phys chapter 35 [12-11
advertisement
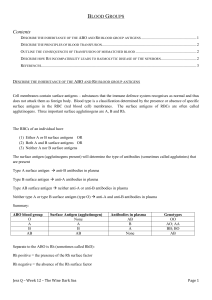
Phys Ch 35 Antigenicity Causes Immune Reactions in Blood Bloods of different people have different antigenic and immune properties so antibodies in plasma of one blood react with antigens on surfaces of RBCs of another blood type At least 30 commonly occurring antigens and hundreds of rare antigens, each of which can at times cause antigen-antibody reactions, have been found on surfaces of PMs of human blood cells o Most antigens weak and only of importance for studying inheritance of genes to establish parentage O-A-B Blood Types A and B antigens called agglutinogens because they often cause blood cell agglutination Come from type O, type A, and type B genes (only one of which can be present on each chromosome) 47% O, 41% A, 9% B, 3% AB Agglutinogens are what is presented on the cells, and agglutinins are what the cell is against (anti-B, anti-A, etc.) o So person with genotype OB has B agglutinogens, is blood type B, and has anti-A agglutinins Immediately after birth, quantitiy of agglutinins in plasma is almost zero, but 2-8 months after birth, infants begin to produce agglutinins for whatever is not presented on their RBCs o Maximum titer usually reached at 8-10 years of age and gradually declines throughout remainder of life o Agglutinins are gamma globulins produced by bone marrow and lymph gland cells that produce antibodies to any other antigens; most are IgM and IgG antibodies o Small amounts of type A and B antigens enter body in food, bacteria, and other ways, and these substances initiate development of anti-A and anti-B agglutinins When agglutinogens exposed to agglutinins that attack them, RBCs agglutinate as result of agglutinins’ attaching themselves to RBCs; because agglutinins have 2 bindings sites (IgG) or 10 binding sites (IgM), single agglutinin can attach to 2 or more RBCs at same time, causing cells to be bound together by agglutinin o Clumps plug small blood vessels throughout circulatory system o During ensuing hours to days, either physical distortion of cells or attack by phagocytic WBCs destroys membranes of agglutinated cells, releasing hemoglobin into plasma (hemolysis of RBCs) When recipient and donor bloods mismatched, immediate hemolysis of RBCs occurs in circulating blood o Antibodies cause lysis of RBCs by activating complement system, which releases proteolytic enzymes (lytic complex) that rupture PMs o Immediate intravascular hemolysis far less common than agglutination followed by delayed hemolysis because there has to be a high titer of antibodies for lysis to occur and different types of antibodies required, mainly IgM antibodies (hemolysins) Blood typing (blood matching) – RBCs separated from plasma and diluted with saline; one portion mixed with anti-A agglutinin and another portion mixed with anti-B agglutinin, then observe which ones agglutinated Rh Blood Types In O-A-B system, plasma agglutinins responsible for causing transfusion reactions develop spontaneously, but with Rh system, spontaneous agglutinins almost never occur o Person must first be massively exposed to Rh antigen, such as by transfusion of blood containing Rh antigen, before enough agglutinins to cause significant reaction develop 6 common types of Rh antigens, each called Rh factor – types designated C, D, E, c, d, and e o Person who has C antigen does not have c antigen, but person missing C antigen always as c antigen (true for all three letters) o Because of manner of inheritance of these factors, each person has one of each of the 3 pairs o Type D antigen widely prevalent in population and considerably more antigenic than other Rh antigens (these people are Rh positive, and those without D antigen are Rh negative) o Even in Rh-negative people, some of other Rh antigens can still cause transfusion reactions, although they are much milder o About 85% of whites, 95% of African Americans, and virtually 100% of African blacks Rh positive When RBCs containing Rh factor injected into person whose blood does not contain Rh factor, anti-Rh agglutinins develop slowly, reaching maximum concentration of agglutinins about 2-4 months later o With multiple exposures to Rh factor, Rh-negative person eventually becomes strongly sensitized o If Rh-negative person has never been exposed to Rh-positive blood, transfusion of Rh-positive blood will likely cause no immediate reaction, but anti-Rh antibodies develop in sufficient quantities during next 2- 4 weeks to cause agglutination of transfused cells still circulating in blood (cells hemolyzed by tissue macrophage system) – delayed transfusion reaction (usually mild); on subsequent transfusion of Rhpositive blood, transfusion reaction greatly enhanced and can be immediate and as severe as transfusion reaction caused by mismatched A or B blood Erythroblastosis fetalis – disease of fetus and newborn child characterized by agglutination and phagocytosis of fetus’s RBCs; in most instances mother is Rh negative and father is Rh positive, and baby inherited Rh-positive o Mother develops anti-Rh agglutinins from exposure to fetus’s Rh antigen, and mother’s agglutinins diffuse through placenta into fetus and cause RBC agglutination o 3% of second Rh-positive babies exhibit some signs of erythroblastosis fetalis, about 10% of third babies exhibit disease, and incidence rises progressively with subsequent pregnancies o After anti-Rh antibodies form in mother, they diffuse slowly through placental membrane into fetus’s blood and cause agglutination and hemolyze RBCs, releasing Hgb into blood; fetus’s macrophages convert Hgb into bilirubin, which causes baby’s skin to become jaundiced; antibodies can also attack and damage other cells of body o Jaundiced, erythroblastotic newborn baby usually anemic at birth, and anti-Rh agglutinins from mother usually circulate in infant’s blood for another 1-2 months after birth, destroying more RBCs o Hematopoietic tissues of infant attempt to replace hemolyzed RBCs, and liver and spleen become greatly enlarged and produce RBCs as they would during middle of gestation o Because of rapid production of RBCs, many early forms of RBCs, including many nucleated blastic forms, passed from baby’s bone marrow into circulatory system, and because of presence of nucleated blastic RBCs, it is called erythroblastosis fetalis o Many children who survive anemia exhibit permanent mental impairment or damage to motor areas of brain because of precipitation of bilirubin in neuronal cells, causing destruction of many (kernicterus) o One treatment is to replace neonate’s blood with Rh-negative blood – repeated several times throughout first few weeks of life, mainly to keep bilirubin level low and prevent kernicterus By time transfused Rh-negative cells replaced by Rh-positive cells baby produces (requires 6 or more weeks), anti-Rh agglutinins from mother will have been destroyed o Rh immunoglobulin globin (anti-D antibody) administered to expectant mother starting at 28-30 weeks gestation; anti-D antibody also administered to Rh-negative women who deliver Rh-positive babies to prevent sensitization of mothers to D antigen; greatly reduces risk of developing large amounts of D antibodies during subsequent pregnancies Anti-D antibody inhibits antigen-induced B lymphocyte antibody production in expectant mother Administered anti-D antibody attaches to D-antigen sites on Rh-positive fetal RBCs that may cross placenta and enter circulation of expectant mother, thereby interfering with immune response to D antigen Transfusion reactions – mostly donor blood becomes agglutinated; rare that recipients are because plasma portion of donor blood immediately becomes diluted by all plasma of recipient, thereby decreasing titer of infused agglutinins to level usually too low to cause agglutination; small amount of infused blood does not significantly dilute agglutinins in recipient’s plasma, so recipient’s agglutinins can still agglutinate mismatched donor cells o Hgb released from RBCs converted by phagocytes to bilirubin and later excreted in bile of liver o Concentration of bilirubin in body fluids often rises high enough to cause jaundice, but if liver function normal, bile pigment will be excreted into intestines by liver bile, so jaundice usually does not appear in adult unless more than 400 mL of blood is hemolyzed in less than a day One of most lethal effects of transfusion reactions is kidney failure, which can begin in a few minutes to a few hours and continue until person dies of renal failure o Antigen-antibody reaction of transfusion reaction releases toxic substances from hemolyzing blood that cause powerful renal vasoconstriction o Loss of circulating RBCs in recipient, along with production of toxic substances from hemolyzed cells and from immune reaction, often causes circulatory shock; arterial BP falls very low, and renal blood flow and urine output decrease o If total amount of free Hgb released into circulating blood greater than quantity that can bind with haptoglobin (plasma protein that binds small amounts of Hgb), much of excess leaks through glomerular membranes into kidney tubules; if amount is still slight, it can be reabsorbed through tubular epithelium into blood and cause no harm, but if great, then only small percentage reabsorbed Water continues to be reabsorbed, causing tubular Hgb concentration to rise so high that Hgb precipitates and blocks many kidney tubules Transplantation of Tissues and Organs Most of different antigens of RBCs that cause transfusion reactions also widely present in other cells of body, and each bodily tissue has its own additional complement of antigens o Foreign cells transplanted anywhere into body of recipient can produce immune reactions Autograft – transplant of tissue from one part of same individual to another part Isograft – transplant of tissue from one identical twin to another Allograft – transplant from one individual to another of the same species Xenograft – transplant from one animal to another animal of a different species With autografts and isografts, cells in transplant contain virtually same types of antigens as tissues of recipient and will almost always continue to live normally and indefinitely if adequate blood supply provided With xenografts, immune reactions almost always occur, causing death of cells in graft within 1 day to 5 weeks unless specific therapy used to prevent immune reactions Tissues and organs that have been transplanted as allografts from one person to another – with proper matching of tissues between persons, many kidney allografts have been successful for 5-15 years, and allograft liver and heart transplants 1-15 years Human Leukocyte Antigen (HLA) complex of antigens – most important antigens for causing graft rejection; six of these antigens present on tissue cell membranes of each person, but 150 HLA antigens to choose from (more than a trillion possible combinations) o Development of significant immunity against any one of these antigens can cause graft rejection o HLA antigens occur on WBCs as well as tissue cells, so tissue typing for these antigens done on membranes of lymphocytes that have been separated from person’s blood (lymphocytes mixed with appropriate antisera and complement, then after incubation cells tested for membrane damage, usually by testing rate of trans-membrane uptake of special dye) o Some of HLA antigens not severely antigenic, so precise match of some antigens between donor and recipient not always essential to allow autograft acceptance o Best success has been with tissue-type matches between siblings and between parent and child o Match in identical twins is exact, so transplants between identical twins almost never rejected In person with serious depression of immune system, grafts can be successful without use of significant therapy to prevent rejection In normal person, even with best possible tissue typing, allografts seldom resist rejection for more than a few days or weeks without use of specific therapy to suppress immune system o Because T cells mainly portion of immune system important for killing grafted cells, their suppression is much more important than suppression of plasma antibodies o Glucocorticoid hormones isolated from adrenal cortex glands (or drugs with glucocorticoid-like activity) suppress growth of all lymphoid tissue, and therefore, decrease formation of antibodies and T cells o Various drugs that have toxic effect on lymphoid system and therefore block formation of antibodies and T cells (like drug azathioprine) o Cyclosporine – has specific inhibitory effect on formation of helper T cells and therefore is especially efficacious in blocking T cell rejection reaction – one of most valuable of all drugs because it doesn’t depress some other portions of immune system o Use of immunosuppressants leaves person unprotected from infectious disease, and sometimes bacterial and viral infections become rampant o Incidence of cancer several times as great in immunosuppressed person because immune system important in destroying many early cancer cells before they begin to proliferate o With introduction of improved immunosuppressive agents, successful organ transplantation has become much more common o Current approach to immunosuppressive therapy attempts to balance acceptable rates of rejection with moderation in adverse effects of immunosuppressive drugs