there are some issues. For instance, they could somehow be seeing some type of seasonal results. The best thing would be to continue the study for a full 12 months.