Managing Acute Confusion in The Elderly
advertisement
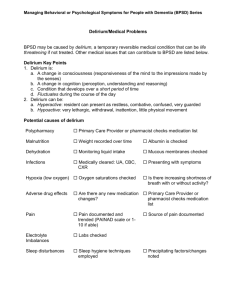
Managing Acute Confusion in The Elderly Dr Rachel Nockels OPALS Consultant Why is this relevant? GP curriculum statement 9 (care of older people) requires GPs to be able to manage the problems of older people, such as confusion, in the elderly Causes of Acute confusion 1. 2. 3. 4. 5. 6. 7. 8. Delirium Worsening dementia Depression Alcohol withdrawal or substance misuse Psychotic disorder Thyroid disease Mania (Schizophrenia) Delirium - definition A common clinical syndrome characterised by disturbed consciousness, cognitive function or perception which has an acute onset and fluctuating course NICE delerium guideline Definition DSM IV disturbance of consciousness (i.e., reduced clarity of awareness of the environment) with reduced ability to focus, sustain, or shift attention. a change in cognition (such as memory deficit, disorientation, language disturbance) or the development of a perceptual disturbance that is not better accounted for by a pre-existing, established, or evolving dementia. the disturbance develops over a short period of time (usually hours to days) and tends to fluctuate during the course of the day. there is evidence from the history, physical examination, and laboratory findings that: (1) the disturbance is caused by the direct physiological consequences of a general medical condition, (2) the symptoms in criteria (a) and (b) developed during substance intoxication, or during or shortly after, a withdrawal syndrome, or (3) the delirium has more than one aetiology”. Confusion Assessment Method 1. 2. 3. 4. Acute onset and fluctuating course Inattention Disorganised thinking Altered level of consciousness A positive CAM requires presence of 1 AND 2 plus either 3 or 4 DELIRIUM DEMENTIA DEPRESSION Sudden (hours to days) Usually gradual (over months) Gradual (over weeks to months) Alertness Fluctuates Sleepy or agitated Generally normal Generally normal Attention Fluctuates – difficulty concentrating, easily distractible Generally normal May have difficulty concentrating, easily distractible Sleep Change in sleeping pattern (often more confused at night) Can be disturbed – night time wandering and confusion possible Early morning wakening Thinking Disorganised - jumping from one idea to another Problems with thinking and memory, may have problems finding right word Slower, preoccupied with negative thoughts of hopelessness, helplessness or self depreciation Illusions, delusions and hallucinations common. Generally normal Generally normal Onset Perception European Delirium Association Theories of delirium pathophysiology 1. 2. Cholinergic deficiency Aberrant stress response/ neuroinflammation Delirium – sub types Hyperactive Hypoactive Mixed (Subsyndromal) Prevalence Medical wards – 20-30% Post surgery – 10-50% Long term care – just under 20% Community- ? Up to 1% Who Is At Risk? Those aged 65 years and older Hip fracture Cognitive impairment Severe illness Sensory impairment Previous episode of delirium Precipitating factors Drugs Infection Neurological Cardiological Respiratory Electrolyte imbalance Endocrine and metabolic Constipation Change in environment Think Pinch Me Pain INfection Constipation Hydration Medication Environment Consequences Dementia/Cognitive impairment Progression of dementia Discharge to care home (for people who were in hospital) Falls Hospital admission (for people who were in long-term care) Post discharge care Consequences cont. Post traumatic stress disorder Pressure Ulcers Mortality Impact on carers Length of stay Quality of life for patients Management Best management is prevention Reorientate Nurse in familiar surroundings Stop all unnecessary medications Keep lighting appropriate Put in hearing aids and wear glasses Keep well hydrated Monitor nutrition Re-align sleep wake cycle Treatment Identify cause(s) Ensure effective communication Use verbal and non verbal techniques Keep moves to a minimum If a risk to themselves or others consider short term haloperidol or olanzapine Continue to re evaluate De Escalation Techniques Approach in a calm manner Give choices and maintain patient dignity Speak in a low even tone Do not maintain eye contact Do not interrupt or argue Allow space, do not touch patient Empathise with their feelings Don’t put yourself at risk Sedation Should be avoided If necessary use low dose and gradually increase Who Needs Admitting? Live alone Will be left unsupervised for any duration of time If carers (or RH) are unprepared or unable to continue looking after the patient If the cause does not become clear despite investigation or the patient fails to improve with treatment and/or If the history and/or examination indicate a cause requiring acute hospital treatment Conclusion Acute confusion in the elderly is a common problem Delirium is often missed especially hypoactive form It can take months to resolve The consequences can be devastating Try not to use sedation if at all possible Thank you Any questions?