ch17_notes
advertisement

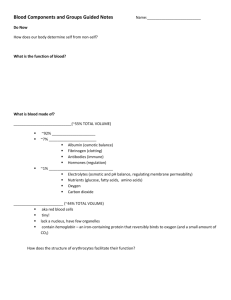
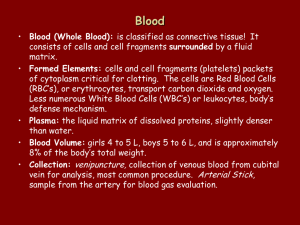
Ch. 17 Notes: Blood Overview Blood Plasma Formed Elements Hemostasis Blood Transfusion Blood Tests ___________ Overview Total blood volume ~= 80 ml/kg, i..e. 5-6 L in a 70 kg person; 4-5 L typ in female, 5-6 typical in male pH, hematocrit: What are normal values? Formed elements versus plasma Blood Plasma Water Cations (Na+) & anions (Cl-, HCO3-, Proteins-) Proteins: albumin, clotting factors, antibodies Formed Elements Hemostasis Blood Transfusion Blood Tests ______________ Overview Connective tissue: cells (formed elements) and plasma (the extracellular matrix) Spin a tube of blood in a centrifuge: get red cells, buffy coat, & plasma Percent that is red cells (erythrocytes) is the hematocrit (Hct). Normal Hct = approx. 38-45% female, 4050% male, add 5-10% if living at high altitude. Total blood volume ~= 4-5 L in female, 5-6 L in male; about 80-100 ml per kg of body weight pH=7.35-7.45 Functions Deliver O2 & nutrients from where they enter the body to where they are used (tissues everywhere). Carry CO2 & wastes from where they are produced (everywhere) to where they are eliminated. Distribute hormones. Regulate body temp, pH, osmolality, fluid balance. Immune protection. Blood Plasma 90% water. Solutes include: nutrients, gases, hormones, wastes, ions, proteins. Dominant protein is albumin. Also clotting cascade proteins & antibodies. Ions: cations (+) & anions (-). Dominant cation in plasma is Na+. Anions include Cl-, proteins, bicarbonate (HCO3-) Formed Elements Erythrocytes = red blood cells = RBCs. Bags of hemoglobin (Hb), no nuclei, no organelles. Bi-concave disk shape give large surface area-to-volume ratio, good for gas exchange. Job = oxygen transport. Use Hb to do it. Normal Hb = 13-18 g/ 100 ml Hemoglobin protein: 4 amino acid chains. Each has 1 heme molecule in it. Each heme has 1 iron atom which can carry one O2 molecule. Oxygenated Hb bright red, deoxygenated dark red. Hematopoiesis (making new blood cells, occurs in red marrow); Erythropoesis = making new RBCs. All blood cells come from hematopoetic stem cell = hemocytoblast. EPO (erythropoetin) (kidney hormone) stimulate RBC formation in red marrow. Kidney makes more EPO if O2-carrying ability of blood is insufficient or if move to high altitude Reticulocyte = last cell before RBC in the development pathway Erythropoesis requires B12, folate, iron RBC life span 100-120 days Old RCs removed by spleen. Protein recycled, heme goes to liver, iron recycled; organic part of heme exits body in bile Anemia = deficiency in RBCs; many causes Hemorrhagic anemia: excessive blood loss. Iron-deficiency anemia, pernicious anemia (lack of B12); renal anemia (kidney disease causes not enuf EPO); hemolytic anemia (RBCs are prematurely destroyed) Sickle-cell anemia: mutant Hb doesn’t fold right, forms rods inside cells, cuausing sickle shape Polycythemia: too many RBCs, causes too-high viscosity of blood (blood is sludgy) Leukocytes (White Blood Cells) <1% total blood volueme. Mediate immune defenses in various ways. One way to classify leukocytes into 2 groups: Granulocytes & agranulocytes Granulocytes Neutrophils – 50%-70% of all leukocytes, migrate to site of inflammation, phagocytic Polys = PMNs Basophils – release histamine as part of inflammatory repsonse Eosinophils – release enzymes to fight parasites esp. parasitic worms Agranulocytes Monocytes – turn into macrophages when they leave blood capillaries to enter peripheral tissue whetre they phagocytose debris, bacteria, damaged & infected cells Lymphocytes: B- and T-lymphocytes are immune cells that make antibodies and recognize & destroy foreign pathogens Platelets Fragments of megakaryocytes. Essential for hemostasis – stopping bleeding. Thrombopoietin regulates platelet formation. Hemostasis – Stopping Bleeding from damaged vessels Vascular spasm helps reduce local blood flow Platelet Plug Formation (pp. 646–647; Fig. 17.13) Platelets stick where endothelium is disrupted/damaged. Release cytokines that attract more platelets – positive feedback. Coagulation: formation of a “blood clot” Three phases Phase 1 can occur via either or both of two parallel pathways: Direct & indirect pathways. Usually both. Both lead to formation of prothrombin activator. Direct involves activated platelets and several proteins (enzymes) of the clotting cascade. Indirect skips some of those steps & tissue factor released from damaged tissue is a key activating factor. Phase2: Prothrombin activator catalyzes conversion of prothrombin to thrombin Phase 3: thrombin catalyzes polymerization of fibrinogen monomers into fibrin strands. Fibrin strands form a mesh that traps RBCs and now you have a blood clot. Clot Retraction and Fibrinolysis: breakdown & removal of blood clot. Plasmin breaks down fibrin. Disorders of Hemostasis Thromboembolic disorders: too much clotting. Know what embolus, thrombus are. Thrombocytopenia: too few platelets. Causes: damaged/suppressed bone marrow; and may result from any condition that suppresses or destroys red bone marrow. Hemophilia: tendency to not clot due to lack of a protein in the clotting cascade, due to an inherited mutation Disseminated intravascular coagulation (DIC): widespread clotting in intact vessels, a potentially fatal complication of septic shock. “Blood thinners” include “antiplatelet”, “anticoagulant”, and “thrombolytic” drugs. Antiplatelet drugs block formation of platelet plug: aspirin, Plavix, etc. Anticoagulants block coagulation pathway, i.e prevent conversion of fibrinogen to fibrin by thrombin: heparin, warfarin (Coumadin), hirudin, etc. Thrombolytics “lyse thrombi”, i.e. they break down existing clots. Thrombolytics used in patients suffering from recent stroke or MI, must be used as soon as possible: streptokinase, tissue plasminogen activator (tPA), etc. Transfusion and Blood Replacement Understand the human blood types and their role in determining who can give blood to whom. First we describe the human blood types. Then we will explain how to predict who can give to/receive from whom. There are three proteins which may be present on the surface of red blood cells (RBCs): the A, B, and Rh proteins. These proteins are often called “antigens” (antibody generators) because they can cause the immune system to make antibodies. A person either has A proteins on their RBCs, or they don’t. Likewise for B and Rh: you either have B antigens or you don’t, and you either have Rh antigens or you don’t. If you have neither A nor B antigens, your blood type is “O”. (Think zero or null.) A person with Rh antigens on their RBCs is called “positive” (positive for Rh), and a person without Rh antigens on their RBCs is “negative”. So a person who is “AB+” (spoken “AB positive”) has A antigens and B antigens and Rh antigens on their RBCs. An “O-” person (spoken “O negative”) has neither A nor B nor Rh. A person who is “B+” has the B antigen and the Rh antigen, but not A, on their RBCs. And so on. If you make a list, you see there are 8 total possible blood types. When it comes to blood transfusions, remember three principles: 1. The immune system of the recipient will attack and destroy RBCs with “foreign” antigens. 2. The immune system will not notice and will not be bothered by the absence of an antigen. 3. The immune system will not attack “self” antigens. Now you know everything you need to know to predict who can donate to and receive from whom. Type O negative (O-) blood is the best to have in the blood bank, because it can be given to anybody. It can be given to anybody because it has neither A nor B nor Rh antigens, so it has nothing that could provoke an immune system attack. Therefore an O- person is a “universal donor”. A person who is AB positive (AB+) can receive any type of blood, because their own blood has A and B and Rh antigens. This means their own immune system is “used to” all three antigens, and therefore it will not attack blood with any of the antigens. Therefore an AB+ person is a “universal recipient”. Test question 1: Can you give B- blood to an A+ person? Why? Answer: No you cannot, because Bblood has the B antigen, which is “foreign” to the immune system of an A+ person. Therefore the A+ person’s immune system would attack and destroy “B-” RBCs. Test question 2: Can you give O+ blood to a B+ person? Why? Answer: Yes you can, because the only antigen on O+ blood is the Rh antigen, which is “familiar” to the immune system of a B+ person. The absence of B antigens on the donated O+ blood is not a problem, because the immune system does not notice the “lack” of something. Diagnostic Blood Tests Clinicians diagnose many diseases & conditions with blood tests “CBC with diff” = complete blood count with differential, i.e. with differential identification of how many of which types of leukocytes are present Blood gas analysis: Measure O2, CO2, pH levels in blood. This might be done with a patient in the ER, or in the intensive care unit, or during surgery. Blood from a systemic artery is typically used. Blood chemistry analysis: analyze levels of many chemicals in blood, including electrolytes, various enzymes, etc. Blood lipid profile: measure amount of cholesterol & other lipids (fats) in blood Copyright © 2015, William C. Rose