Physical Principles of Mammography
advertisement

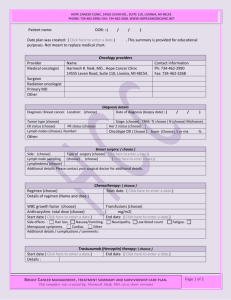
PHYSICAL PRINCIPLES OF MAMMOGRAPHY European School of Medical Physics, Archamps, November 2005 Dr David Dance Joint Department of Physics, Institute of Cancer Research and Royal Marsden Hospital, London SW3 6JJ, United Kingdom 1 Properties of the female breast Compressed breast thickness Compressed breast area 2 -11 cm 35 cm2 - large enough to require several exposures Composition - mixture of adipose and glandular tissues. glandular tissue is most sensitive to carcinogenesis Atomic compositions. Data from Hammerstein et al. Radiology 130 (1979) 485-491 PERCENTAGE COMPOSITION BY WEIGHT DENSITY H C N O Gm/cc Fat 11.2 49.1-69.1 - 18.9-35.7 0.93 Gland 10.2 10.8-30.5 3.2 55.2-75.9 1.04 calcium hydroxyapatite or phosphate, size 0 - several mm2 important to see 200 micron calcifications Calcifications - Breast glandularity varies with breast size and age, though there is a large variability. Figure shows glandularity of typical breasts for women aged 50-64 from two regions in UK (Dance et al. PMB 45 (2000) 3225-40. Glandularity (%) 100 80 60 40 20 0 0 2 4 6 8 10 Breast thickness (cm) 2 Photon interactions Variation of attenuation with type of tissue : Fibro-glandular tissue has a much higher attenuation coefficient than fatty tissue. The difference in attenuation between fibro-glandular tissue and carcinoma can be small. Carcinomas more likely to be seen as a change in breast architecture. Data from Johns and Yaffe, PMB 32 (1987) 675-695 1 The photoelectric cross section dominates below 22 keV. Only a small energy transfer for scatter processes. Large attenuation coefficient at low energies means low transmission through the breast. Scattering Processes At low energies it is not sufficient to assume that all scattering processes are from free electrons. Allowance must be made for electron binding. For most purposes it is sufficient to assume atomic binding. Two scattering processes must be considered: coherent and incoherent scattering. In coherent scattering all the electrons scatter in phase and there is no energy transfer, but only a change in photon direction. This is dominant in the forward direction and decreases with increasing momentum transfer. Away from the forward direction, incoherent scattering becomes important. This is scattering with energy transfer to a recoil electron and approaches the standard Klein-Nishina cross section for large momentum transfers. Comparison of scattering processes for breast tissue at 20keV. The Klein-Nishina formula is a poor approximation in the forward direction but is a good approximation in the backward direction where the contribution of coherent scattering is smaller. . 3 Important physical parameters Requirements for mammography high contrast good resolution (unsharpness) low dose low noise large dynamic range 2 Contrast Factors, which affect contrast: object background transmitted spectrum receptor scatter Variation of contrast with photon energy. Contrast calculated ignoring degradation due to unsharpness and scatter. Contrast decreases rapidly with increasing photon energy. Low energy is necessary to achieve adequate contrast, but this is in conflict with the requirements of low dose. Unsharpness Unsharpness contributions : geometric unsharpness receptor unsharpness movement unsharpness Dose Factors, which affect dose : breast thickness breast composition photon spectrum receptor sensitivity Various dose specifications have been suggested : incident or surface dose, mid-breast dose, mean breast dose and the mean dose to the glandular tissues within the breast, which are the tissues at risk of radiation induced carcinogenesis. The latter quantity is the quantity of choice and has been recommended by the ICRP and generally adopted in national dosimetry protocols. There is a dose penalty for using low energy photons to image the breast. Low energy photons are strongly absorbed and contribute only to dose and not to the image. 3 Transmission of photons through breast tissue. Dose varies rapidly with depth. Surface dose is not a good indicator of risk. Dose depends upon tissue type. There is a large advantage in reducing the breast thickness by compression. Dependence of mean glandular dose on breast composition and thickness. Noise Factors, which affect noise : quantum mottle light photons screen structure film granularity Signal-to-Noise Ratio for a 100 micron calcification. Calculated for a Min-R/OM screen/film combination, ignoring unsharpness and only including contribution of quantum mottle. There is a threshold energy above which the calcification will not be seen. 4 X-ray Tube 4 X-ray spectra The choice of photon energy for mammography is a compromise between contrast and dose. To find the optimum energy, it is necessary to introduce further constraints in terms of the contrast needed or the signal-to-noise ratio (SNR). One approach is to calculate the SNR for fixed dose to the breast. Dependence of SNR for fixed breast dose on photon energy and breast thickness. SNR calculated for imaging a 100 micron calcification and ignores unsharpness. Noise due to quantum mottle only. Each curve is for fixed breast thickness and the position of the maximum gives an optimum energy in terms of SNR. This is probably most relevant to digital imaging. Optimal energies bands for mammography based on SNR for fixed dose : 2cm breast 14-18 keV 6cm breast 19-23 keV 4cm breast 17-21 keV 8cm breast 20.5-23.5 keV 1.25 Relative number of photons A 1.00 Mammographic X-ray spectrum from a Mo target at 28kV filtered by 30 micron Mo. The Mo characteristic X-ray lines are well suited to imaging all but the largest breasts where a higher energy spectrum might have some advantages. 0.75 0.50 The X-ray spectrum is chopped at 20keV because of the Mo filter. 0.25 0.00 10 15 20 25 30 Photon energy (keV) Transmission through a 30 micron Mo filter The Mo K-edge is at 20keV and there is a step in the photoelectric cross section at this energy. The result is decreased transmission above the K-edge. 5 Possible K-edge filter materials for mammography: molybdenum rhodium palladium 20 keV 23.3 keV 24.3 keV X-ray tubes are available with a dual anode and a selection of filters. The anode, filter and tube potential are selected automatically after a brief pre-exposure to establish the transmission through the breast. 1.25 The figure shows the spectrum obtained using a rhodium target and a rhodium filter at 28 kV. Relative number of photons E 1.00 This higher energy spectrum is better suited to imaging larger breasts. 0.75 0.50 0.25 0.00 10 15 20 25 30 Photon energy (keV) Figure shows relationship between contrast (of a calcification) and mean glandular dose for different target/filter combinations. Each curve shows the variation as the tube voltage is changed from 25- 32 kV. None of the new spectra can match the Mo/Mo contrast at 26 kV and only one spectrum can match Mo/Mo at 28 kV (Mo/Rh) and some dose saving is then possible. If the contrast requirement is relaxed (say to match Mo/Mo at 30 kV), a larger dose saving is possible and other target/filter combinations can be used.) 8.0 Mean glandular dose (mGy) 25 kV Mo/Mo Mo/R h 6.0 26 kV R h/Al 28 kV R h/R h W /R h 30 kV 4.0 32 kV 2.0 0.0 0.20 0.25 0.30 0.35 Contrast Figure shows the relationship between the mean glandular dose and the choice of X-ray spectrum in digital mammography for the task of imaging a particular detail at a signal-to-noise ratio of 5. Results are for an 8cm thick breast of 10% glandularity. The W/Rh spectrum is the best of those illustrated. It is important to note that the choice of optimum spectrum is dependent on breast thickness. The following reference discusses the choice of spectra for screen-film and digital mammography: Influence of anode filter material and tube potential on contrast, signal-to-noise ratio and average absorbed dose in mammography: a Monte Carlo study, Dance et al BJR 73 (2000) 1056-67) 6 Focal spot size and imaging geometry If we ignore movement unsharpness, then an estimate U of the overall unsharpness can be obtained by combining the geometric and receptor unsharpness in quadrature. U 1 m 1 2 f 2 F 2 m Here m is the magnification, f the focal spot size and F the receptor unsharpness. The first squared term is the geometric unsharpness and is zero for magnification 1. The unsharpness has been normalised to correspond to sizes in the object plane Variation of unsharpness with (actual) focal spot size and image magnification. Receptor unsharpness of 100 micron assumed. Curves shown for focal spot sizes of 0, 100, 600, 1000 micron. An actual focal spot size of 0.6mm or less and an FFD of at least 60cm are recommended. For moderate focal spot sizes, the overall unsharpness increases with magnification and contact mammography only should be used. Increasing the FFD or decreasing the OFD will decrease magnification and improve the unsharpness. For a small focal spot size, magnification decreases unsharpness but will increase dose. Because of the air gap, there will be a decrease in scatter (no grid is normally used for magnification), and a larger image on the same receptor means the effect of noise is reduced. 5 Breast Compression Reasons for compression : reduced dose reduced scatter - improved contrast softer spectrum - improved contrast reduced geometric unsharpness reduced movement unsharpness reduced dynamic range of image reduced tissue overlap - better visualisation 6 Anti-scatter grids The contrast in the image is degraded by the scattered radiation recorded by the image receptor. The amount of degradation varies with photon energy, breast size and image receptor. It can be quantified using the contrast degradation factor CDF which is the ratio of the image contrast with and without the effects of scatter. CDF 1 1 S P where S and P are the energies absorbed in the receptor from secondary and primary radiation respectively. Grid parameters for a typical mammographic grid: 7 lines/cm interspace lead height grid ratio 31 paper 1.5 mm 5.0 Variation of S/P ratio with breast thickness. Min-R screen, 28kV Mo/Mo. Without a grid, the CDF for a 5cm breast is 0.65. S grid and M grid indicate values corresponding to the use of particular stationary and moving grids Grid performance can be assessed in terms of the contrast improvement factor CIF and the Bucky factor BF. The CIF is the ratio of the contrasts with and without the grid and is given by : CIF 1 1 Ts S Tp P The BF is the ratio of the exposures with and without the grid and is given by : BF CIF Tp Ts and Tp are the transmissions of secondary and primary photons through the grid respectively. For medium to large breasts, the contrast improvement associated with the use of the grid is important. For a 2cm breast the CIF is only 1.2 whereas the BF for the M-grid is 1.7 8 7 Screen/film receptor Speed Factors which affect speed : K-edge keV CaWO4 Gd2O2S La2O2S Y2O2S 69.5 50.2 38.9 17.0 screen thickness photon spectrum Light efficiency % 3.5 15 12 18 light output screen composition film response film processing (Light efficiency data taken from Stevels, 1975) Energy absorption efficiencies for various phosphors. Each curve is for a screen 100 micron thick (i.e. all screens have similar resolution) with a 50% phosphor packing density. The Gd2O2S and CaWO4 phosphors have the best energy absorption efficiency. Taking into account the light efficiency of the phosphor means that Gd2O2S is the phosphor of choice. Energy absorption efficiency for Kodak Min-R screen (33.9 mg/cm2 Gd2O2S) Calculations of efficiency vs energy for both primary and secondary photons for a 6cm thick breast. The higher efficiency for the secondary photons is due to the greater path length and lower energy. This effect enhances the S/P ratio. For Gd2O2S, a 20 keV X-ray will produce about 1200 light photons of typical energy 2.4 eV. 9 Resolution Factors which affect resolution: screen thickness absorptive dyes incident photon spectrum crossover (double screen system only) Spread of light fluorescent photons as they pass from screen to emulsion. The screen is placed behind the emulsion to bring the X-ray photon interaction point as close as possible to the emulsion MTF measured by Kuhn and Knüpfer (Medical Physics 19 (1992) 449) for mammographic screens constructed to a standard prescription and to achieve high detail or low dose. Mammographic screen films Important factors are contrast latitude sensitivity processing granularity reciprocity failure Film characteristics and film gamma for two mammographic screen films. The region of high gamma or good contrast is very limited and correct exposure is very important [Data from Meeson et al. BJR 74 (2001) 825-835]. 10 Wiener spectra, DQE and NEQ Noise power (Wiener) spectra for a mammographic screen-film combination. Data taken from Nishikawa and Yaffe (Medical Physics 12 (1985) 32). MinR screen with Ortho M film. O.D. 1.0 At normal optical densities and moderate frequencies, the quantum mottle is the largest noise contribution. At low and high OD and at high frequencies, the film granularity dominates. The detective quantum efficiency (DQE) and the noise equivalent quanta (NEQ) are useful measures of the imaging performance which take account of the noise. Bunch [e.g. SPIE 1090 (1989) 67 and SPIE 3659 (1999) 120] has measured DQE and NEQ for various mammographic screen-film combinations. For the MinR screen used in conjunction with OrthoM film, the highest value of the DQE is 0.27, much lower than the efficiency shown earlier. This is because of the additional noise introduced in converting absorbed X-ray energy into an image. Detective quantum efficiency 0.5 The figure shows the DQE for the MinR2000 screen-film combination. For this combination, the highest DQE value is about 0.4. The highest values of the DQE and NEQ occur at optical densities higher than 1.0, and there is a significant loss of performance at high and low optical densities and at high frequencies. 2 0.4 4 6 0.3 0.2 10 0.1 15 20 0.0 4.9 5.1 5.3 5.5 5.7 5.9 Log10 (X-ray quantum f luence) The desirability of using an optical density greater than 1.0 is consistent with work by Young et al. (table below and Clin. Radiol. 49 (1994) 461). These authors found that that the cancer detection rate in the UK National Breast Screening Programme was dependent upon the optical density on the film, with the higher detection rates found at higher optical densities. Table: Small cancer detection rates in the UK Breast Screening Programme. Optical density range Small cancer detection rate (%) 0.8 - 0.99 1.0 - 1.19 1.2 - 1.39 1.4 - 1.59 1.6 - 1.79 1.8 - 1.99 0.13 0.02 0.11 0.01 0.16 0.01 0.17 0.01 0.18 0.02 0.20 0.02 11 9 General references Säbel M and Aichinger H 1996 Recent developments in breast imaging Phys. Med. Biol. 41 315 Dance D R 2005 Physical principles of mammography in: Commissioning and routine testing of mammographic X-ray systems, A C Moore et al. IPEM Report 89, IPEM, York. 12