Delirium - Clinical Departments - Medical University of South Carolina
advertisement

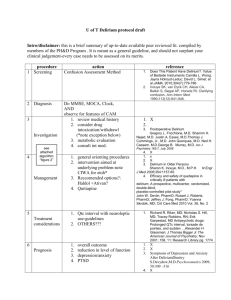
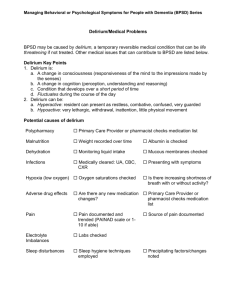
Delirium Ashley Duckett, MD Pamela Pride, MD Medical University of South Carolina 2012 CAM Definition of Delirium Acute onset or fluctuating course AND Inattention (decreased ability to focus, shift or sustain attention) PLUS EITHER Disorganized thinking (incoherent or illogical speech (questions – does a stone float on water, etc) OR Altered Level of Consiousness (anything other than alert and calm) – RASS other than 0 Confusion Assessment Method- Inouye, Ann Intern Med 1990 -INATTTENTION is the cardinal feature for diagnosis -Can use serial 7’s, WORLD, reciting days or months in reverse, etc; ICU uses letter test (SAVEAHAART) -SUBTYPES -Hyperactive – agitated, hyperalert -Hypoactive – calm and confused, lethargic -Mixed – features of both *no difference in etiology or outcomes among the subtypes *hypoactive pts commonly missed without formal screen The 3 D’s Depression - Dementia - Delirium Delirium Dementia Depression Onset Abrupt Slow, insidious Recent, may be associated with loss Duration Hours to days Months to years Stable, may be worse in the morning Attention Impaired Normal, except severe cases Usually normal Consciousness Reduced, fluctuating Clear Clear Silverstein & Maslow, 2006 Why do we care? VERY common (esp if older, had ICU stay) although underdetected Increased morbidity and mortality – Higher risk for falls, decubs, pna – Higher risk of functional decline and institutional care – Longer LOS – Predictor of 12 mo mortality Risk factors (far from an exhaustive list) Age >70 Dementia or underlying brain dysfunction Alcohol abuse Hearing or visual impairment History of delirium Inouye et al, Multicomponent Intervention of Prevent Delirium in Hospitalized Older Patients, NEJM; 1999 (340) 9:669-76) Modifiable risk factors Medications Polypharmacy (>3 new inpt meds) Physical restraints and catheters Sleep deprivation Immobility Uncontrolled pain Medical illness (organ failure, electrolytes, etc) Antiparkinson drugs Insomnia drugs Corticosteroids Narcotics UI drugs Theophylline Emptying drugs (motility drugs) Muscle relaxants Seizures Drugs Cardiovascular Drugs H2 blockers Look to these medications Antimicrobials if there is an NSAIDs ACUTE CHANGE IN MS Geropsychiatric drugs ENT drugs http://www.geronurseonline.org; Flaherty, J.H. (1998). Psychotherapeutic agents in older adults. Commonly prescribed and over-the-counter remedies: causes of confusion. Clinics in Geriatric Medicine, 14(1): 101-27. Mini-Cog Recall 0 Recall 1-2 Impaired Abnormal Clock Impaired Borson S et al. (2000), Int J Geriatr Psychiatry 15(11):1021-1027 Recall 3 Not Impaired Normal Clock Not Impaired Serial administration of a modified RASS for delirium screening Chester, JG et al. J Hosp Med 2012 May-June 7 (5) 450-3. Evaluation Vital signs, pulse ox, volume status Focused exam including determining baseline cognition, urine output, last BM Blood glucose Review medications Consider withdrawal as a cause Testing – CBC, BMP, UA, CXR, EKG Additional testing if clinically indicated Management Try to identify underlying cause Prevent complications and provide supportive care – Avoid bed rest, catheters, mobilize patient – Sleep at night, awake during day – Monitor nutrition status and output – Consider aspiration precautions – Enlist the help of family Management Antipsychotics are drug of choice for treating agitation – Can consider treating hypoactive delirium to treat subjective stress (paranoia, hallucinations) Haldol – cheap, can be given PO, IV, IM – CAN’T be used in Parkinson’s, Lewy body dementia, prolonged QT DON’T USE BENZOs UNLESS YOU’RE TREATING WITHDRAWAL or NMS!!! What’s the evidence? Best drug? Haldol v Atypicals (Risperidone, Olanzipine, Quetipine) – Systematic reviews show similar efficacy, question of fewer side effects – NEED larger and better studies 2005 FDA warning re risk of death – Use for shortest duration, with caution – NEED larger and better studies Haldol and EKGs? Concern for prolonged QTc and torsades or polymorphic VT Review showed that most conduction disturbances involve heart disease and high doses (50mg/24 hrs) More recent review – heart dz, >65, female, hypokalemia Stop if QTc>500 Don’t wait to give Haldol until after EKG Lawrence, Pharmacotherapy 1997; 17(3);531-537 Screening Inpatients Delirium task force Goal should be prevention; cutting back on physical restraints Nurses will screen each shift with RASS Delirium protocol - order set with suggested workup and drug dosing based on patient factors References DSM-IV TR, 2000 Inouye et al, Multicomponent Intervention to Prevent Delirium in Hospitalized Older Patients, NEJM; 1999 (340) 9:669-76) Borson S et al. (2000), The mini-cog: a cognitive 'vital signs' measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry 15(11):10211027 Flaherty, J.H. (1998). Psychotherapeutic agents in older adults. Commonly prescribed and over-the-counter remedies: causes of confusion. Clinics in Geriatric Medicine, 14(1): 101-27. http://www.geronurseonline.org Lawrence, Conduction Disturbances Associated with Administration of Butyrophenone Antipsychotics in the Critically Ill: A Review of the Literature. Pharmacotherapy 1997; 17(3);531-537 Wenzel-Seifert, QTc Prolongation by Psychotropic Drugs and the Risk of Torsade de Pointes. Dtsch Arztebl Int 2011; 108 (41): 687-93 Delirium. Updates in Hospital Medicine 2012. Harvard Medical School Antipsychotics for delirium. Cochrane review