Physiology Ch. 35 p445-450 [4-25
advertisement
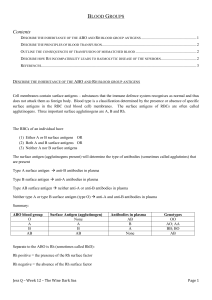
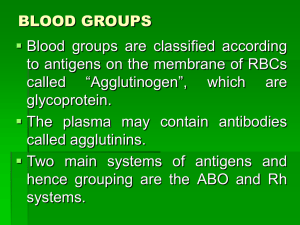
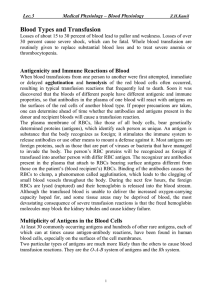
Physiology Ch. 35 p445-450 Blood Types; Transfusion; Tissue and Organ transplantation O-A-B Blood Types – two antigens, A and B occur on the membranes RBCs in many humans and are called agglutinogens that cause many blood transfusion reaction -When neither A nor B is present, the blood type is type O -When only A is present, it is type A, when only B is present, it is type B -When both A and be are present, blood is type AB -Two alleles on both chromosomes determine O-A-B blood type, and type O gene is functionless or almost functionless that causes no type O agglutinogen on the cells -Six combinations of genes are OO, OA, OB, AA, BB, and AB called genotypes -Most frequent blood type among group of people is type O (47%), while the second is type A (47%). Type B is 9% and Type AB is 3% Agglutinins – when type A agglutinogen is not present in a person, antibodies known as anti-A agglutinins are present in that person’s plasma. Same when type B agglutinogen is not present, anti-B agglutinins are present in plasma -For type O blood, there are no agglutinogens, but both anti-A and anti-B agglutinins are present -Type AB blood has no agglutinins Titer of Agglutinins at Different Ages – right after birth, quantity of agglutinin is near 0 and the infant only begins to produce those 2-8 months after birth -There are much more Anti-A agglutinins in type B and O blood than Anti-B agglutinins in type A and O blood Origin of Agglutinins – the agglutinins are gamma globulins (antibodies) produced in the bone marrow and lymph cells, and are mostly IgM and IgG -people produce agglutinins to agglutinogens they don’t possess because small amounts of type A and B antigens enter body in food, bacteria, and other ways to initiate development of those agglutinins Agglutination Process in Transfusion Reaction – when bloods are mismatched and anti-A or B agglutinins are mixed with RBCs containing A or B agglutinogens, the RBC’s agglutinate as a result of agglutinins attaching themselves to RBC -single agglutinin can bind 2 (IgG) or 10 (IgM) RBCs at the same time to cause them to clump and clog blood vessels -phagocytic WBC destroy membranes of agglutinated cells and release hemoglobin into plasma, called hemolysis Acute Hemolysis Occurs in Some Transfusion Reactions – when donor and recipient are mismatched, immediate hemolysis of RBC can occur because antibodies will cause activation of the complement system, which releases proteolytic enzymes to rupture RBC membrane -immediate hemolysis is less common than delayed hemolysis -immediate hemolysis requires IgM antibodies called hemolysins Blood Typing – determining blood type of individual. Performed by separating RBC from plasma and diluting with saline -One portion is mixed with anti-A agglutinin and another portion with anti-B agglutinin and then observed under a microscope and watched for clumping Rh Blood Types – Rh system is also important and transfusing blood, big difference to O-A-B system -O-A-B system has plasma agglutinins responsible for causing transfusion reactions to happen spontaneously -Rh system does not have spontaneous agglutinins ever occur, instead, a person must have massive exposure to Rh antigen before enough agglutinins develop to cause significant reaction Rh Antigens- Rh-positive and Negative People – there are 6 common Rh antigens, each called Rh factor These types are designated as C, D, E, c, d, and e. -A person who has a C antigen does not have the c antigen, but the person missing the C antigen always has the c antigen -The same is true for D-d antigens and E-e antigens -Type D is widely prevalent and more antigenic than other Rh antigens -Anyone with Type D antigen is considered Rh Positive and if they do not have type D antigen, they are considered Rh negative -even in people with other Rh antigens, they can still cause transfusion reactions, just milder -85% of white people are Rh positive and 15% Rh negative -95% of black americans are Rh positive, and 100% of African blacks are Rh positive Rh Immune Response – when RBC containing Rh factor injected into a person without that Rh factor, anti-Rh agglutinins develop slowly and reach maximum concentration 2-4 months afterwards, and the sensitivity increases with multiple exposures to the Rh antigen -if an Rh negative person has never been exposed to Rh positive blood, transfusion into that person will likely not cause an immediate reaction, however, anti-Rh antibodies can develop within 2-4 weeks to cause agglutination of those cells still circulating and are later hemolyzed by tissue macrophages -Thus, a delayed transfusion reaction occurs, but it is mild -Second transfusion will cause greatly enhanced response since they are already immunized Erythroblastosis Fetalis (Hemolytic disease of newborn) – disease of the fetus characterized by agglutination and phagocytosis of fetus’s RBCs, where mother is Rh negative and father is Rh positive and mother develops anti-Rh agglutinins from exposure to fetus’s Rh antigen such that mother’s agglutinins diffuse through placenta into fetus to cause agglutination -An Rh-negative mother having her first Rh-positive child does not develop sufficient anti-Rh agglutinins to cause harm, but 3% of second Rh positive babies exhibit some erythroblastosis fetalis and 10% for third child -After anti-Rh antibodies have formed in mother, they diffuse through placental membrane to cause agglutination of blood and they then hemolyze to release hemoglobin into blood -fetal macrophages then convert hemoglobin into bilirubin to cause baby’s skin to turn yellow -the jaundiced, erythroblastotic baby is anemic at birth and the agglutinins from mother circulate in baby for 1-2 months after birth -liver and spleen become enlarged and produce RBC same way they do during middle of gestation -many early, nucleated forms of RBC pass from bone marrow into circulatory system, and the presence of these cells in blood is called erythroblastosis fetalis -anemia is major cause of death, but survivors exhibit mental impairment and motor damage due to precipitation of bilirubin in neuronal cells, called kernicterus -Treatment for this is to replace neonates blood with Rh-negative blood for many times during first weeks of life to keep bilirubin low -prevention of erythroblastosis fetalis can happen with development of Rh immunoglobulin globin, and anti-D antibody administered to expectant mother -Anti-D antibody inhibits antigen-induced B lymphocyte antibody production -antibody also attaches to D-antigen sites on Rh-positive fetal RBC and interfering with D antigen Transfusion Reactions Resulting from Mismatched Blood Types – if donor and recipient blood is different, transfusion reaction is likely to occur in which RBC of the DONOR are agglutinated and not the recipient’s RBC because plasma portion of the donor gets immediately diluted by plasma of recipient to decrease the titer of the infused agglutinins to a low level -jaundice does not appear in adult transfusion reaction unless more than 400mL of blood is hemolyzed in less than 1 day Acute Kidney Shutdown After Transfusion – most lethal effects of transfusion reactions is KIDNEY FAILURE, which begins minutes to hours afterwards and continues until death Shutdown of kidneys results from 3 causes 1. Antigen-antibody reaction of reaction releases toxic substances from hemolyzing blood that cause renal vasoconstriction 2. Loss of circulating RBC along with toxic substances from hemolyzed cells cause circulatory shock, arterial BP falls low and renal blood flow/urine outpu decreases 3. If total free hemoglobin released is greater than quantity that can bind to haptoglobin, much of the excess leaks through glomerular membranes into kidney tubules and can precipitate to cause blockage and acute renal shutdown Transplantation of Tissues and Organs – most antigens of RBC also present on other organs, and each tissue has its own additional antigens that can produce immune reaction in another individual -transplant of tissue or whole organ from one part of animal to another part of same animal is called autograft. -from one identical twin to another is called isograft -from one human to another of the same species is called allograft -from one animal to one of a different species is called a xenograft Transplantation of Cellular Tissues – in autografts and isografts, cells in transplant contain same antigens as the tissues of recipient and will live normally if blood supply is provided -in xenografts, immune reactions almost always occur unless suppressive immune therapy is given -some different tissues and organs have been transplanted as allografts from one person to another – skin, heart, liver, bone marrow, lung with proper matching, successful kidney allografts survive for 515 years, and heart and liver survive for 1-15 years Tissue Typing, Human Leukocyte Antigen (HLA) Complex of Antigens – most important antigens responsible for graft rejection is a complex of HLA antigens, 6 of which are present on tissue membranes of each person, but there are 150 to choose from, so it is impossible for 2 people to have the same six HLA antigens, and immunity will cause graft rejection -HLC antigens occur on WBC and on tissue cells, therefore tissue typing is done on membranes of lymphocytes separated form blood Prevention of Graft Rejection by Suppressing Immune System – successful grafts can be performed if we suppress the immune system with the following agents: 1. Glucocorticoid hormones isolated from adrenal cortex glands which suppress growth of lymphoid tissue to decrease antibodies/T cells 2. Drugs that have toxic effect on lymphoid system, such as azathioprine 3. Cyclosporine – specific inhibitory effect on formation of helper T cells and therefore efficacious in blocking T cell rejection reaction. Proven to be most valuable of all other drugs because it DOES NOT depress other parts of immune system -use of these agents leaves person unprotected from infectious disease, and viral infections become rampant -Incidence of cancer increases several times because the immune system is important in destroying early cancer cells before they proliferate